HealthManagement, Volume 23 - Issue 6, 2023
Interoperability outcomes in healthcare refer to improving patient care, reducing medical errors, and increasing efficiency in healthcare delivery by enhancing the necessary coordination of all the agents involved.
Key Points
- Interoperability oriented towards care continuity.
- Empowerment of the patient over their clinical information.
- Greater visibility and transparency about the results of the clinical practice.
- Optimising the available resources for the benefit of the patient and population health.
- Improving the coordination of care.
- The critical impact of interoperability on medical outcomes.
Introduction
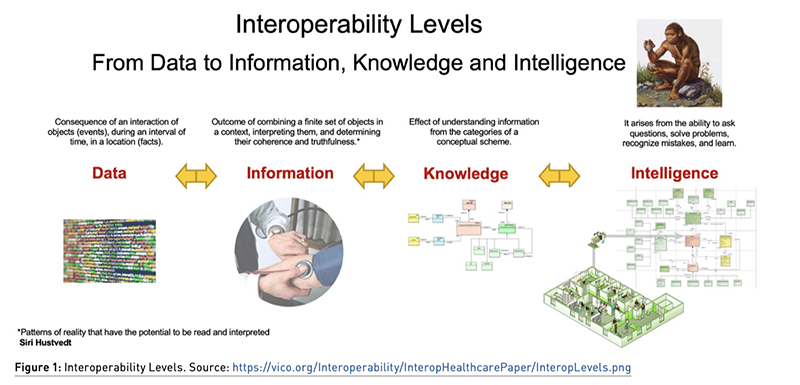
Interoperability implies data, information, knowledge and intelligence exchange, including their free usability between a range of components from several different technologies, based on open standards, plainly defined, and subject to transparent conformance of their structure and algorithms. A broader definition takes into account organisational factors that impact system-to-system business process performance. When a vendor is forced to adapt its system to a dominant system that is not based on open standards, we are talking about compatibility, not interoperability. Types of interoperability include syntactic level, where several systems can communicate with each other, and semantic cross-domain level, where multiple organisations work together and exchange information assets based on a shared reference information model.
Interoperability outcomes in healthcare refer to improving patient care, reducing medical errors, and increasing efficiency in healthcare delivery. Interoperability allows healthcare providers to access patient data regardless of the system or platform where the data is stored. This means that a patient’s electronic health record (EHR) can be accessed by different healthcare providers and systems, such as hospitals, clinics, and pharmacies, in order to provide coordinated care and continuity of the care process. However, achieving interoperability in healthcare can be challenging due to a variety of factors, such as multiple healthcare organisations involved, differences in data and terminology standards, the multiplicity of regulatory concerns on privacy, and technical limitations on coexistence between legacy and new systems. Efforts to improve healthcare interoperability are ongoing and involve collaboration between healthcare providers (public and private entities), government agencies, research institutions, and technology vendors.
Why Healthcare Interoperability
By “health system”, we mean a network of organisations that brings together people, institutions and resources. Its mission is to provide services aimed at meeting the health needs of citizens and a target population. Its rules act on the basis of fair conditions and respect for people’s dignity, with sustainable funding and accountability for the results of their actions.
The health organisation is a space of collaboration where several agents share the responsibility of solving, maintaining and improving the functional state of health and the quality of life of the citizens. These tasks require an organisational structure that is sustainable with a risk, quality and cost that we must manage and measure.
We will fulfil these requirements effectively only if we share standardised clinical information through the care processes and if we apply an interoperability scheme oriented towards care continuity and the empowerment of the patient over his clinical information. Both actions generate greater visibility and transparency about the results of the clinical practice of our professionals and help to optimise the available resources for the benefit of the Patient and Population’s health.
Let’s review the main agents involved in the delivery of healthcare services in a health system. Here are some examples:
- Physicians: Doctors who diagnose and treat illnesses, injuries, and diseases.
- Nurses: Healthcare professionals who provide patient care and assist physicians in medical procedures.
- Pharmacists: Healthcare professionals who dispense medications and provide drug information to patients and healthcare providers.
- Allied health professionals: These include a variety of healthcare professionals who work in fields such as physical therapy, occupational therapy, speech therapy, respiratory therapy, and radiology.
- Health administrators: These are the people who manage healthcare facilities, such as hospitals and clinics.
- Health educators: These are professionals who provide education and information to patients and the general public about various health issues and disease prevention.
- Medical researchers: These are scientists who conduct research to develop new treatments and cures for diseases.
- Health insurers: These are organisations that provide insurance coverage for healthcare services.
- Government agencies: These are entities that regulate and oversee healthcare services, such as pharmacovigilance management and health programmes.
- Patients: We consider that patients themselves are healthcare agents, as they play a role of greater empowerment in their own healthcare and treatment decisions.
