HealthManagement, Volume 23 - Issue 3, 2023
Fast growing integrated health care and social organisation present a challenge due to the increased complexity of its operations.To manage the services at scale while remaining a patient-centred organisation, new tools need to be incorporated to assist members in their decision making and care quality measurement.
Key Points
- Defining a strategic map enables a link between the strategic plan and the Balanced Score Card (BSC) and to be used as the common language to achieve the mission of the organisation.
- Using a bottom-up strategy when defining KPIs (Key Performance Indicator) for a BSC allows not only the involvement of all the internal stakeholders in the BSC design, but also to understand that is a communication tool more than a control mechanism.
- BSC use in healthcare institutions should give special importance to the patient dimension and the care quality indicators.
- A BSC should be a dynamic tool and adapt according to the organisation needs.
Introduction
Fundació Aspace Catalunya is a non-profit entity that is part of the Catalonian Health Public System and provides health, social, and educational services.
We give continuous care each year to more than 2000 people with cerebral palsy and neurodevelopmental disorders, with high complexity in terms of health, where 72% have co-morbidity with serious mental health pathologies.
The organisation has experienced an exponential growth in recent years and has ventured into new initiatives in the field of academic research, innovation, and partnerships with other entities to carry out joint projects.
This, combined with the increased level of complexity in both direct care and the different operational processes of the institution, adds difficulty to the already challenging task of monitoring the performance of the organisation and making strategic decisions guided by data.
The organisation is not only a complex agent of its own but it is also an active participant in a CAS (Complex Adaptive System). There is a close interconnection with other elements of the Catalonian Health Public System as well and we actively adapt our behaviour to influence them in a positive way and be influenced by these in a continuous feedback loop.
Therefore, it is necessary to add new tools so as to allow us to manage our services, not only in the quantity of care and work done, but also in the quality of what we offer in the different areas we cover.
Performance measurement has been defined as the process of “evaluating how well organisations are managed and the value they provide to customers/patients and other stakeholders” (Kollberg 2003). It is important to take reliability into account when developing performance measures, how they will be perceived by professionals and users, and whether they add value to the services we offer.
When measurement is done properly, it can motivate professionals to improve, illustrate the true performance of the system, and identify the impact of any changes in real-time. However, when this is not done correctly, it can have an impact on the morale of the professionals and lead to a culture of blame in which personnel follow objectives at the expense of patient care” (Aidemark 2001).
Therefore, measuring performance in healthcare services is often perceived as a controversial initiative, although no less necessary. As is well known, it is easier to manage what we can measure.
To partly meet this challenge, the Balanced Scorecard (BSC) has been proposed as an instrument that allows us to analyse and organise data. It allows for the extraction of knowledge in order to make better decisions supported by data, and improve the organisation’s ability to implement its strategy.
Balanced Scorecard
According to Kaplan and Norton, the BSC is designed to support and fulfill the company’s vision and overall strategies. Their version of the BSC, presented in 1992, contains four different perspectives: financial, customer, internal processes, and learning and growth. These perspectives represent how the company is viewed by the most important stakeholders: shareholders, management, customers, and employees.
Balanced scorecards applied to healthcare organisations have been used to address a variety of challenges ranging from improving the quality and safety of care, guiding public or private healthcare services administration, and supporting the profitability or competitiveness of healthcare companies in market systems.
BSC Design Process
Taking into account the particular characteristics of the Fundació Aspace Catalunya, the Kaplan and Norton BSC model has been used with some modifications, incorporating some of the contributions suggested by different examples.
In particular:
- Develop a strategic map that serves as a link between the Strategic Plan and the scorecard.
- Begin the process by providing sufficient context to the responsible professionals, so that they can understand the objective and importance of implementing a Healthcare Scorecard.
- Give equal importance to all perspectives, but giving special importance to the patient dimension.
- Take into account quality indicators.
- Use a bottom-up approach, involving healthcare professionals in the design of the scorecard, as this is better suited to the entity’s work culture.
- Use the scorecard as a common language to fulfill the entity’s mission.
- Develop a Healthcare Scorecard with key perspectives and indicators in a first stage. In a second stage, identify the need to develop second level scorecards.
