HealthManagement, Volume 23 - Issue 4, 2023
Awareness, systems approach, interaction from top-down and bottom-up, willingness and urgency to take action and tackle the climate change problem with the decarbonisation of the health sector will require efforts from people involved in healthcare and the environment, according to the principle of “One Health”. Interventions are urgent. Time is of the essence.
Key Points
- The greenhouse effect is when solar radiation penetrates the atmosphere and hits the Earth with energy as short-wave rays. It strikes the Earth, generating heat that gets re-emitted as infrared rays, that is, long-wave rays. The greenhouse gases retain a relevant portion of those infrared radiations and form a coating around the troposphere, the closest layer to the Earth’s atmosphere.
- Greenhouse gas (GHG) is any gas that has the property of absorbing infrared radiation (net heat energy) emitted from the Earth’s surface and re-radiating it back to the atmosphere, thus contributing to the greenhouse effect. Carbon dioxide, methane, and water vapour are the most important greenhouse gases.
- A moderate layer of greenhouse gases in the troposphere, when regulated mostly by nature, was performing a positive role with its protecting effect and its temperature. The accumulation of a thick layer of GHG in the troposphere has a profound negative effect on the energy budget of the Earth’s system, producing excessive heat, with consequences on human and environmental health and the disasters related to climate change.
- Carbon footprint measures human impact on the environment with the amount of greenhouse gases produced.
- Ecological footprint measures human demand on the Earth’s ecological capacity.
- CO2 E or CO2-eq. is a metric measure used to compare emissions from various greenhouse gases based on their global warming potential (GWP).
- Decarbonisation is a set of coordinated actions aimed at eliminating or reducing near-zero emissions of a single infrastructure or a set.
- Systems theory and systems analysis are basic approaches when studying human and other living environments in the complexity of their relations.

Framework
“Primum non nocere - First do no harm” is the oath of ethics historically taken by physicians.
Health professionals and anyone dealing with health matters know the Hippocrates oath and assume it originally referred to doing no harm to your patient.
It took a long time and a long evolution of society to reach an organisation and physical structure - the hospital in the modern sense - for taking care of sick persons. It was not even considered a question that the hospital had to respect the complexity of its patients based on the ancient “first do no harm”. The hospital became synonymous with a place for recovery. Most of us remember the blunt definition of the famous architect Le Corbusier of the hospital as “la machine à guérir” or the healing machine.
With the evolution of the concept of where and how to give medical assistance to sick persons, what was happening inside the main healing machine came under scrutiny: on one side, the question of how the patients were treated and the hygienic conditions, on the other emerging evidence that there were materials and procedures, used inside hospitals, that could do harm to patients and not only to them.
One of the most important international organisations that started promoting inquiries about the matters was and continues to be Health Care Without Harm (HCWH). This organisation was created in the U.S. more than 30 years ago and is now present in all continents and, in the last 20 years, has also been operating in Europe. One of the most relevant battles won by HCWH has been the elimination of the use of mercury in hospitals, which proved to be dangerous for patients and medical staff.
In recent times, healthcare and its specific authorities, such as NHS in the U.K. or SSN in Italy, and other private systems publicly subsidised, started to attract attention from the economic aspect of politicians and policymakers. Healthcare was openly declared too heavy a burden on public finances; especially the energy consumption of the major infrastructures, the hospitals, came under scrutiny.
Hospital managers were aware of the large energy consumption of their infrastructure, but realistically, even with increasing fuel prices, they were pointing out that the total staff needed, the medicines and the medical devices were, by a large margin, a heavier burden due to insufficient finances. Energy costs, certainly with some relevance, were contained, almost hidden, among the general maintenance costs.
Analysing only the economic factor, this evaluation could be justifiable due to the poor or insufficient awareness of the related environmental problems. In a large survey conducted in 2012 with hospital managers involving eight countries in a European project, the burden on the environment for satisfying the needs of “energivorous” structures as the hospitals were not yet considered. A good number of hospital managers answering the questionnaire declared that how energy was produced and supplied to hospitals was not “their problem”, and their primary duty was curing patients.
The effects of climate change were already starting to be more and more evident. Calamitous events had started to directly involve hospitals, like the Katrina Hurricane in 2005, destroying an entire hospital in New Orleans, Louisiana, and then others that followed. Disastrous heatwaves in many countries caused hospitals to fill up with sick people, especially from the weakest strata of the urban populations. Healthcare was made to recognise the relevance of climate change and the need to consider it a danger.
In a relatively short time, the focus became the need to defend against the effects of climate change on the healthcare infrastructure, with justified concern for safeguarding their operability, from energy and water supplies to electricity, communications, connection infrastructures, such as roads, bridges, etc., - in short to protect their serviceability in case of calamities. In other words, the aspects related to the protection from the possible risks to which climate change could subject hospitals became an emerging important duty of the hospitals.
