ICU Management & Practice, Volume 24 - Issue 2, 2024
When the stakes are high, and the path ahead is uncertain, the decisions made, especially if a patient continues to worsen, can be sources of self-torment and can haunt us for a long time. Our goal is to suggest ways to steer decision-making for intensivists in the face of uncertainty by proposing a clear, practical, stepwise approach through the creation of a new algorithm that reflects our common goal in such situations, which is to STABILIZE our patients.
Introduction
An intensive care unit is a fast-paced, high-stakes environment in which patients with life-threatening illnesses require near-constant attention, especially when first admitted to prevent them from dying. Important decisions must be made quickly: ones that engage a complexity of inter-related issues, ones that trade-off benefits and undesired effects, ones that have irreversible consequences, and ones that must be made in the context of missing data and constant ambiguity. Often, significant aspects of the nature of the patient’s critical illness itself remain uncertain throughout their admission.
How Do We Make Decisions?
Making effective decisions is an essential quality for any medical leader. Almost unique to the intensity of critical care practice is the sheer number of decisions that must be made within short periods of time. Research shows that intensivists make more than 100 decisions/day, just during patient rounds alone (i.e. over a mean time of 3.7 hours), with more decisions being made for those more recently admitted, those seen earlier in the day, and by female intensivists (McKenzie et al. 2015; Dennis et al. 2023). This does not include the number of decisions made as new patients get admitted and as others deteriorate. This relentless need to make decisions is a critical aspect of training in critical care medicine and is one of the principal causes of the exhaustion of clinical practice.
Our approach to making decisions can be considered in two different psychological models: the normative and the descriptive models. Simplistically, a normative model describes how doctors should make decisions – using a rational or hypothetical-deductive cognitive process. Conversely, a descriptive model describes how we actually make decisions – using intuition and recognition-primed decision-making.
How We Should Make Decisions
Ideally, decision-making in the ICU should follow a hypothetical- deductive model. This is a rational approach in which hypotheses are formed from the patient’s history and physical examination, refined through confirmatory and eliminatory diagnostic testing, followed by simultaneous intervention and evaluation of response (Christenson et al 2022; Lighthall and Vazquez-Guillamet 2015). Also known as evidence-based reasoning, the generation of several hypotheses, or differential diagnoses, is fundamental to this process. Each hypothesis or diagnosis should have some sense of likelihood, such that each possibility is grounded in history, physical examination findings, and initial investigations.
How We Actually Make Decisions
In contrast, intuitive decision-making or recognition-primed approaches employ heuristics or shortcuts. The cognitive psychology literature suggests that we make 95% of our decisions in this way (Lakoff 1999). Known also as experience-based reasoning, the brain's automatic and initial response to what we see, hear, smell, etc., is to try to match it to a familiar pattern. In clinical medicine, one summons remembered experiences and understanding of similar presentations, missed diagnoses (ours and those of our colleagues), and even stories in the media (academic, social or otherwise). If these memories form a matching pattern, they become the basis of a healthcare provider’s decision-making – in ways that are almost certainly subconscious or automatic (Christenson et al. 2022; Lighthall and Vazquez-Guillamet 2015). For a highly pathognomonic case and for a clinician with significant experience, the diagnosis is likely to be correct. How often is this truly the case?
Impediments to Decision-Making and Bias
Both rational and intuitive decision-making may be used together in any given situation. Just because our intuition influences a decision does not mean that we cannot change it with rational, reflective thinking and metacognition. This executive override is vital as intuitive decision-making (and, to an extent, hypothetical- deductive) is subject to biases (i.e. likelihood and/or recall). This failure to consider and/or discount evidence that would point to a different diagnosis or a new issue (confirmation and/or anchoring bias) may result in overconfidence regarding the accuracy of the assessment of any given patient (Christenson et al. 2022; Lighthall and Vazquez-Guillamet 2015). A final and sometimes dangerous pitfall of decision-making is that of status quo biases or diagnostic momentum in which healthcare providers are more likely to not intervene or change the decision-making course once set (Christenson et al. 2022; Lighthall and Vazquez-Guillamet 2015). All of these challenges can, of course, lead to error events and less-than-ideal patient outcomes.