In the context of healthcare, interoperability has a significant impact on medical outcomes by improving the necessary coordination of all the agents involved:
- Improved coordination of care: When different healthcare providers and systems can exchange patient data easily, it can improve the coordination of care. The lack of clinical information sharing kills more than the improper access to medical data.
- More accurate diagnosis and treatment: Interoperability can enable healthcare providers to access a patient’s complete medical history, including information from different providers and systems. This can help providers make more accurate diagnoses and develop more effective treatment plans.
- Reduced errors: Interoperability can reduce errors that occur when information is not shared or is shared inaccurately. For example, a pharmacist can access a patient’s medication history from different providers and systems, which can help prevent adverse drug interactions or duplicative prescriptions.
- Better patient engagement: Interoperability can improve patient engagement by allowing patients to access their own health information from different providers and systems. Patients could check their medical information available, and they could also act as a controller of the quality of the clinical sources and detect potential misunderstandings that affect their healthcare process.
Standards Portfolio
We have different sorts of organisations with complementary accountability. For example, HL7 International (Health Level Seven) is a “Standards Development Organisation” (SDO) for the field of health. Founded in 1987, their standards have been accredited by ANSI and ISO. It operates internationally, and its mission is to provide global information standards for clinical practice, healthcare organisations, administration and logistics to achieve real interoperability between the different information systems and technology applied in selected healthcare domains. On the other side, IHE (Integrating the Healthcare Enterprise) is a “Standards Implementing Organisation” (SIO), an initiative that aims to improve the interoperability of healthcare information systems. It defines a set of standards and implementation guidelines for the exchange of health information that can be tested in a real-time context to prove their efficacy and correct alignment with stakeholder requisites (Rules of Conformance).
To best understand how the information standards thrive inside the healthcare ecosystem, we share a reading of a conceptual model (Figure 4).
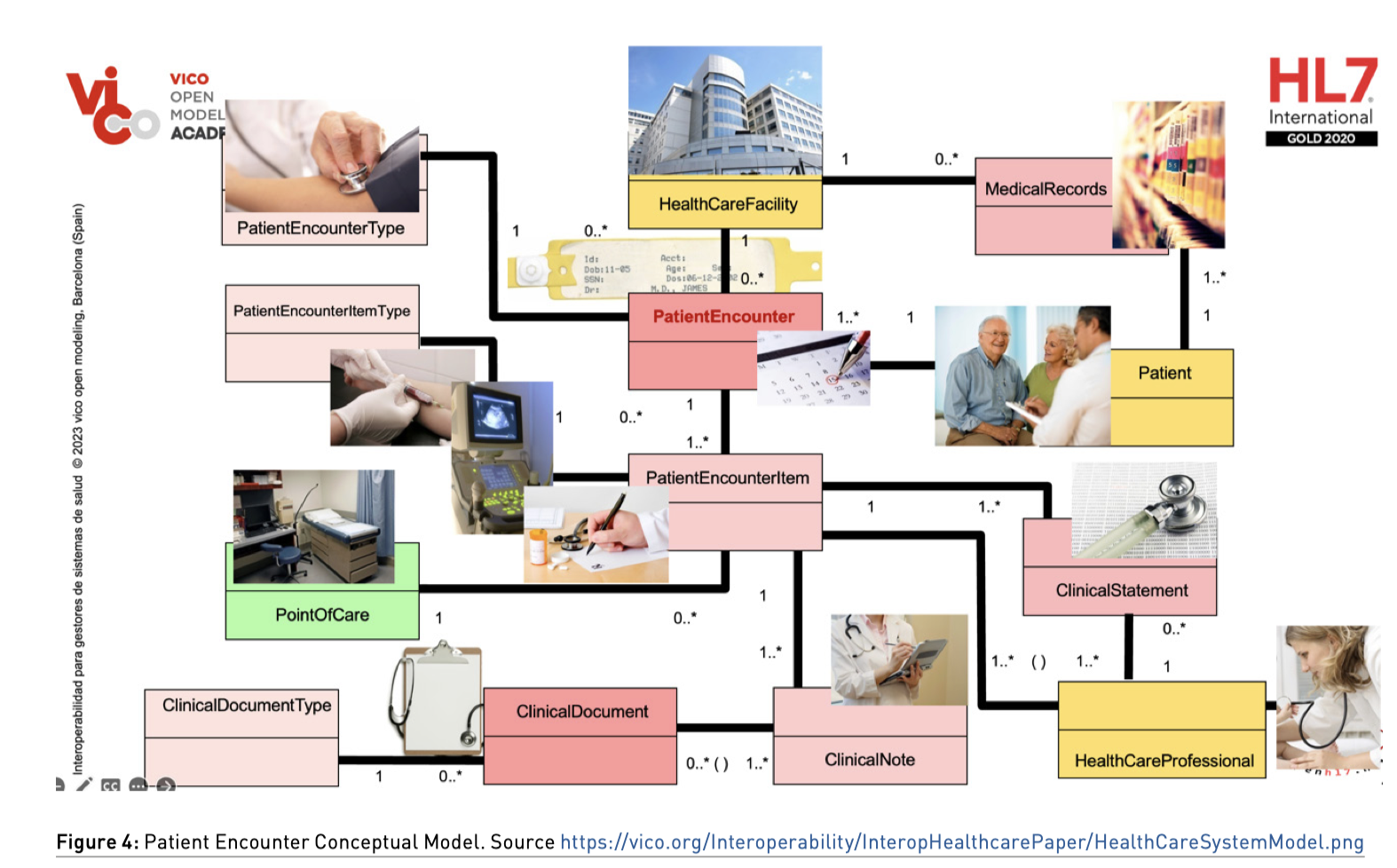
By convention, we have rendered the main process in the middle of the model. The background colour of the concept means a stereotype of the process corresponding to a patient encounter. The primary goal of each encounter is to provide appropriate care, address the patient’s needs, and improve their overall health outcomes.