To achieve this, a scorecard development methodology was followed, consisting of the following phases:
1. | State of the art study |
| Before embarking on the task of defining the BSC, it was important to conduct a thorough study of the available literature and the different BSC formulas used in healthcare organisations of countries with similar healthcare systems as ours. | |
2. | Preparation |
The next step was to prepare a presentation explaining what the BSC, Strategic Map, and KPIs (for professionals who were not familiar with these concepts) consisted of, along with the objectives we wanted to achieve by implementing this tool and the time we had available to do the work. At this point, we also developed the interviews and questionnaires to be used in meetings with the different department heads (middle management). These were the tools to determine what were the best indicators (KPIs) that would work and add the most value to their respective services. For this, a Strategic map was defined in order to describe the strategy and serve as a guide for professionals, to determine if the performance metrics chosen during the interviews were aligned with the institution’s strategic plan. | |
| 3. | Focus group interviews and workshops |
| Since the BSC followed a bottom-up approach, it was the professionals from the different levels who determined the KPIs to be used in each service. This was achieved by conducting interviews with them and discussing what was the most important to measure in order to improve our processes and offer a better healthcare service to our patients. | |
| 4. | Executive workshops for bottom-up KPI validation |
| Although the BSC design followed a bottom-up model, the KPIs defined by middle management were validated by the executive team. This was necessary to ensure that the measures were aligned with the organisational strategic plan. | |
| 5. | Healthcare CMI design |
Once the KPIs were formulated and validated by the executive team, the BSC could be designed to meet the needs and objectives of the organisation in the knowledge that the KPIs to be measured were defined by professionals who are closer to patients and thus aware of their needs. | |
| 6. | Pilot testing of KPIs associated with a specific service |
| To adjust details about the design and future implementation of the BSC in Healthcare, we decided to conduct a pilot test. | |
| 7. | Review by management |
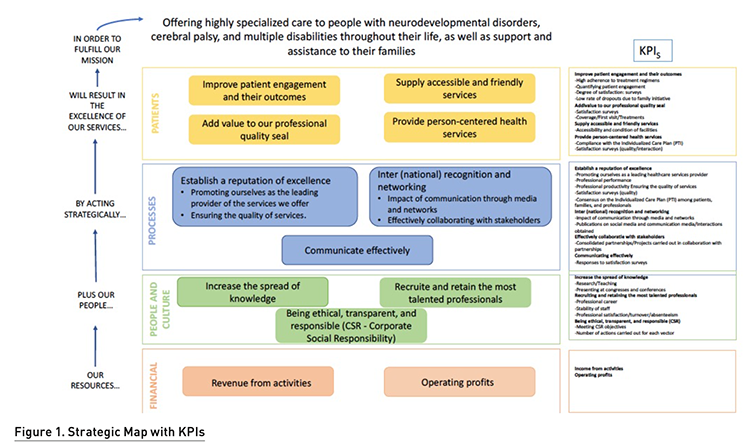
| The last phase was to review with the management team both the Strategic Map and the BSC with the obtained KPIs. The resulting strategic map and their KPIs are shown in the following Figure 1. |
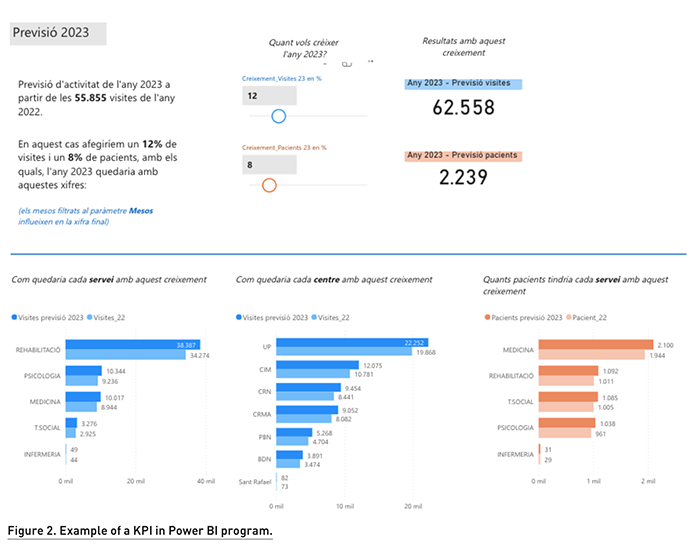
As mentioned above, we have started the implementation of our BSC using a Business Intelligence (BI) software suite. This allows us to extract knowledge from the data and have predictive models that allows us to anticipate for changes and make data driven decisions. As an example, Figure 2 shows an estimation of how much the organisation will grow by using the historical data to interpolate the future value.
Conclusion
The development and subsequent implementation of the BSC represents a real and important need within the organisation, considering the growth it has experienced in recent years, and is aligned with the new Strategic Plan for the next 5 years.
The purpose of creating and using the BSC in Health at the Aspace Catalunya organisation has been as a tool to properly and effectively implement the organisation’s strategy. It is envisioned to be used more as a communication tool rather than a control tool.
We understand and are alert to the fact that our BSC should be dynamic and change according to the organisation needs.
Conflict of Interest
None.
References:
Aidemark LG (2001) The Meaning of Balanced Scorecards in the Health Care Organisation. Financial Accountability & Management. 17(1):23 – 40.
BohmLacailleSpencer, et al. (2021) Scoping review of balanced scorecards for use in healthcare settings: development and implementation. BMJ Open Quality. 10(3):e001293.
Carnut L, Narvai PC (2020) A Meta-summarization of Qualitative Findings About Health Systems Performance Evaluation Models: Conceptual Problems and Comparability Limitations. INQUIRY: The Journal of Health Care Organization, Provision, and Financing. 57.
Gonzalez-Sanchez MB, Broccardo L, Pires AMM (2018) The use and design of the BSC in the health care sector: A systematic literature review for Italy, Spain, and Portugal. The International Journal of Health Planning and Management. 33(1):6-30.
Grifith, JR (1994) Reengineering health care: Management systems for survivors. Journal of Healthcare Management/ 39(4):451.
Kaplan RS, Norton PD (1991) The Balance Scorecard-Measures That Drive Performance. Harvard Business Review. 70(1):71-79.
Kaplan RS, Norton PD (1993) Putting the Balanced Scorecard to Work. Harvard Business Review. 71
Kaplan RS, Norton PD (1996) The balanced scorecard: translating strategy into action. Boston: Harvard Business School Press.
Kaplan RS, Norton PD (2001) The strategy-focused organization: How balanced scorecard companies thrive in the new business environment. Harvard Business School Press.
Kollberg B (2003) Exploring the Use of Balanced Scorecards in a Swedish Health Care Organization. Doctoral Thesis. Linköping University, The Institute of Technology. ISBN 91-7373-741-0. ISSN 0280-7971.
Martin CM (2018) Complex adaptive systems approaches in health care - A slow but real emergence? Journal of Evaluation in Clinical Practice. 24(3): 601-605
Rogers H, Silvester K, Copeland J (2004) NHS Modernisation Agency's way to improve health care. BMJ (Clinical research ed.). 328:463.
Zelman WN, Pink GH, Matthias CB (2003) Use of the balanced scorecard in health care. Journal of Health Care Finance. 29(4):1-16.


