Managing Uncertainty
There are often many paths to stabilising critically ill patients and achieving good outcomes. Yet what happens when the road is not clear and when you aren't sure what to do next? Decisions must still be made, decisions to intervene either further or differently or decisions to give the patient more time, to wait and see if there is a delay in response, without any change in course within the treatment plan. Uncertainty is often lauded as a concept that stimulates creativity, leads to new scientific discoveries and promotes humility. Uncertainty, when the explanation for what is happening with a critically ill patient, when it’s unclear how to proceed, is distressing (Dunlop et al. 2020) and frankly isolating. Even if uncertainty is a common experience in the ICU, such uncertainty is arguably only really perceived by intensivists as a normal component of critical care medicine when it pertains to patient outcomes because of the severity of their illness and the understanding that unexpected events may occur as one navigates one’s way back to health. Otherwise, in a field built on the concepts of regaining and not losing control of severe illness, normalising physiology, paying attention to details, making difficult choices and decisions and living with each of our sickest patients, moment by moment, uncertainty is terrifying and may be paralysing.
In a thematic analysis, Helou et al. (2020) have sought to address uncertainty by emphasising the need to recognise it, classify the type of uncertainty, explore stakeholder (in particular patients’) perspectives and acquire knowledge while seeking to assess, synthesise and reflect on the impact of different perspectives and new information on its resolution and the ability to move forward in decision-making. Yet, in our opinion, these approaches do not provide a clear enough guide for intensivists struggling with uncertainty, whether diagnostic or treatment related—the causes of uncertainty are usually pretty clear, patients' values are usually known, or they (or their families) are unable to convey them, nor are they able to describe what they are experiencing and there are typically already a myriad of tests and results and a mass of information available. The issue is navigating through these chaotic situations.
Others have proposed the use of checklists, decision support tools, cognitive forcing strategies (self-reflection and monitoring during decision-making) and post hoc metacognitive strategies (e.g. morbidity and mortality rounds, critical incident reviews and root cause analysis) focusing on the potential for system failures to contribute to diagnostic failures, education on how decisions are made and group decision-making (Christenson et al. 2022). Christenson et al. (2022) also discuss relational reasoning, exploring concepts of analogy, anomaly, antimony and antithesis, vertical and horizontal tracing of inter-relationships of diagnosis and aetiologies and associated illnesses have the potential to mitigate bias and assist with decision-making although these strategies are not well studied in critical care. Yet, still, only some of these concepts provide the intensivist with guidance on how to move forward in the moments when facing uncertainty.
So what should happen when a patient is getting sicker, is barely hanging on, and you can't decide what to do? Our goal is to suggest ways to steer decision-making for intensivists in the face of uncertainty by proposing a clear, practical, stepwise approach, one that we have developed and honed based on self-reflection/ analysis of our own clinical practices and on dissection of our teachings to our critical care fellowship trainees in the University of Toronto, Canada. For ease of recall, we are suggesting the creation of a new algorithm that reflects our common goal in such situations, which is to STABILIZE our patients.