A patient encounter refers to any interaction or meeting between a healthcare provider and a patient. It involves the exchange of information, assessment of the patient’s condition, and the delivery of healthcare services. Patient encounters can take place in various healthcare settings, such as hospitals, clinics, doctor’s offices, emergency rooms, or even through telemedicine platforms.
During a patient encounter, healthcare providers aim to gather relevant information about the patient’s medical history, current symptoms, and concerns. They may perform physical examinations, order diagnostic tests, prescribe medications, provide treatments, or offer counselling and education regarding the patient’s condition. The specific nature and depth of the encounter depend on the purpose, urgency, and complexity of the patient’s situation.
Reading the model, we can represent the diverse range of patient encounters that can occur across different healthcare settings and specialties (longitudinal register) and establish the following business rules through the different relationships between concepts (cardinality):
- All patient encounters must be performed in one healthcare facility (the salmon colour of the concept implies that it is a process, and the yellow colour of the facility means the role of an entity healthcare organisation, with requisites and constraints associated).
- The healthcare facility could house none or several patient encounters.
- Every patient encounter must indicate their patient encounter type (see the examples of patient encounters above).
- The patient encounter type could define none or several patient encounters.
- All patient encounters must contain one or more activities detailed as patient encounter items.
- Every patient encounter item belongs to a patient encounter.
- Every patient encounter item must indicate their patient encounter item type (see the examples of patient encounters above).
- The patient encounter item type could define none or several patient encounter items.
- All patient encounters are referred to one patient.
- Every patient must have one or more patient encounters (The yellow colour of the concept means the role of an entity person, with requisites and constraints associated).
- Every patient must have one or more entries in their medical record.
- The medical record belongs to one patient.
- The medical record must be custodied by a healthcare facility (on behalf of a healthcare organisation).
- A healthcare facility could have custody of none or several medical records.
- Every patient encounter item must be performed in a point of care (the green colour of the concept implies a concrete ubication of the healthcare facility with requisites and constraints associated).
- The point of care could house none or several patient encounter items.
- Every patient encounter item must generate one or more clinical statements (we’ll explain this concept below).
- Every clinical statement must be associated with a patient encounter item.
- Every clinical statement must be authored by one healthcare professional.
- A healthcare professional could be the author of none or several clinical statements (The yellow colour of the concept means the role of an entity person, with requisites and constraints associated).
- A healthcare professional must record their clinical statements in one or more clinical notes.
- Every clinical note must be authored by one or more healthcare professionals.
- A clinical document must gather one or more clinical notes.
- A clinical note could be gathered in none or several clinical documents.
- Every clinical document must indicate its clinical document type and a clinical document type could define none or several clinical documents.
About Clinical Statements
Clinical statements capture key information about the patient’s condition, allowing healthcare professionals to make informed decisions and provide appropriate care.
A clinical statement refers to a concise and structured piece of information that describes a patient’s health status, medical condition, diagnosis, treatment, or any other relevant clinical details. Clinical statements are commonly used in healthcare settings to document patient encounters, communicate information among healthcare professionals, and ensure accurate and standardised documentation for medical records.
Clinical statements typically follow a specific format and include essential elements such as:
- Patient identification.
- Date and time when the statement was documented or when the relevant clinical event occurred.
- Clinical context: Provides an overview of the patient’s medical history, presenting problem, or reason for the statement.
- Objective findings: Are factual and observable information gathered through physical examinations, laboratory tests, imaging studies, or other diagnostic procedures.
