In an interesting session today at #ISICEM24, Dr Annika Reintam Blaser, an intensivist at Lucerne Cantonal Hospital in Switzerland, discussed future research on optimising feeding for critically ill patients. She highlighted the accumulating evidence over the past 15 years suggesting that feeding might have harmful effects on critically ill patients.
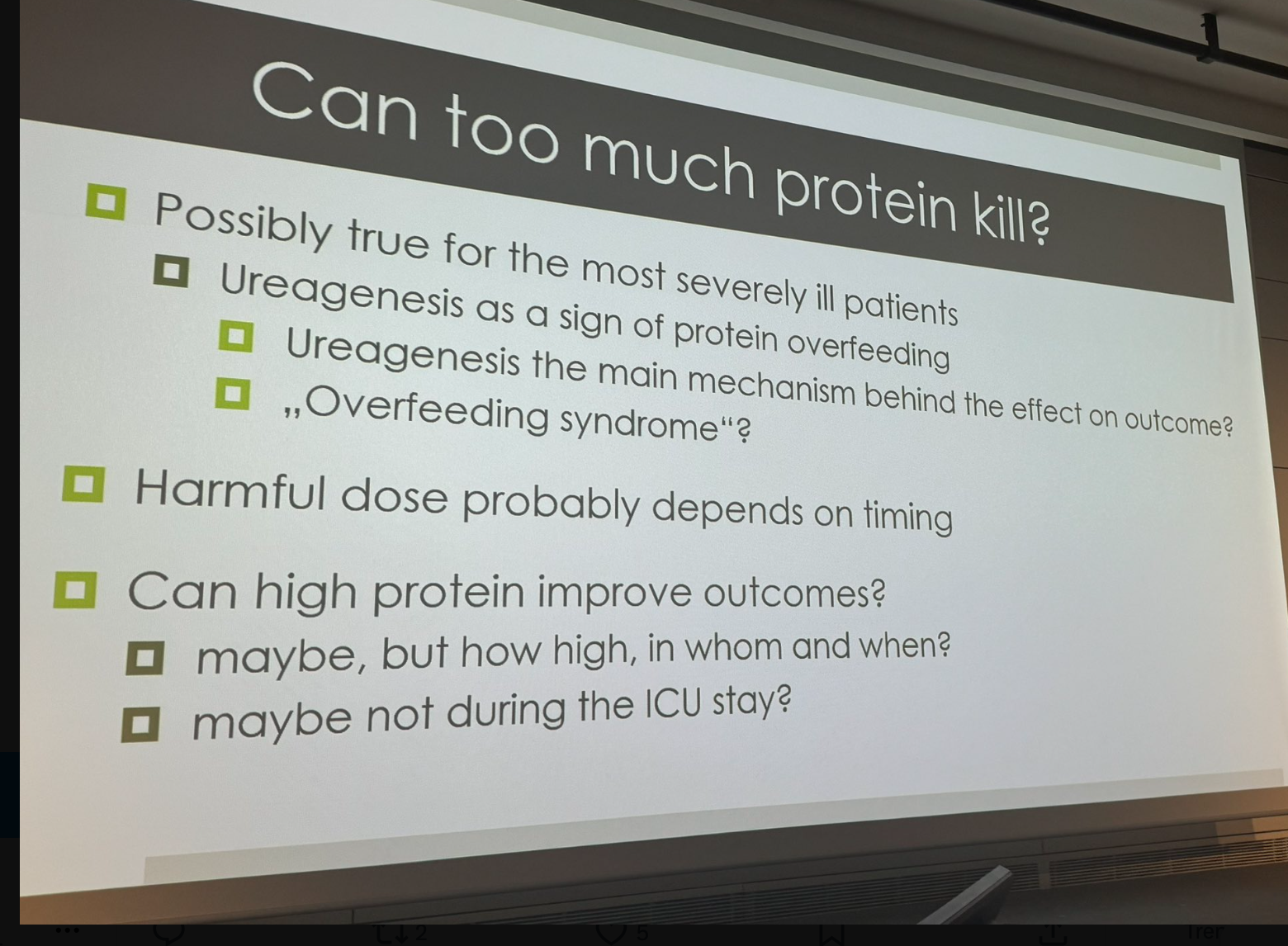
Dr Blaser challenged the intuitive belief that more nutrition is better for critically ill patients, citing numerous studies that have shown otherwise. She emphasised that early feeding might be harmful and suggested shifting the research focus away from early ICU feeding, which has been extensively studied, to investigating later stages of nutrition provision beyond the acute ICU period.
The complexity of nutritional intervention in ICU patients is further complicated by the transition to general wards, where undernutrition remains a concern. One promising study, EFFORT, conducted on non-ICU medical patients, indicates positive outcomes with sufficient nutritional support. Other studies, including EPaNIC and NUTRIREA 32, show similar findings. There is a need for a deeper understanding of when and how to provide optimal nutrition because the body's natural survival mechanisms may not prioritise nutrition during extreme situations.