We devoted ourselves intensively to studying and talking about resilience, mitigation, and adaptation - in short, to see how to protect hospital infrastructures from the problems posed by the ‘enemy’ climate change, without having sufficiently understood, at least at first, that they were and are also part of that enemy.
In the years when ecological thinking was growing and developing, there were attempts by scholars to address the problem of assessing the footprint, i.e. the burden of hospital infrastructures on the environment. They were, however, relatively few and not sufficiently understood. This was matched by a larger contribution in studies, guides, standards and regulations on the challenge to the risks caused by climate change on healthcare infrastructures. I directed a study for S.I.A.I.S. (Società Italiana dell’Architettura e dell’Ingegneria per la Sanità) called “Sustainable and Climate Change Resilient Healthcare Facilities in Europe: the Challenge”, which was awarded a prize for leadership in climate change in 2018 at the First Climate Change Summit In London, held by Health Care Without Harm, Europe.
The Gradual Recognition of Healthcare as a Polluter
More recently, a serious introspection of the situation began to be more largely felt as necessary inside the healthcare system. In the beginning, this was mostly considering, but not limited to, the contribution to the greenhouse effect. Different types of pollution were progressively brought up to the front by the medical staff directly involved in the therapeutic part of healthcare.
In the day-to-day activities of individual healthcare units and the medical sector in general, attention began to be paid to the set of factors that led the healthcare system as a whole to be one of the most critical contributors not only to the production of GHGs but also more extensively for air pollution and plastic invasion with the addition of indirect pollution produced by its supply chain, an indispensable factor of the hospital operational activity.
Although the documentation is beginning to be relevant, it is not yet completely homogenous, nor is it sufficiently permeated into the day-to-day working of the health systems in the different social, economic, and urban characteristics and environments. Another problem, which unfortunately is not affecting only healthcare, is the enormous difference in awareness of these problems from country to country and globally, due, among others, to the different languages with little circulation of knowledge and information, determining a state of poor common action, despite the efforts relevant of the European Union. The “energy transition is suffering from the same problem”, even if energy was the first to receive attention because of its repercussions and links initially with economic aspects, then slowly with environmental problems.
However, it is necessary to grant, support and try to valorise that a certain relevance of analysis has been reached. Many aspects that make the hospitals contributors, not merely victims, to the effects produced by climate change and related health problems start to be identified and tackled as we will explore, in a more diffused way and should start to produce results.
Studies that have focused their attention on the healthcare system as a producer of GHGs, the various types of gases that are trapped mostly in the lower layer of the atmosphere, the troposphere, have led to the attribution to healthcare worldwide of around 5% of the total climate-changing gases, consisting mainly of the most influential, long-lasting- greenhouse gases, carbon dioxide (CO2), methane (CH4), and nitrous oxide (N2O). These are joined by other gases in smaller proportions, but some, such as the group of fluorinated hydrocarbons, have a high impact on air quality and are relevant inside the hospitals.
The percentage of GHGs produced by the healthcare sector is not the same in different areas of the planet, depending on geomorphological characteristics and economic, social, and urban factors (that is, anthropomorphic) in each area. For Europe as a whole, it is considered to be between 4 and 5%, while some studies attribute higher values of 7 to 10% to the United States, and even higher percentages are attributed to other areas of the planet.
Global warming is now well known for all its direct negative effects and consequences. Air pollution is the fourth leading cause of mortality worldwide. In Europe, it causes around 350,000 deaths a year. The relationship between the presence of air pollutants and the increase in respiratory or cardiovascular diseases has already been proven in several studies. In recent times, surveys carried out by the European Space Agency in periods before, during and after the pandemic have shown a significant correlation between pollution levels and the spread of COVID-19.
It is evident, from these initial considerations, that those who work in the health sector have and are starting to take into account the issue of emissions coming from health activities as one of the fundamental problems that must be qualitatively and quantitatively analysed to develop actions for their reduction, if not their elimination. The aim is to have health systems that are taking concrete action to reduce pollution and stop contributing to unhealthy living conditions when healing people.
Under the stimulus of the goals developed during the Conference of Parties (COP) 21 in 2015 and collected in the document known as the Paris Agreement, many studies have emerged dedicated to showing how much the health sector has to become conscious of its environmental sins.
Among them, the study produced by HCHW in collaboration with the research company ARUP, “Health Care’s Climate Footprint - How the Health Care Sector Contributes to the Global Crisis and Opportunities for Action”, was among the first to explicitly highlight the healthcare sector’s contribution to the global climate change related crisis and possible actions against it. A further value of this study was that it pointed the finger at the socially unjust aspect of the effects of climate change. Striking is the example of Bangladesh, one of the poorest countries in the world and most affected by catastrophic flooding due to climate change, which has put a crowded and fragile territory at risk, even though it is responsible for only 0.1% of climate-changing emissions.