- Subjective information: Includes the patient’s self-reported symptoms, complaints, or other relevant information shared during the encounter.
- Assessment and diagnosis: The healthcare professional’s evaluation and determination of the patient’s medical conditions based on the presented information.
- Treatment plan: Outlines the recommended interventions, therapies, medications, or procedures for managing the patient’s condition.
- Prognosis: An estimation of the expected course and outcome of the patient’s condition or disease.
Clinical information standards are centred on electronic data interchange, clinical document sharing, interoperability artefacts, and the platforms that manage exchange and communication.
It’s very important not to confuse the levels of accountability that conditions every information standard. In our model, we’ll solve the different interoperability scenarios with data, documents, and messages to fulfil the requisites of the sender and receiver on their electronic data interchange and documents to share the Clinical Statements authored by Healthcare Professionals.
Data interchange doesn’t need a context or an author, but clinical documents are fully constrained by a context, by one or more authors of the content, a legal authenticator of the clinical statements, and a healthcare organisation that must act as a custody of the documents by law.
Please remember that an Electronic Health Record is a “Clinical Document Related Group” (not a simple clinical data gathering), and each clinical document is:
- An act of clinical knowledge.
- A clinical statement about the functional health status of a patient
- A collaboration tool between health professionals and communication with the patient.
Scenarios, Actors and Transactions
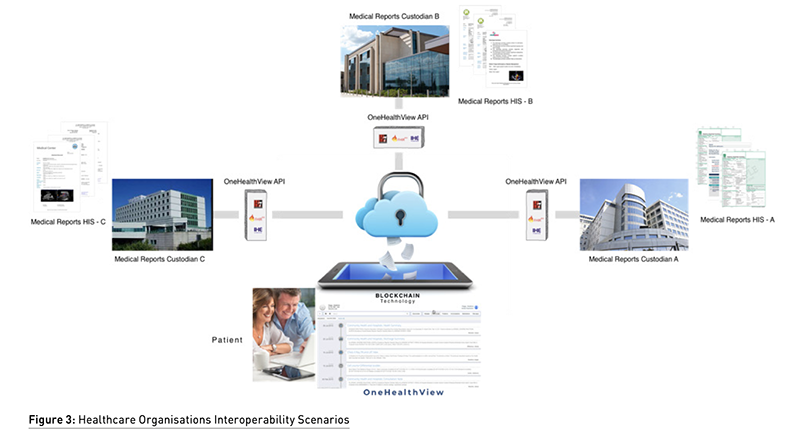
Interoperability scenario refers to a situation or context where multiple systems, devices, or software applications are able to work together and exchange information seamlessly. It involves the ability of different components or entities to communicate, interact, and share data effectively, despite being developed independently by different vendors or organisations. When we talk about interoperability Use Cases (UC), we understand that each UC is a package that contains one or more scenarios. The exact number of contained scenarios depends on our UC granularity criteria.
In an interoperability scenario, the various systems involved should be able to understand and interpret the data and commands shared between them, regardless of their underlying technologies, protocols, or standards. This enables them to collaborate and achieve common goals without encountering compatibility issues or barriers.
Interoperability scenarios can occur in various domains of healthcare, for example, allowing different electronic health record (EHR) systems to exchange patient data securely and accurately, enabling healthcare providers to access comprehensive medical information regardless of the system they use.
IHE (Integrated Healthcare Enterprise) is our best reference for specifying scenarios with actors and transactions. It will be useful to browse the contents of the ATNA (Audit Trail and Node Authentication) infrastructure profile to learn, with examples, the relevance of identifying actors and transactions when we define an interoperability scenario.
One of the key concepts in IHE is the notion of actors and transactions. An actor is a functional component within a healthcare information system that plays a specific role in the exchange of health information. A transaction is a specific type of exchange that occurs between two actors, is implemented by interoperability artefacts and is managed by interoperability platforms.
Transactions are specific types of exchanges that occur between actors. For example, one common transaction in the IHE framework is the Patient Identifier Cross-Reference (PIX) transaction, which is used to query a cross-reference of patient identifiers maintained by the PIX actor. Another example is the Retrieve Imaging Information (RII) transaction, which is used to retrieve information about medical images stored in an Image Archive (IA) actor. The concept of actors and transactions is a key part of the IHE framework, and understanding these concepts is essential for building interoperable healthcare information systems that can exchange information seamlessly across different applications and systems. For example, between a PACS (Picture Archiving and Communication System) and a DACS (Document Archiving and Communication System).