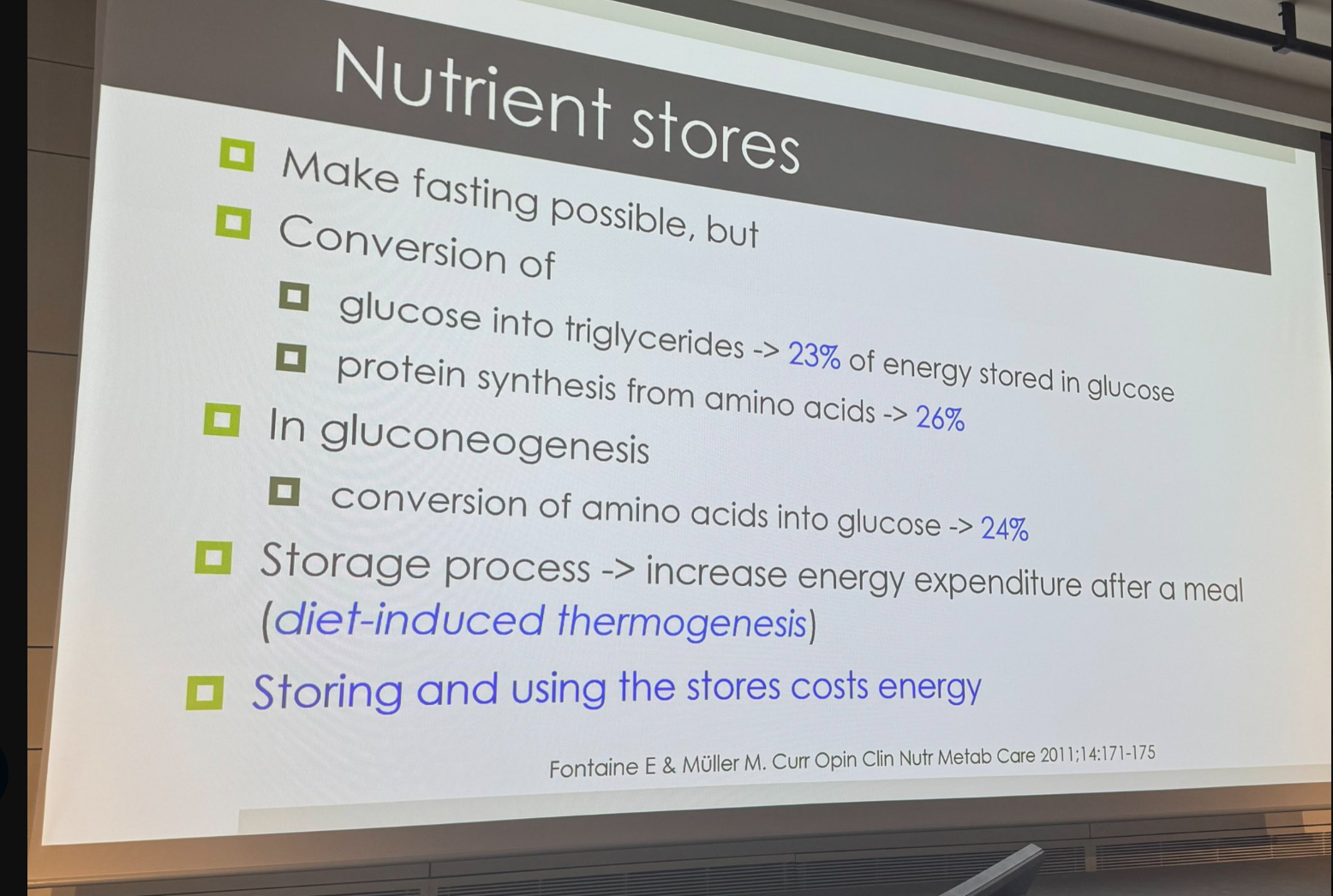
There is also a need for advancements in measuring metabolic processes to optimise nutrition for critically ill patients. This can be achieved by developing a "metabolic monitor" to tailor feeding regimens based on individual metabolic needs, which is a major limitation of current standardised approaches. While indirect calorimetry can measure resting energy expenditure, it lacks the ability to assess endogenous energy production and nutrient utilisation, particularly in the acute phase. Hence, it is necessary to understand these metabolic dynamics to improve patient outcomes in intensive care settings.
It is equally important to understand energy dynamics in critically ill patients. Even in severe illness, patients continue to produce internal energy, which can lead to overfeeding if additional external energy is provided through nutrition. There is a need to measure endogenous energy production to avoid overfeeding and optimise nutrition. While guidelines recommend progressively increasing feeding during ICU stays, uncertainties remain regarding the timing and duration of such adjustments.
Overall, Dr Blaser emphasised the need for ICU physicians to shift their perspective and consider the longer-term implications of nutrition beyond the acute phase.
Source: ISICEM
Image and Slide Credit: ISICEM


























