The increasing life expectancy of persons living with HIV (PLWH) due to effective antiretroviral therapy (ART) has led to a rise in non-AIDS-related health issues, notably cardiovascular disease (CVD). PLWH have an estimated fourfold higher rate of sudden cardiac death compared to the general population, though the exact reasons are not fully understood. Early detection of subclinical CVD in young PLWH is crucial for effective intervention and management. A study recently published in Radiology: Cardiothoracic Imaging aimed to use MRI to assess CAD burden in adult PLWH with low Framingham scores and no history of CVD, comparing them to healthy controls. Additionally, the study sought to determine if subclinical CAD in PLWH correlates with echocardiographic measures of myocardial function.
Intersection of HIV, Antiretroviral Therapy, and Cardiovascular Disease
Traditional markers like coronary artery calcium, assessed by cardiac CT, are less effective in PLWH due to a predominance of noncalcified coronary plaque. While coronary CT angiography can detect noncalcified plaque, it may not be ideal for long-term monitoring, especially in young PLWH and diverse demographic groups. Studies have shown that despite having preserved overall heart function, PLWH often exhibit early diastolic dysfunction and abnormalities in myocardial strain. For instance, middle-aged PLWH were found to be more than twice as likely to have diastolic dysfunction compared to controls without HIV. Furthermore, early signs of coronary artery pathology, such as increased coronary vessel wall thickening, have been observed in young PLWH, suggesting early coronary artery disease (CAD) development.
Study Design and Participant Overview
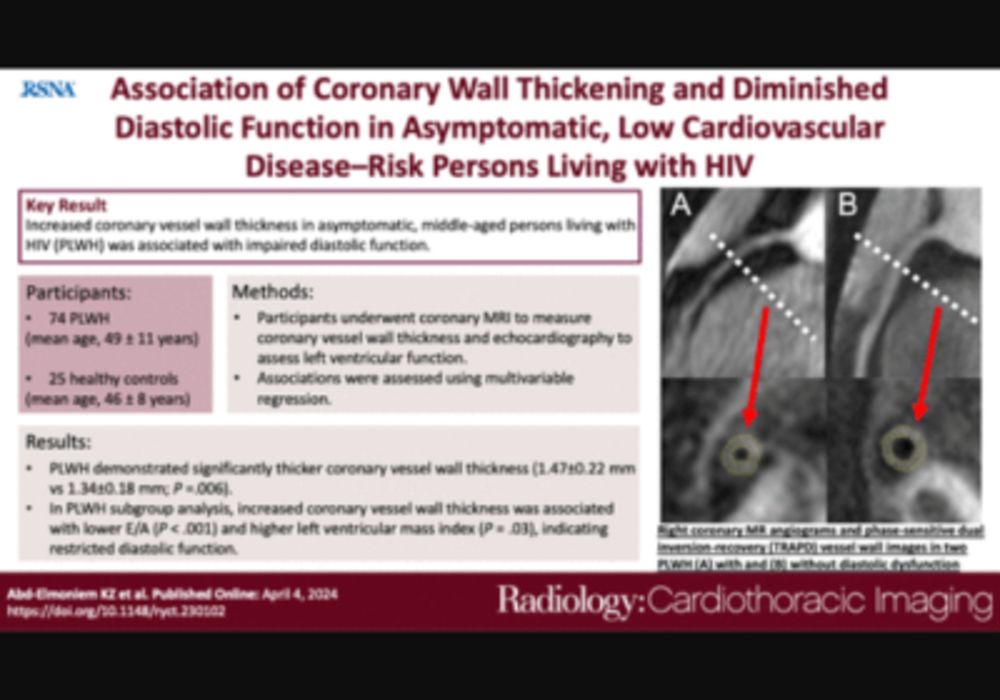
The authors conducted a prospective study from April 2010 to May 2013 at the National Institutes of Health, evaluating 74 adult persons living with HIV (PLWH) and 25 age-, sex-, and race-matched controls. All participants provided written informed consent, and the study was approved by the institutional review board and compliant with the Health Insurance Portability and Accountability Act. Participants were recruited through self-referral and local advertisements. Exclusions included contraindications to MRI or known cardiovascular disease (CVD). There were no restrictions on antiretroviral therapy (ART) use, HIV suppression, or CD4+ T-cell count. Controls were HIV-negative and healthy with no significant medical conditions, including CVD. Each participant underwent a detailed medical history, physical examination, and laboratory tests, including fasting lipid panel, CD4+ and CD8+ T-cell count, and HIV viral load measurements. The study focused on coronary vessel wall thickness (VWT) in association with diastolic function.
Influence of Diabetes and Antiretroviral Therapy on Coronary Pathology
In this study, middle-aged persons living with HIV (PLWH) who had low Framingham Risk Scores (FRS) and no known cardiovascular disease (CVD) were found to have increased coronary vessel wall thickness (VWT) and left ventricular mass index (LVMI) compared to healthy controls. This association with HIV remained significant even after adjusting for age and was further influenced by diabetes. Increased coronary VWT was also linked to a reduced E/A ratio, indicating impaired diastolic function. The study utilized echocardiography and MRI to understand the relationship between coronary pathology and myocardial function in PLWH. The study highlighted that coronary artery VWT, measured using MRI, could serve as a potential indicator of diastolic dysfunction and coronary pathology in PLWH. The findings also revealed that diabetes had a significant impact on coronary artery VWT, as it is a known risk factor for CVD. The study further discussed the complexities of coronary wall thickening in PLWH, which could be due to chronic inflammation triggered by HIV infection, vascular injury, or metabolic abnormalities associated with antiretroviral therapy (ART). The use of specific ART drugs like didanosine was associated with increased coronary VWT, possibly due to altered endothelial-leukocyte interactions. The study used a reliable method called TRAPD for measuring coronary artery VWT, considering various imaging factors to ensure accuracy. Despite some limitations, such as the cross-sectional design and potential selection bias, the study provides valuable insights into the association between coronary thickening and diastolic dysfunction in PLWH.
In conclusion, this study suggests that increased coronary artery VWT detected by MRI may indicate early coronary pathology and impaired diastolic function in middle-aged PLWH with low FRS. While the observational nature of the study precludes establishing direct causality, these findings underscore the importance of early detection and monitoring of cardiovascular abnormalities in PLWH to inform risk modification strategies and future research.
Source & Image Credit: Radiology Cardiothoracic Imaging