About Interoperability Artefacts
We consider the interoperability artefacts as a set of tools, standards, and guidelines used to ensure that different systems, applications, and devices can work together seamlessly. These artefacts are essential in achieving interoperability. Some examples of interoperability artefacts include:
- Application Programming Interfaces (APIs): These are sets of protocols, routines, and tools used by developers to build software applications. APIs allow different applications to communicate and exchange data with each other. FHIR® is the most recent example of success in healthcare interoperability.
- Data and Document exchange formats: These are standardised formats for exchanging data and documents between different systems. Examples include XML, JSON, and CSV.
- Standards and protocols: These are guidelines and rules that ensure that different systems can communicate with each other effectively. Examples include HTTP, TCP/IP, and LDAP.
- Middleware: This is software that acts as a bridge between different systems and applications. Middleware can translate between different protocols, data formats, and APIs, enabling interoperability between different systems.
About Interoperability Middleware
Enterprise Service Bus (ESB) and Message-Oriented Middleware (MOM) are technologies used for asynchronous communication between different systems or components. However, they have significant differences that we must take into consideration if we are facing complex scenarios where a choreography of processes or fault-exception rules are needed.
ESB is a cloud-based messaging service and process manager that enables communication between different applications and services in the cloud or on-premises. It offers a reliable and scalable platform that supports multiple protocols, message patterns and Business Process Execution Language (BPEL) services. On the other hand, MOM is a middleware technology that enables communication between different applications or services using only messaging patterns. MOM is typically used in enterprise environments where different systems need to communicate with each other only through electronic data interchange.
We can find solutions to this kind of middleware, both open-source and freeware. For example, OpenESB provides a powerful and flexible platform for building and managing complex integration solutions that can help organisations streamline their business processes and improve overall efficiency. It is a Java-based enterprise service bus (ESB) that supports a platform for integrating enterprise applications and services.
Healthcare Decision-Makers View
Let me share some ideas on why decision-makers should embrace interoperability services in their healthcare domains. There are several compelling arguments that healthcare decision-makers can consider when it comes to adopting interoperability in healthcare systems.
- Enhanced Patient Care: Interoperability enables seamless sharing of patient health records and information across different healthcare providers, improving care coordination and patient outcomes. Access to comprehensive and up-to-date patient information allows healthcare professionals to make informed decisions and provide more personalised, timely, and effective treatments.
- Patient Safety and Reduced Errors: Interoperability helps prevent medical errors by ensuring an accurate and complete exchange of patient data, including medications, allergies, and medical history. Access to real-time patient information can help avoid duplicate tests, medication errors, and adverse drug interactions, ultimately improving patient safety.
- Increased Efficiency and Cost Savings: Interoperability streamlines workflows and reduces administrative burdens associated with manual data entry, paperwork, and faxing. It improves operational efficiency by eliminating redundant processes and automating data exchange, which saves time and reduces costs for healthcare organisations.
- Improved Population Health Management: Interoperability enables comprehensive data aggregation and analysis, which supports population health management initiatives. By having access to integrated patient data, healthcare decision-makers can identify trends, monitor health outcomes, and proactively address public health concerns such as disease outbreaks, chronic disease management, and preventive care strategies.
- Empowered Patient Engagement: Interoperability promotes patient engagement by allowing individuals to access and control their health information securely. Patients can actively participate in their care decisions, access their medical records, and share information with other providers. This engagement leads to increased patient satisfaction and better health outcomes.
- Research and Innovation: Interoperability facilitates data and document sharing for research purposes, enabling large-scale analysis and the discovery of new insights. With interoperable systems, decision-makers can leverage big data analytics, machine learning, and artificial intelligence to drive research, develop innovative treatments, and advance medical knowledge.
- Regulatory Compliance and Incentives: Many countries are enacting regulations and policies that promote interoperability as a means to improve healthcare outcomes. Adopting interoperable systems ensures compliance with these regulations and opens up opportunities for healthcare organisations to qualify for incentive programmes and funding related to interoperability implementation.
- Collaboration and Continuity of Care: Interoperability allows for seamless communication and collaboration between healthcare providers, promoting a continuum of care. Sharing patient data across different care settings, such as hospitals, clinics, and long-term care facilities, enables care teams to work together effectively, reducing gaps in care and ensuring smoother transitions for patients.
By embracing interoperability, healthcare decision-makers can unlock the potential for better patient care, improved efficiency, and transformative advancements in healthcare delivery, ultimately leading to better health outcomes for individuals and populations as a whole.
Again, the most appropriate starting point for a decision-maker is the review of the implementation guides published by IHE. The guides represent a distillation of interoperability best practices, and the events organised under the heading of “connectathon” are a very valuable source of reference for knowing the level of quality of technology providers in the health systems market and to what extent they are in compliance with the most accredited clinical information standards.
