The European Health Data Space (EHDS) is a health-specific ecosystem comprising rules, common standards and practices, infrastructures and a governance framework aiming at empowering individuals through health data access and researchers through a trustworthy set-up for health data research. This session chaired by Luis Marti-Bonmati (Spain) will provide an overview of what the EHDS is from the EU perspective, how it is perceived by patients and what challenges to data exchange lie ahead.
The EU vision for health data exchange
Aleksandra Wesolowska (Luxembourg) shed light on the EU's ambitious plans for health data exchange and innovation. As part of the Commission's broader European data strategy, the importance of interoperable data spaces across key sectors, including health, has been underscored. The COVID-19 pandemic further highlighted the critical role of digital services and data availability in healthcare, prompting a concerted effort to bolster Europe's capabilities in this domain. The EU's vision for health data exchange encompasses addressing multifaceted challenges, including issues related to individual data access and control, healthcare professional data access across different institutions and borders, and policymakers' access to reliable data for evidence-based decision-making. Moreover, barriers to interoperability among digital health solutions and the scarcity of quality health data for research and innovation have been identified as pressing concerns.
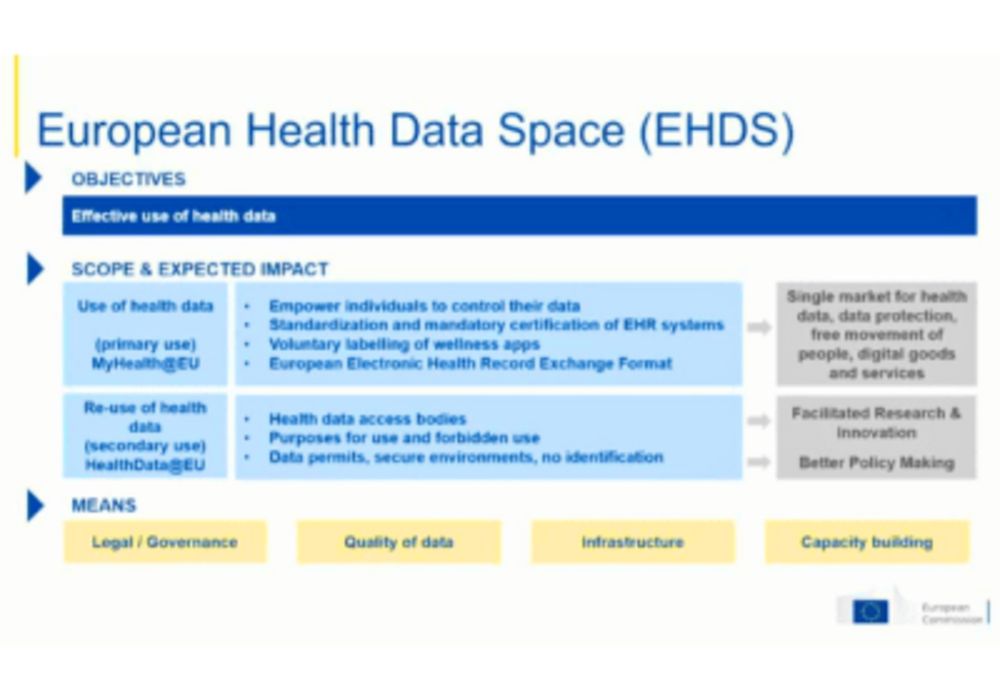
To tackle these challenges, the European Commission has proposed the creation of a European Health Data Space (EHDS) and regulatory frameworks to govern the primary and secondary use of health data. The EHDS aims to establish rules, infrastructure, and governance frameworks to facilitate the pooling and sharing of health data while upholding European values and standards, particularly concerning sensitive personal data. Key provisions of the EHDS regulation include empowering individuals to control their health data, prioritising access for healthcare professionals to essential categories of data such as imaging studies, and mandating the standardisation and certification of electronic health record systems to enhance interoperability.
For primary data use, the existing infrastructure of My Health@EU provides a foundation for exchanging patient summaries, e-prescriptions, and clinical documents across member states. As part of the EHDS roadmap, participation in this infrastructure is set to become mandatory, with additional services planned for laboratory results, medical imaging, and discharge letters.
In parallel, efforts are underway to develop a decentralised EU cross-border infrastructure for the secondary use of health data. This includes the establishment of health data access bodies to grant permissions for data access and the implementation of secure processing environments to safeguard data privacy and security.
Furthermore, projects such as the Cancer Imaging Initiative, the 1+Million Genomes initiative, or the Virtual Human Twins programme exemplify the EU's commitment to fostering innovation and leveraging data for research in healthcare while safeguarding patients’ rights.
The EU aims to unlock the full potential of health data while ensuring compliance with European values and regulations. Through these concerted efforts, Europe seeks to position itself as a global leader in digital health and data-driven solutions, poised to address current healthcare challenges and future emergencies effectively.
The patient perspective on data exchange
Erik Briers (Belgium), member of the ESR patient advocacy group and a cancer patient himself, emphasised in his lecture the importance of not forgetting the patients amidst all the technical discussions. Highlighting the intricate web of personal health data, encompassing everything from genetic predispositions to past medical events, he underscored the importance of understanding the holistic journey of each patient.
Health data is multifaceted by nature, spanning verbal, written, and structured sources past and present, each contributing to the comprehensive picture of an individual's health profile. However, challenges arise concerning the accessibility and standardisation of this data, particularly when integrating data from disparate sources such as clinical trials or medical records.
Addressing concerns around data privacy and consent, patient empowerment means controlling access to their health information, emphasising the need for transparent and secure data-sharing mechanisms. Moreover, ensuring data integrity is critical, and any misuse or unauthorised access should face severe penalties.
A key focus of the discussion is the potential of health data sharing to drive research and innovation, ultimately benefiting both current and future patients. However, the quality and standardisation of data emerge as critical hurdles in leveraging the full potential of large-scale data projects. The process of distilling vast amounts of medical literature into evidence-based recommendations must be rigorous, discerning between credible and unreliable sources of data is critical. Continued collaboration and vigilance are necessary in navigating the complexities of health data exchange, with the ultimate goal of improving patient care and outcomes.