Gradually, more studies deepened the link between climate change and human health. The Centre for Disease Control and Prevention (CDC) defined the nation’s leading science-based, data-driven impact of climate change on human health (Figure 1).
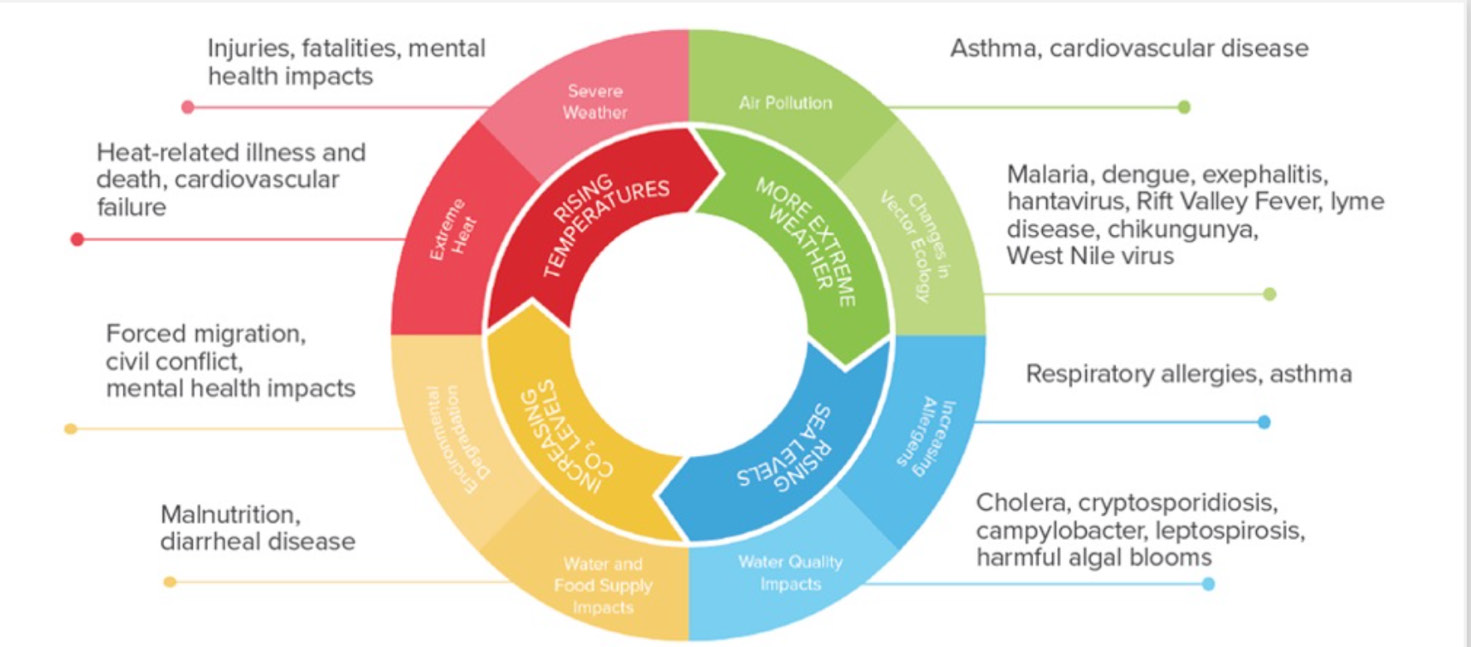 Figure 1. Impact of climate change on human health (Source: U.S. Center for Disease Control and Prevention)
Figure 1. Impact of climate change on human health (Source: U.S. Center for Disease Control and Prevention)
In parallel to this, there have been and continue to be studies extending the knowledge of how the healthcare sector has an environmental impact. The concept of carbon footprint is now considered in hospitals, and its evaluation progressively is addressed to all the aspects of the possible harm to patients and staff.
The Carbon Footprint of the Healthcare System - One of the Main Actors
The environmental footprint of people or systems, in this case, the healthcare system, is referred to as the carbon footprint. This does not encompass the totality of the hospital’s polluting factors. In most cases, the focus is on the largest climate-altering gases, such as CO2, in the complex of hospital activities, which directly contributes to climate change. The ecological footprint, on the other hand, goes beyond what is covered by GHGs. The evaluation of the ecological footprint takes into account which and how many resources are required and taken away from/subtracted to the planet’s ecological systems to operate and involves also looking at other types of pollution that cannot be measured by CO2 and CO2 E . Carbon dioxide equivalent (CO2-eq), is a metric measure used to compare emissions from various greenhouse gases on the bases of their global-warming potential (GWP). To be even clearer, GWP measures how much energy the emissions of 1 ton of a gas will absorb over a given period relative to 1 ton of carbon dioxide (CO2) emissions. It also takes into consideration the duration of the effect.