It is also highly recommended to follow up on the market showcases. An interoperability showcase is an event or demonstration that highlights the ability of different systems, technologies, or platforms to work together seamlessly and exchange information effectively. It aims to showcase how different components, devices, or software can communicate and interact with each other, even if they are developed by different vendors or utilise different standards. Interoperability showcases are commonly organised in the technology industry to promote collaboration, innovation, and compatibility among various products or solutions. These showcases often involve live demonstrations or simulations where different systems or products are integrated to demonstrate their interoperability capabilities. The main goals of an interoperability showcase are:
- Compatibility: To demonstrate that different systems or technologies can work together and exchange data without any issues, regardless of their underlying specifications or protocols.
- Collaboration: To encourage collaboration among different vendors, developers, or organisations by showcasing how their products can integrate and complement each other to provide enhanced functionalities or services.
- Standardisation: To promote the adoption of common standards, protocols, or frameworks that facilitate interoperability and create a unified ecosystem where various technologies can seamlessly interact.
- Innovation: To inspire innovation by showcasing how interoperability can enable the development of new applications, services, or solutions that leverage the strengths of multiple systems or technologies.
Interoperability showcases are often organised by industry associations (HIMSS), technology consortia, or standards organisations. They provide a platform for companies to demonstrate their products or solutions to potential customers, partners, or stakeholders, fostering collaboration and driving the adoption of interoperable technologies. These showcases can cover various domains, such as healthcare, telecommunications, smart cities, Internet of Things (IoT), financial services, and more. They may focus on specific interoperability standards or technologies, or they can have a broader scope to encompass multiple areas. Interoperability showcases play a crucial role in promoting compatibility and collaboration within the technology industry, ultimately leading to more integrated and interconnected systems that benefit end-users and drive technological advancements.
Patient: A New Interoperability Actor
Patient engagement plays a crucial role in achieving interoperability in healthcare. By involving patients in their own care and empowering them to access and share their health information, interoperability can be enhanced, leading to improved healthcare outcomes. Here are some use cases that demonstrate how patient engagement can promote interoperability:
- Personal Health Records (PHRs): Patients can maintain their own PHRs, which consolidate their medical information from various healthcare providers. By actively updating their records, patients ensure that their health information is accurate and up to date. PHRs can be accessed by different healthcare providers, facilitating interoperability and seamless information exchange.
- Patient Access to Health Information: Patients can be given access to their electronic health records (EHRs) through secure patient portals. This allows them to review their medical history, test results, diagnoses, and treatment plans. By having access to their own health information, patients can actively participate in care decisions, seek second opinions, and share the information with other healthcare providers as needed.
- Patient-Generated Health Data (PGHD): Patients can collect and contribute their health data using wearable devices, mobile apps, or other monitoring tools. This includes information such as activity levels, heart rate, blood pressure, sleep patterns, and more. Integrating PGHD with EHRs allows healthcare providers to have a comprehensive view of patients’ health, enabling better-informed decisions and personalised care plans.
- Appointment Scheduling and Reminders: Patient engagement can be enhanced through interoperable systems that enable online appointment scheduling and automated reminders. This helps patients stay informed about their upcoming appointments, reduces no-show rates, and improves overall care coordination.
- Secure Messaging and Telehealth: Interoperable messaging platforms and telehealth solutions enable patients to communicate securely with their healthcare providers. Patients can ask questions, discuss concerns, share updates, and receive guidance remotely. By facilitating these interactions, interoperability supports patient engagement and strengthens the patient-provider relationship.
- Medication Management: Interoperable systems can integrate medication lists, prescription history, and medication adherence data. Patients can access this information to ensure they are following the prescribed treatment plan correctly. Interoperability enables medication reconciliation during care transitions, preventing errors and promoting patient safety.
- Health Education and Decision Support: Interoperable health information systems can deliver personalised educational resources and decision-support tools to patients. These resources can help patients understand their conditions, treatment options, and potential risks. By being well-informed, patients can actively participate in shared decision-making with their healthcare providers.
By leveraging patient engagement and interoperability, healthcare organisations can create a more patient-centred and collaborative care environment. These use cases foster information exchange, enable better care coordination and empower patients to take an active role in their own health management.
Blue Button is a healthcare industry initiative that provides patients with secure and easy access to their personal health information. It allows patients to download and share their health data with healthcare providers, family members, or other authorised individuals. The Blue Button was initially launched by the U.S. Department of Veterans Affairs (VA) in 2010 and has since been adopted by several other healthcare organisations, and many private and public health plans.
The Blue Button is typically accessible through a patient portal or mobile app and allows patients to download their health records in a standardised format, such as PDF, XML, or JSON. This data can include information on medications, allergies, lab results, immunisations, and other clinical data. The Blue Button initiative aims to empower patients to take control of their healthcare by giving them greater access to their health information and promoting interoperability and data sharing among healthcare providers. By making it easier for patients to access and share their health data, the Blue Button can help improve the quality and coordination of care, reduce medical errors, and enable patients to make more informed healthcare decisions.