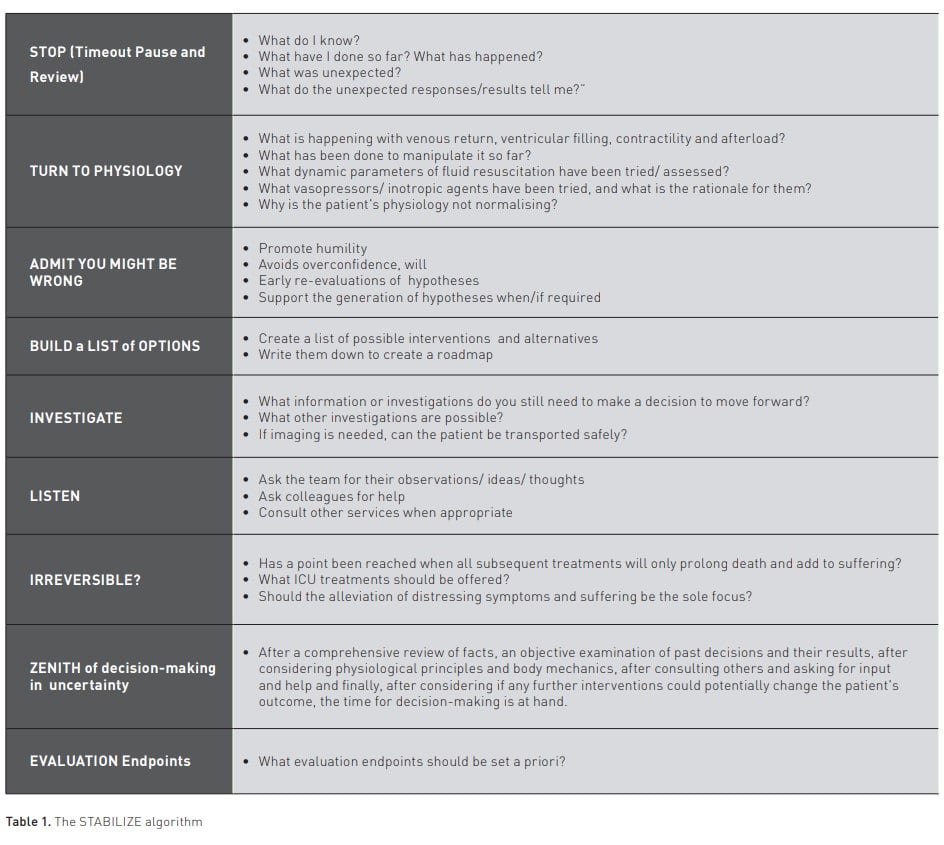
The STABILIZE Algorithm in Decision-Making Uncertainty
Stop and review
In the midst of an acute resuscitation, it can be challenging to find time to stop reacting and instead take time to think. Timeouts have been recognised as invaluable in improving patient safety and outcomes in many healthcare settings, such as the OR (Borchard et al. 2012; LoPresi et al. 2021; Papadakis et al. 2019), in medication administration (Mishima et al. 2023; Tainter et al. 2018), transfer of accountability, patient transport and around procedures such as intubation, post-intubation mechanical ventilation, central lines and lumbar punctures to name but a few. The same impact of timeouts can be true with respect to dealing with uncertainty, in particular when a patient is not responding as expected to resuscitation. Some of the most important questions that intensivists can/should ask themselves are aimed at re-examining the foundations on which they began their initial resuscitation plans. These foundations begin by returning and reviewing the initial history, physical exam and investigations. Questions such as ‘What do I know? What have I done so far? What has happened? What was unexpected? What do the unexpected responses/results reveal?" can help in developing a cold, hard look at the assumptions and available evidence. These questions integrate some of the concepts previously described (Christenson et al. 2022; Helou et al. 2020). Time pressures have been identified as barriers to implementing such diagnostic timeouts (Yale et al. 2022). Yet such a pause and review can assist in generating new hypotheses and/or identifying what is going wrong and perhaps open the door to answering the crucial questions of why and where we go from here.