The difference between carbon footprint and ecological footprint was already expressed by Professor Samanthi in 2011, when he said, “The fundamental difference between the ecological footprint and the carbon footprint is that the ecological footprint measures human demand on the Earth’s ecological capacity, while the carbon footprint measures human impact on the environment with the amount of greenhouse gases produced measured in units of carbon dioxide or carbon dioxide equivalent” (reproposed by Richie et al. 2020).
Among the various visualisations of differences, two complementary images seem the most representative:
The first observation when examining the carbon footprint of hospitals is that we encounter multiple gases. Even in the healthcare system, there is a prevalence of CO2. The other gases include methane CH4, various nitrogen compounds from NO with limited toxicity to the very polluting NO2, nitrous oxide and all the other combinations of nitrogen and oxygen, indicated as NOx, to the variety of fluorinated hydrocarbons.
The burden of the hospital footprint can be seen through CO2 equivalent, making it possible to find a way to measure the weight of each gas on global emissions and consequently to make the sum for determining the total burden. According to the protocol drawn by the scientists of the International Panel on Climate Change, each pollutant is assigned a GWP (Global Warming Potential). Starting with the ‘weight’ equal 1 for CO2, it rises to 25 for methane and 298 for NO2, nitrous oxide, and well beyond for fluorinated hydrocarbons. The numbers given here are the ones reported by Eurostat.
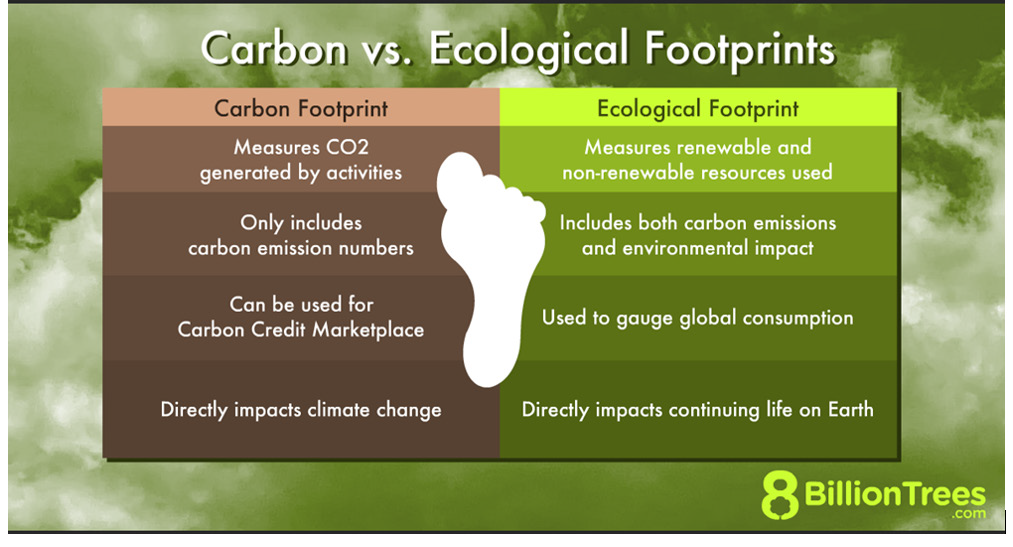
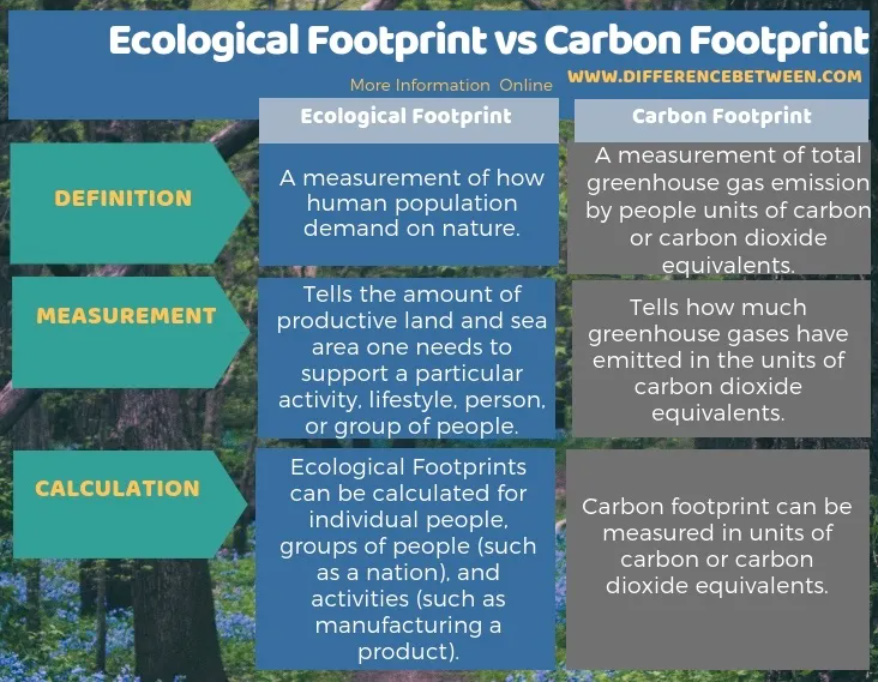
Image: Carbon footprint by Notnarayan via Wikimedia Commons
There are many studies on the hospital footprint. A study by Rodríguez-Jiménez et al. (2023) conducted an electronic search that produced 4368 records. After the screening process, 13 studies were included in their review. The studies were all in English and conducted in different locations between 2012 and 2022: one in Morocco, one in Japan, two in the United States, three in Australia, two in Switzerland, one in the U.K., one in China and two in Canada. This literature review included studies that calculated the carbon footprint of a complete hospital and some only a functional unit in a healthcare setting. The studies were done using one of the following methods: bottom-up life cycle assessment (Keller et al. 2021; Lim et al. 2013; MacNeill et al. 2017; Mtioui et al. 2021); top-down cycle assessment or economic input–output analysis (Eckelman et al. 2018; Eckelman and Sherman 2016; Malik et al. 2018; Nansai et al. 2020; Wu 2019); or a combination of both, also known as hybrid model (Tennison et al. 2021).