Another initiative that will trigger a breakthrough in patient empowerment is The European Health Data Space (EHDS). It is an initiative of the European Union (EU) aimed at facilitating the secure exchange and sharing of health data across borders within the EU. It is part of the broader European Commission’s Data Strategy, which aims to unlock the potential of data-driven technologies and services while protecting individual privacy and ensuring the highest standards of security.
The EHDS seeks to address challenges related to fragmented health data systems and data silos across European countries. It aims to enable healthcare providers, researchers, and innovators to access and use health data more effectively and efficiently for the purposes of research, innovation, and improving healthcare outcomes.
Key objectives of the EHDS include:
- Interoperability and standardisation: Promoting the adoption of common technical and semantic standards to ensure that health data can be exchanged and understood across different systems and countries.
- Data governance: Establishing a framework for data governance that defines the rights, responsibilities, and accountability of all stakeholders involved in the sharing and use of health data while respecting individual privacy and data protection laws.
- Data quality and integrity: Ensuring the quality, reliability, and integrity of health data shared within the EHDS to support evidence-based decision-making and research.
- Access and reuse of health data: Facilitating secure access to health data for authorised users, such as healthcare professionals, researchers, and innovators, while implementing stringent privacy and security measures.
- Citizen empowerment: Empowering individuals to have more control over their health data through mechanisms such as consent management, allowing them to actively participate in data-sharing decisions and benefit from innovative healthcare solutions.
The EHDS aims to promote cross-border collaboration, accelerate medical research, foster innovation, and enhance healthcare delivery by leveraging the vast amount of health data available across the EU. It also seeks to address ethical, legal, and technical challenges associated with data sharing, ensuring that privacy and data protection rights are upheld.
The implementation of the EHDS involves close collaboration between EU member states, relevant stakeholders, and the European Commission. It builds upon existing initiatives and regulations, such as the General Data Protection Regulation (GDPR) and the EU’s Electronic Health Record Exchange Format, while seeking to harmonise standards and practices across different countries.
In Catalonia, the Healthcare Department has recently implemented a joint service of Blue Button and European Health Data Space rules, focused on sharing clinical documents and generating European patient summaries from a DACS (Document Archiving and Communication System) through a Patient Portal “La Meva Salut” (My Health). Empowered patients can now download all their medical reports and patient summaries on their mobile devices and share them with research institutions in a collaborative effort with non-governmental organisations like Salus-Coop.
Interoperability Pitfalls and Evolution
Current prevalent standards are evolving without any intention of unifying their artefacts. It is missed that the ambitious UMLS initiative regarding the mapping and harmonisation of all biomedical terminology standards, is not also applied with regard to the clinical information modelling standards.
FHIR® (Fast Healthcare Interoperability Resources) and openEHR (open Electronic Health Record) are two prevalent standards in the healthcare domain, specifically focusing on interoperability and electronic health records (EHRs). While they have similar goals, they approach interoperability and EHRs from different perspectives and have different design principles. Here’s an overview of the relationship between FHIR and openEHR:
Purpose and Scope
- FHIR: Is a standard developed by HL7 (Health Level Seven International) and aims to provide a framework for exchanging healthcare information electronically. It focuses on data exchange, allowing different healthcare systems to share information using a standardised set of resources and APIs.
- openEHR: Is an open standard developed by the openEHR Foundation. It aims to define a common information model and architecture for EHRs that support lifelong, shared healthcare records. openEHR focuses on creating semantically rich and computable EHRs with a strong emphasis on clinical content and decision support.
Data and Reference Information Models
- FHIR: Utilises a resource-based data model, where healthcare information is represented as discrete resources such as Patient, Observation, Medication, etc. These resources have predefined structures and can be exchanged using RESTful APIs and formats like JSON or XML.
- openEHR: Employs an archetype-based data model. It defines a set of archetypes that capture the clinical knowledge and semantics of various types of health data. These archetypes are used to create templates for capturing and storing EHR data. The templates can be customised to accommodate local requirements and are designed to be computable and interoperable.
Interoperability
- FHIR: Focuses on facilitating interoperability between different healthcare systems and applications. It provides a set of well-defined resources, standards, and APIs that allow for easy data exchange and integration. FHIR is widely used for implementing interoperability at the application level and enables plug-and-play integration of different healthcare systems.
- openEHR: Aims to achieve semantic interoperability by providing a standardised information model and clinical knowledge representation. It focuses on capturing structured and semantically rich EHR data that can be shared and processed by different systems. openEHR provides a foundation for creating interoperable EHRs with consistent clinical content and decision-support capabilities.
