With industry companies publicizing their efforts to decrease the energy consumption of devices and unveiling AI solutions for power management, sustainability was one of the main keywords of the ECR (European Congress of Radiology) congress in Vienna. In a session chaired by Jose Guilherme Couto (Malta) and Philipp Brantner (Switzerland), lecturers presented their insights and field experiences to make radiology green and sustainable. Defined as the capacity of a health service to deliver healthcare over time, with consideration to future generations, sustainability can be financial, societal and environmental. Prioritizing only safety, cost savings and convenience is not enough, future focus should also be on sustainability.
Tips for making more effective use of departmental resources
Andrea Grace Rockwell delved into her experience to deliver great impact on departmental resources management and reduce radiology’s carbon footprint. Optimising building infrastructure, purchasing green electricity and improving the supply chain are big challenges to impact energy efficiency, but simpler actions can be implemented easily and yield positive impact of imaging carbon footprint. Changing the wait period between standby and turning off reporting stations from four to one hour can reduce more than half of the energy consumption. Centralised automatic switch off of computers can be managed through software implementation, and saved 500’000£ in the Imperial College Healthcare NHS Trust where the experiment took place. In the study, CT and MRI accounted for 4% of the hospital consumption, 44% of which came from cooling systems. 66% of CT energy consumption was during idle state and 33% of MRI energy consumption was during system-off state. The implementation of a dashboard display shared with the staff yielded good results and engaged the healthcare community.
Energy waste in CT/MRI can be reduced when 3 main levers are actioned:
- Industry
- Development of sleep mode/stand-by/power save modes
- Heat-waste recovery from cooling systems
- Refurbishment of old scanners to upgrade rather than new build
- Governmental
- Possible EU directive could mandate energy savings in healthcare
- European Coordination Committee of the Radiological, Electromedical and Healthcare IT Industry
- Departmental:
- Ensure smooth and efficient workflows to reduce on time but not in use
- Turn off out of hours
- Departments of the future will monitor energy consumption
- Envision energy dashboard
- Plan lay-out of scanners to share cooling systems
Physical waste management is also an area of focus, as contrast bottle, giving set and residual contrast are often all being disposed of in the incineration sharps bin, leading to a high carbon footprint and financial cost for disposal. Contrast bottles can be recycled, not all part of the giving set should be incinerated. Environmentally-friendly radiology dept should be required in future; small changes may make a big impact cumulatively and are easy to implement: Auto-shut down PACS, projectors and computers; Motion sensitive lights, LED; Care with water usage and air conditioning/heating; Biodegradable cups.
Departments need to start measuring and evaluating their performance against environmental impact, as we do with clinical audit for diagnostic accuracy, waiting times and turnaround times. A simple framework plan could be to measure consumption, monitor impact of saving measures, and count the savings, through ad-hoc dashboards and KPIs.
How circular economy and sustainable practices can be applied to healthcare?
The healthcare sector is one of the largest industries worldwide and a major contributor to the climate crisis with the sector's carbon footprint equivalent to 4.4% of global net emissions. In her lecture, Ana Luísa Ferreira Soares (Portugal), defined the concept of circular economy and identified the different dimensions across which sustainable practices can be applied by healthcare professionals. Circular economy (CE) aims to maintain the value of resources in the economy for as long as possible, using efficiently the resources through waste minimisation, reduction of primary resources, and closed loops of products.
Circular economy practices related with radiotherapy would be:
- Waste separation according to the signposting
- Take into account/reduce the table paper
- Reduce WC hands paper
- Reduce plastics / Avoid single-use plastic, devices
- Reduce single-use materials, clothes, disposable shoe covers
- Reuse materials, devices ... (e.g. bolus, vacuum materials/mattresses)
- Reuse the water bottles
- Paperless workflow departments
Individual practices can also fall in the scope of circular economy:
- Telemedicine
- Use of bicycle, public transports and car pooling
- Reduce transportation distances from healthcare waste and food
- Patient's environment-friendly transportation
In order to maximise the adoption of these practices, a behaviour change has to occur through staff training to raise awareness. Management team should foster and encourage engagement in sustainable practices and report on the environmental performance of the organization against environmental objectives and goals.
Low-value imaging can be a sizeable waste of resources
Sustainability also comes in the form of not performing imaging services when the value to the patient treatment is not clear. Elin Kjelle (Norway) goes over a detailed overview of what’s to gain when reducing low-value imaging.
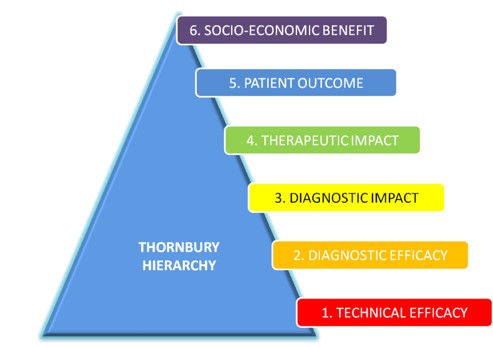
Following the Thornbury hierarchical model of efficacy, value in imaging comes in six different levels, from technical efficacy, all the way up to socio-economic benefit.
84 different typical low-value procedures in imaging were identified, including atraumatic pain, routine imaging (Minor head injury, trauma, thrombosis, kidney stone) and follow-ups for fractures and cancers. The magnitude of the wasted resources is important: with 3.6 billion examinations per year and 20-50% of imaging being of low value, at an average cost of $92/examination, the worldwide low-value waste would amount to $66-166 billion per year.
Drivers explaining the amplitude of this unnecessary procedures are the exaggerated technology beliefs of patients, referrers knowledge and competence and the guidelines radiologists follow.
The Kjelle et al. study in BMC Health Serv Res identified various levers to decrease low-value imaging, the most effective being:
- Required action from referrer
- Feedback to referrer
- Implementing a clinical decision support system
- Guidelines implementation
The best results came from a multicomponent intervention with education.



