The Tennison study applied the hybrid model and provided with its analysis the most comprehensive view of the carbon footprint of hospitals. Stressing the usefulness of the greenhouse accounting, it clarifies the strategic points where to concentrate mitigation efforts. It has focused on evaluating the carbon footprint involving NHS healthcare facilities in England (Tennison et al. 2021). Since its publication, it has become a point of reference for the work concerning the carbon footprint of hospitals, making it worth a more extensive examination.
The methodology started with quantifying emissions using the Greenhouse Gas Protocol associated with NHS emission categories. The emissions are subdivided according to Scopes 1, 2 and 3, which is routinely done, even if the items referred to in the three scopes have some variations from one work to another. In the case of this study, the attribution to the scopes of the emissions was:
- Scope 1 - Covers the direct emission deriving from the provision of care;
- Scope 2 - Covers emissions from the energy in almost all the cases still purchased for the general operation of supplying the care, including the use of medical equipment;
- Scope 3 - Covers water needed and waste produced, measurable gases emitted by equipment for treatment, such as sprays, with some other qualifications. Scope 3 also includes GHG emissions from the chain of suppliers in making and delivering products and those from services commissioned to third parties.
In this study, patients’ and visitors’ travels were considered a part of the study since they are not included in the NHS protocol. The same is true for commissioned health services. Due to the not always similar focus of the research, differences in the attribution to Scope 2 or 3 are noticeable among studies, without changes to the validity of the findings.
The NHS study covered the period 1990-2019 and focused on gas emissions of CO2, CH4, N2O and some categories of fluorinated gases. It correctly underlined that some medicines and pharmaceuticals, in addition to the manufacturing footprint of the production (considered in the supply chain), have emissions that were appropriate to be included in Scope 1. Precisely, they are anaesthetic gases, propellants of inhaled medicines and other medical and surgical gases producing GHGs when used inside the hospital. Volatile anaesthetics such as sevoflurane, isoflurane and desflurane are potent greenhouse gases, not considered pollutants till relatively recent times, and now finally getting attention.