Relationship
FHIR and openEHR are not mutually exclusive and can complement each other in certain use cases. They can be used together to achieve comprehensive interoperability and EHR capabilities. For example:
- FHIR can be used as a transport mechanism for exchanging data between openEHR-based systems or as a mechanism to expose openEHR data to external applications.
- openEHR can provide the underlying information model and clinical content framework for storing and managing EHR data, while FHIR can provide the standardised APIs and resources for interoperability with other systems.
In summary, FHIR and openEHR have different approaches and design principles but share the common goal of improving interoperability and electronic health records. They can be used together to leverage the strengths of each standard and create comprehensive solutions for healthcare information exchange and EHR management.
Clinical intelligence (AI in the healthcare domain), thanks to global clinical information access through interoperability services and the application of public and transparent algorisms, must help to generate relevant and pertinent questions, and at the same time, it must answer the key questions that our daily clinical practice generates:
- How can I be thorough yet efficient in considering the possible causes of my patient’s problems?
- How do I rate the information I have gathered during the medical interview and physical examination?
- How do I interpret new information aimed at establishing a diagnosis?
- How do I select the most appropriate diagnostic examination?
- How do I choose between several alternatives on treatment with risk of error and harm to the patient?
- How can I improve my relationship and communication with the patient?
Acknowledgements
I am grateful to so many people for their support and their faith. Thanks to Dr Josep M. Picas, my colleague, for many years of work and learning. My partners at https://vico.org/ Martí Pàmies and Rafael Rosa (Interoperability Architects); Dr Jaime Delgado (UPC Cybersecurity Authority) at https://www.clinicaldocumentengineering.com/en and Dr Marc Carreras (UDG Research Group on Health Services and Health Outcomes), for their faculty and intelligence; Daniel Nebot and Diana Gómez for their valuable support at https://vicoacademy.com/; Rosa Barber from Servei Català de la Salut, for sharing her vision and initiatives and to all the reviewers of this paper.
Conflict of Interest
None.
References:
Benson T, Grieve G (2016) Principles of Health Interoperability: SNOMED CT HL7 and FHIR (Health Information Technology Standards). Springer.
Blois MS (1984) Information and Medicine. The Nature of Medical Descriptions. University of California Press. Berkeley.
Braunstein ML (2022) Health Informatics on FHIR: How HL7's API is Transforming Healthcare. Springer.
Oemig F, Snelick R (2016) Healthcare Interoperability Standards Compliance Handbook: Conformance and Testing of Healthcare Data Exchange Standards. Springer.
Trotter F, Uhlman D (2011) Hacking Healthcare: A Guide to Standards, Workflows, and Meaningful Use. O'Reilly Media.
Wager K, Lee A, Glaser FW, John P (2013) Health Care Information Systems: A Practical Approach for Health Care Management. Wiley.
Useful links
https://vico.org/hl7/AboutHL7/HL7_RepEstandares2022ca.pdf
https://vico.org/AOfertas/IHE_concepts2022ca.pdf
https://vico.org/HL7_RIM/index.html - foundation-classes
http://www.vico.org/CDA_explorer/examples/SampleCDADocument/visualizer.html
https://www.vico.org/CDAR22005_HL7SP/infrastructure/cda/SampleCDADocument.xml
https://www.clinicaldocumentengineering.com/CCDARenderingToolChallenge/SampleCDADocument.xml
https://vico.org/MeusPOSTERS/PostersIHE/ATNA/IHE_ATNA.pdf
https://vico.org/CDE/KeyNotes/CDE_OpenCDE_resum_eng.pdf
https://vico.org/COVID19/COVID19TestTrackTreat.pdf
https://www.vico.org/MeusPOSTERS/Posters%20OpenCDA/OpenCDA_concept.pdf
https://vico.org/mindray/MonitorCtesIntegracionEng.pdf
https://vico.org/aFHIRbest/ClinicalCondition/FHIR_ClinicalCondResources.pdf
https://vico.org/ClipsPerEnganxarMail/__Models_eHEALTH/ConfigProdSalud1.pdf
https://guarda.vico.org
https://www.vico.org/MeusPOSTERS/Posters%20OpenCDA/OpenCDA_Security.pdf
https://vico.org/vicoappGuarda/EPS_GUARDA.mp4
https://vico.org/Mobile/17.02.01mConnectCDEflyerEng.pdf
https://vico.org/CDE/KeyNotes/OpenCDE_KeyNotes1_XPAT2018_eng.pdf
https://vico.org/CDE/KeyNotes/OpenCDE_KeyNotes1_VIC2018_eng.pdf




