Turn to physiology
The foundations of critical care medicine seek to understand, manipulate and normalise physiology. Understanding organ system interactions and responses to severe illness are the basic knowledge requirements to successfully resuscitate a person with a life-threatening illness. Importantly, while a lot of attention, research and guidance in critical care medicine has been paid to lung physiology and its interactions with mechanical ventilation, this is not the only physiology, nor, in a given patient, may it be the most important one at any given time. Nor does pulmonary physiology live in a vacuum. Heart-lung physiology is a more important cornerstone in an acute resuscitation of shock states—remember there is no V unless there is Q (we have been known to remind our trainees that Q comes before V in the alphabet)— returning to concepts of “What is happening with venous return, ventricular filling, contractility and afterload? What has been done to manipulate them so far? What dynamic parameters of fluid resuscitation have been tried/assessed? What vasopressors/inotropic agents have been tried, and what is the rationale for them? Why is the patient’s physiology not normalising?” can help understand what is happening to your patient and reduce the uncertainty on how to move forward. Furthermore, it is important to understand that other organs (e.g. brain, liver, kidneys, etc.) are also not idle bystanders and how they respond requires an understanding of the impact of the underlying illness on their function and of their own pathophysiological responses to attempts at resuscitation. Finally, the goal of any resuscitation is to save a person and the importance of always considering the impact of critical illness that is failing to respond to treatment on the brain – this may affect both the decisions made and the urgency of their implementation moving forward.
Admit you might have been wrong before and with the decisions you will now make
One of the most common and repeated fallacies in critical care is to fall in love with a theory of what is happening and to ignore the need for separation, and even that of eventual divorce, as scientific evidence emerges that the original premise is wrong. The emotional and psychological intensity of critical care medicine results in being prone to a multitude of biases that negatively impact any ability to solve or reduce uncertainty in decision-making. The first step is, therefore, to admit you may have been wrong, to suspend belief. Equally important is to admit you may still be wrong moving forward with whatever decisions you take. Such an approach engages cognitive forcing strategies (Christenson et al. 2022), promotes humility, avoids overconfidence, mitigates bias, will result in earlier re-evaluations of the accuracy of your hypotheses and will continue to support the generation of new ones when/if required.
Build a list of potential differential diagnoses, paths forward/treatment options
The analysis of data up to this point, consideration of physiology, and separation/divorce from previous thinking should help create a revised list of differential diagnoses, including what the diagnosis may be and what problems are occurring. This analysis can then be used to create a list of possible interventions and trials of treatment plans as well as a series of plans, i.e. plan A, B and C., in anticipation of negative events or new challenges. Writing these down can also serve as a potential roadmap to return to if any other difficulties arise along the way.
Investigate
What information or investigations do you still need to make a decision to move forward? As new potential causes and reasons for failure to respond to resuscitation/treatments are considered, more investigations and information may need to be sought. Or existing lab work may need to be repeated. A core question with respect to any new imaging is whether such imaging is possible if the patient needs to be transported out of the ICU for it to be performed. What information will it add? How will patient safety be maintained? (Lee et al. 2019).
Listen to others
Uncertainty and not knowing what to do next is not all that uncommon when a patient fails to respond to the initial resuscitation and treatment plans. The ICU can feel like a very isolating environment, yet intensivists do not work alone. Every healthcare provider plays a vital role in getting a patient through a life-threatening illness, and our inter-professional team is highly skilled in providing invaluable observations and insights into what is happening and generating ideas as they also attempt to stabilise the patient. Consulting with other intensivist colleagues and asking consulting services for help can make a significant difference. We conceive of this process as obtaining a 360-degree perspective of what is happening rather than a group thinking process (Christenson et al. 2022), for ultimately, decision-making responsibility will rest with the intensivist.
Irreversible
Though at times difficult to acknowledge, considering whether achieving stability is not possible is crucial. When a patient is not responding to treatment, it may be that a point has been reached when all subsequent treatments will only prolong death and add to suffering. If this is the case, then open, honest conversations should occur with the patient, their substitute decision-maker and family regarding what, if any, further treatment can/will be offered, taking into account whether such treatments would still fall within the standard of care (Lee et al. 2019) and, if they do, whether they would reflect the patient's values. If no further ICU treatments would change the outcome, the focus should be on alleviating distressing symptoms and suffering, and a palliative care plan should be initiated.
Zenith
After all these steps, though they may still feel very uncertain, intensivists are at the zenith of the decision-making process in the face of uncertainty. Decisions regarding the next steps now need to be taken, knowing they have done their best to undertake these after a comprehensive review of facts, an objective examination of past decisions and their results, after considering physiological principles and body mechanics, after consulting others and asking for input and help and finally after considering if any further interventions could potentially change the patient's outcome. The decision at this point may also be one to give more time for previous treatments to work, but it is important to understand that inaction must be an active choice.