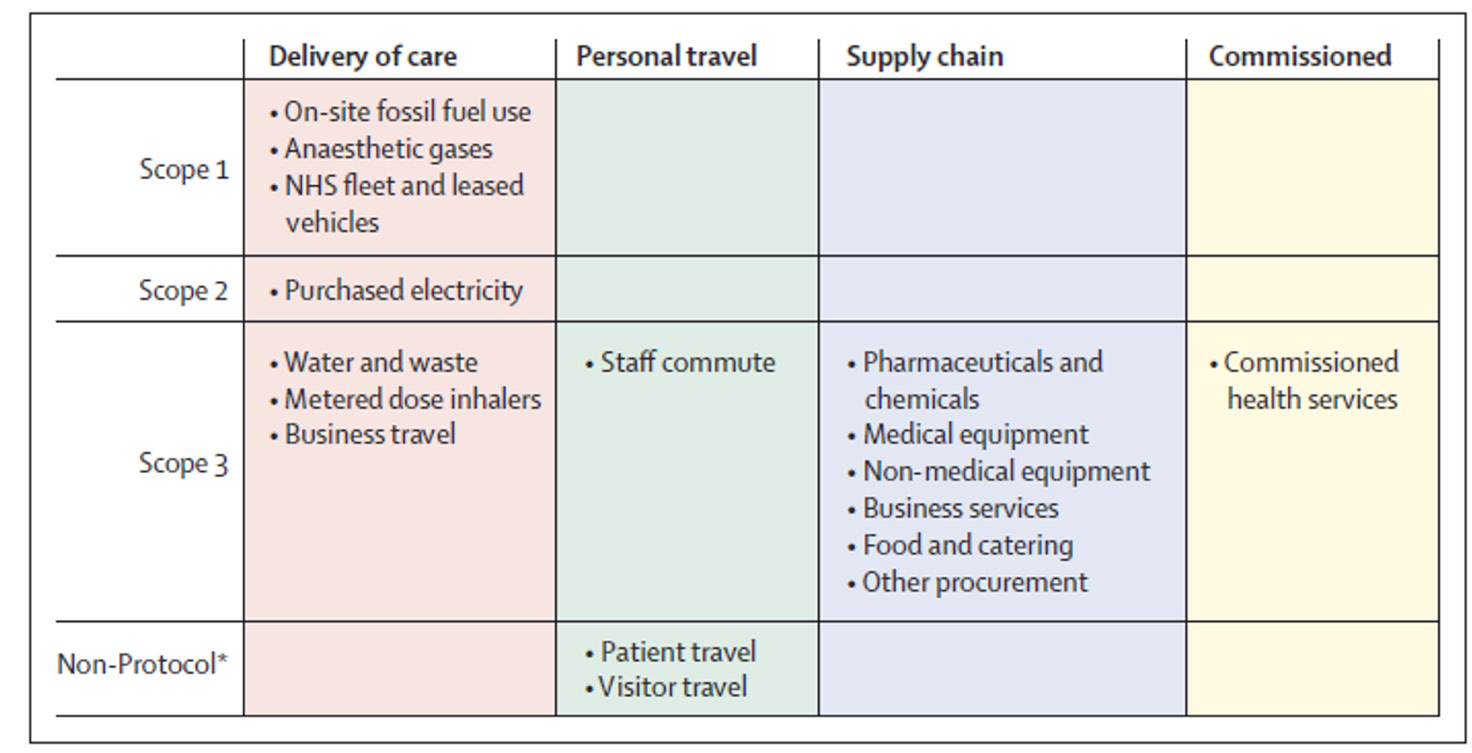 Table 1. Sources of emissions organised by Greenhouse Gas Protocol Scopes and NHS emission categories. Columns represent NHS emission categories, and rows the Greenhouse Gas Protocol Scopes. NHS=National Health Services
Table 1. Sources of emissions organised by Greenhouse Gas Protocol Scopes and NHS emission categories. Columns represent NHS emission categories, and rows the Greenhouse Gas Protocol Scopes. NHS=National Health Services
The following figure represents the situation in 2019 when the study was completed. Some important observations can be made to give a correct interpretation of the figure and the results that it visualises. In the article, the authors themselves offer some relevant keys of interpretation.
The first is that the situation exposed is representative of NHS, with England as the primary region of focus. The authors underline that it can also be referred to as U.K. The first specific observation, certainly one of the most evident from the figure, than follows, is the very relevant weight of the supply chain, even more, compared with the delivery of care. This can be influenced by the fact that in 2019 in the U.K. and also in England, NHS could count on advanced decarbonisation of energy production; therefore, Scope 1 comes out in this study as having reduced its relative weight, making the weight of the supply chain more relevant. It is, however, necessary to highlight that in the 13 cases examined in different local and national contexts by the study reported previously (Rodríguez-Jiménez et al. 2023). the weight of the supply chain came out as very high in many cases due to manufacturing, packaging and transport of medicines and goods. As stressed in the NHS-England study, it is undeniable that there is an objective difficulty for the healthcare sector to take action to get improvements from the supply chain.
Inside the Delivery of Care
Scope 3: The present situation could be described as the health sector being dependent, especially on the so-called big pharma, mostly from the pharmaceutical and medical equipment sectors, which has been highlighted in many circumstances. The experience of the recent pandemic is a confirmation of the present state. The reduction of the weight of Scope 3 cannot be left to the goodwill of the supply chain, nor is it possible to accept the “greenwashing” that has started to emerge in some healthcare-related production areas without delivering tangible results. The healthcare systems need to concretely realise the reduction of their carbon footprint. It is possible not to be at the mercy of the supply chain. It is a matter of discussion to see which possible ways to reach results in this scope.
Scope 2: This is related to the supply of energy. The answer should be easy because the energy sector was the first to receive the initial pressure to reduce its costs (energy saving campaigns, efficiency, use of renewable energy sources, etc.), so it should be ready to switch to clean, renewable energy use. Up to now, the results have not been as good as they could and should be. The photovoltaic has made a big advancement. Eolic use of green hydrogen, new construction materials and technology devoted to energy saving are also promising. In front of this great development of new technologies, what is still missing is the support of a political and policy vision in some European nations more than in others. For example, the EU made large funds available from the Next Generation Europe, developing the “Recovery and Resilience Plan” programme. Italy got the largest amount of funding. The plan of investment was prepared. Among the six missions to be implemented, there was one called “Energy Revolution”, supposedly devoted to energy transition in a number of production sectors. Despite the recognised relevant need for energy in the healthcare sector, it was not considered for receiving a contribution from these funds. So, the energy transition of the healthcare sector toward the reduction of GHGs regarding energy, for lack of more consistent public financial support, is dependent on the meagre funds of the hospitals and/or on the decisions of energy producers, based mainly on economic evaluations.
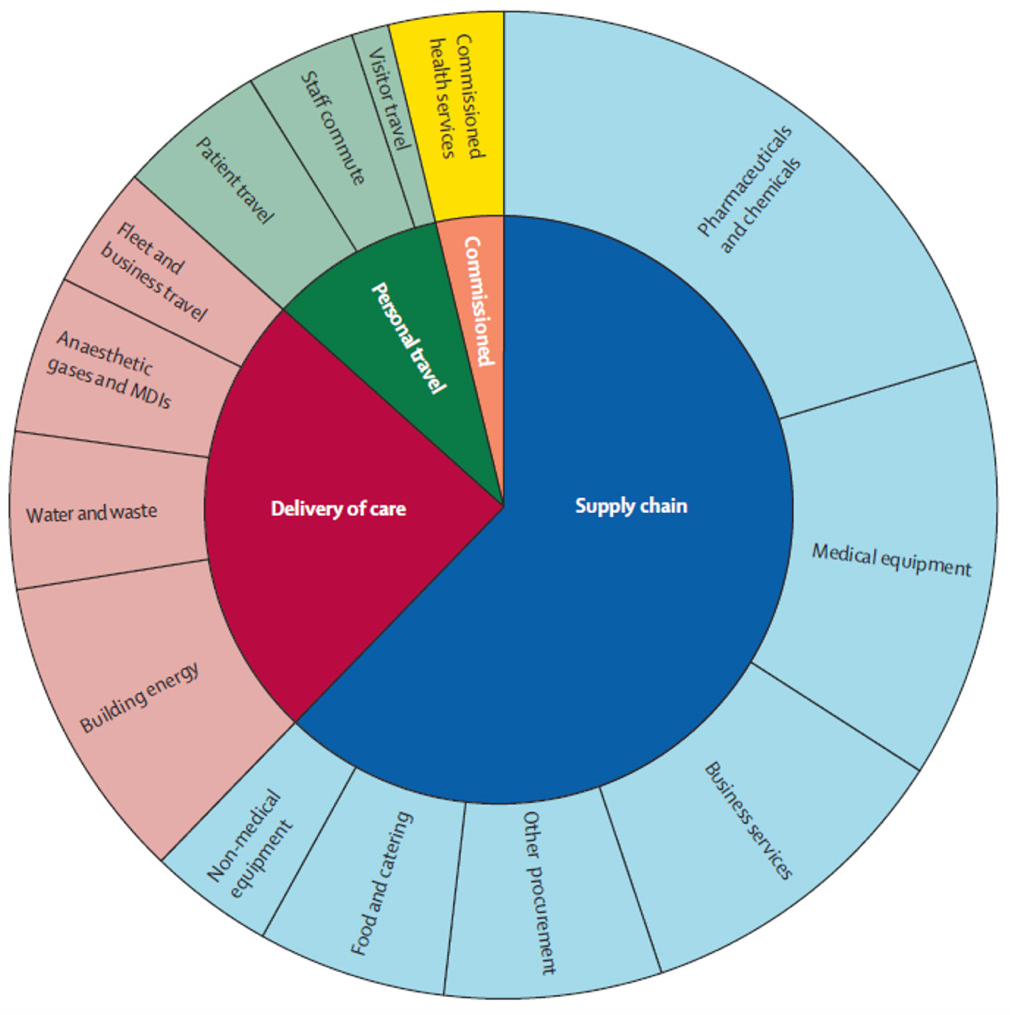
Figure 2. Contribution of different sectors to the greenhouse gas emissions of the NHS England, 2019.
Scope 1: This is not as irrelevant as it could be perceived at first glance. We start to analyse what goes on inside the hospitals in care delivery or what used to go on until “yesterday”. The first point is the extra-consumption (=waste) and misuse inside the hospital, which consists of energy, use of pharmaceuticals and chemicals, and excess tests and medicines. We can also consider hazardous waste production, general waste production (including the part coming from food), and the production of plastic waste with single-use gloves and utensils.