Evaluation Endpoints
The final step of navigating an urgent path through uncertainty when a patient is acutely critically ill and not responding to treatment is to devise, a priori, a set of signs that would indicate either a response or a failure to respond to the newly initiated resuscitation/treatment plans. These evaluation endpoints may include haemodynamic and physiological parameters, laboratory values, active reassessments of heart-lung physiology, including echo/ultrasound, and mechanical ventilation parameters. Setting these endpoints in advance mandates a new therapeutic stop/pause during which this whole STABILIZE clinical algorithm can be repeated as required in the attempt to achieve the best possible outcomes that reflect patient wishes and values.
Conclusion
Some of the most challenging moments in critical care medicine encompass the need to make difficult, complex decisions in the face of uncertainty when patients are rapidly deteriorating and/or are failing to respond to the initial resuscitation and treatment plans. These are decisions that can haunt us throughout our careers. It is our hope that the STABILIZE algorithm may provide a path forward and help, in a small way, to reduce the anxiety and stress that intensivists feel in such situations.
Conflict of Interest
None.
References:
Borchard A, Schwappach DL, Barbir A, Bezzola P (2012) A systematic review of the effectiveness, compliance, and critical factors for implementation of safety checklists in surgery. Ann Surg. 256(6):925-933.
Christenson M, Shukla A, Patel JJ (2022) Intensive Care Unit Decision-Making in Uncertain and Stressful Conditions Part 2. Crit Care Clinics. 38(1):89-101.
Dennis D, Calhoun A, Khanna R et al. (2023) Stories from ICU Doctors: Navigating and Conquering Adversity. Springer.
Helou MA, Diaz Granados D, Ryan MS, Cyrus JW (2020) Uncertainty in Decision Making in Medicine: A Scoping Review and Thematic Analysis of Conceptual Models. Acad Med. 95(1):157-165.
Higginson IJ, Rumble C, Shipman C et al. (2015) The value of uncertainty in critical illness? An ethnographic study of patterns and conflicts in care and decision-making trajectories. BMC Anesthesiol. 16:11.
James FR, Power N, Laha S (2018) Decision-making in intensive care medicine – A review. J Intensive Care Soc. 19(3):247-258.
Lakoff G, Johnson M (1999) Philosophy in the Flesh: The Embodied Mind and Its Challenge to Western Thought. New York: Basic Books.
Lee JS, Roberts SWP, Gotsch K et al. (2019) Caring for Critically Ill Patients in Humanitarian Settings. Am J Respir Crit Care Med. 199(5):572-580.
Lighthall GK, Vazquez-Guillamet C (2015) Understanding Decision Making in Critical Care. Clin Med Res13(3-4):156-168.
LoPresti MA, Du RY, Yoshor D (2021) Timeout and Its Role in Neurosurgery. Neurosurgery. 89(2):266-274.
McKenzie MS, Auriemma CL, Olenik J et al. (2015) An Observational Study of Decision Making by Medical Intensivists. Crit Care Med. 43(8):1660-1668.
Mishima Y, Nawa N, Asada M et al. (2023) Impact of Antibiotic Timeouts in Multidisciplinary ICU Rounds for Antimicrobial Stewardship Program on Patient Survival: A Controlled Before-and-After Study. Crit Care Explor. 5(1):e0837.
Papadakis M, Meiwandi A, Grzybowski A (2019) The WHO Safer Surgery Checklist Time Out Procedure Revisited: Strategies to Optimise Compliance and Safety. Int J Surg. 69:19-22.
Tainter CR, Nguyen AP, Pollock KA et al. (2018) The impact of a daily "medication timeout in the Intensive Care Unit". J Crit Care. 43:366-369.





