This overview cannot leave out what needs to be done better/differently, as the management of the buildings is certainly very important. Hospitals have to contribute to reducing GHG production and protecting (guaranteeing resilience, mitigation, etc.) from the risks of the already advanced climate change. Transport and commuting are relevant producers of emissions. It is realistic to say that this sector, which involves the relationship with the so-called “territorial healthcare” and the relationship with the served territory, could be highly improved. Certainly, the necessity of a new vision rethinking institutional as well as organisational changes has to be holistic.
Towards Environmentally Conscious Healthcare Systems
We mentioned before that the decarbonisation of the health systems requires a comprehensive vision and systems approach. Digitalisation cannot involve only a sector of the hospital organisation, nor (systemic approach) the effects an action can have on other parts and, enlarging the circles, on the entire system. The work that needs to be done is certainly complex. It requires environmental awareness of the stakeholders, medical and non-medical staff and the patients, but the need for change has to also be shared by policymakers at all levels. Examples that indicate the way exist and are starting to become known. One of the recent and relevant is the decision of the NHS Scotland to eliminate desflurane. It has become the first national health service in the U.K. to stop using an anaesthetic with a high global warming potential. Desflurane used as an anaesthetic during surgery, has, as many studies report, a global warming potential 2,500 times greater than carbon dioxide.
The danger to the environment of the anaesthetic gases is not a new discovery. Yasny et al. (2012) stated that “for several decades, anaesthetic gases have greatly enhanced the comfort and outcome for patients during surgery. The benefits of these agents have heavily outweighed the risks. In recent years, the attention towards their contribution to global climate change and the environment has increased. Anaesthesia providers have a responsibility to minimise unnecessary atmospheric pollution by utilising techniques that can lessen any adverse effects of these gases on the environment.”
This proves how updating the parameters to evaluate care procedures in hospitals is necessary. NHS Scotland has to be praised for this important step. It received, among others, the first prize during CleanMed 2023, one of the most significant European events regarding health and the environment, with one week of exchange and brainstorming about healthcare problems, solutions, and vision organised this year in Berlin by HCWH-EU. Hopefully, it will be followed by many other systems and hospitals. But a fundamental question that needs to be raised is timing. Considering how fast the devastations of climate change are happening, do we have the option to take it easy? Should we not accelerate the actions of decarbonisation? Especially now that we know much better where we have to focus. Success in the healthcare sector could also be evaluated by examples from other sectors, considering how diffused is its supply chain.
This brings us to the tender spot, which is the large consensus that healthcare can do very little about the supply chain. An interesting discussion paper developed as part of a collaboration between AstraZeneca and The Health Policy Partnership Ltd. raises the point: “Health systems are complex, and decarbonisation strategies must take a systems approach to have a meaningful impact”. Equally, if not more interesting to consider, is what concerns the supply chain, “the supply chains make a significant contribution to carbon emissions through the production, transport and disposal of goods and services (e.g. medicines, medical devices, food and hospital equipment). Health systems could support lower-carbon supply chains by ensuring manufacturers are decarbonising their processes with verifiable targets, such as the Net Zero Corporate Standard defined by the Science Based Targets initiative. Suppliers could also provide evidence of their progress in line with these targets.”
This goes with what several sources say that the key to control the supply chain is public procurement. We are convinced that tools like PPI (Public Procurement of Innovation), P-CP (Pre-Commercial Procurement) and others could make a difference. The subject is complex and multifaceted and deserves a full article, but it is important to register that also, from the supplies side, interventions are pointed out as necessary.
Even part of the supply chain indicates that while it is difficult to make it go towards decarbonisation, it is not impossible. The crucial point is the willingness, at all levels, to acknowledge the importance and to give the public sector the necessary tools and power to make decarbonisation a priority.
Conclusion
It is important to go back to the statement about timing. A lot of knowledge has been acquired for the decarbonisation of the health sector. There are certainly other sides that need to be considered. Antonio Bonaldi is a great expert on the matter, the originator of the great activity undertaken by the Local Health Authority Bergamo-est, leading Italy in a systemic approach to decarbonisation and collaboration with local government. He is now working with other important actors on improving the ecological outputs of healthcare: the MMGs. Their potential contribution is twofold: to have the healthcare outside hospitals minimise its impact while not reducing the quality of care and possibly improving it, and contribute to awareness of people, starting with patients.
Back to the biggest polluter of the health sector: the hospitals. A question that emerges is whether the definition of green hospitals expresses sufficiently and adequately the present role of this crucial health entity. Environmentally conscious health systems and sub-systems of the larger healthcare sector appear to be highly significant, but more than a definition, what is important is the action/the actions. We cannot take it easy with decarbonising hospitals, waiting for other important sectors to move. The financial means that will bring enormous co-benefits need to be found urgently. Time is of the essence for making the health sector, and its major actor, the hospital, not only in the first line for “repairing” persons’ health but also a leader in “repairing” the environment.
Conflict of Interest
None.
















