ICU Management & Practice, Volume 23 - Issue 4, 2023
Digitalisation is ultimately the driving force behind digital transformation. It will take us from a reactive healthcare system to a proactive one that focuses on prediction and prevention.
Introduction
The digital transformation has left a few things untouched in recent years, radically changing healthcare management for citizens, professionals, and public health departments. In the medical field, this digital transformation process is a far-reaching concept that extends to a wide range of situations, which are fundamentally based on the use and processing of digital data.
The concept of digital health is often thought of as being solely related to technological advances (electronic prescriptions, mobile applications, etc.), but in reality, its scope is far broader and entails a paradigm shift. Here, we apply the idea of digital density, which expresses the amount of digitalised data in a system. When the digital density value of a system is equal to 1, this means that all the data is digitalised, implying an impending change in the sector.
Hence, we can say that we are currently undergoing a digital revolution, one that follows both the agricultural revolution, where land was the underpinning value, and the industrial revolution, where the transforming element was energy. Today, value derives from data, and the changes we are experiencing occur at an everincreasing speed, so we often speak of technological acceleration.
With this backdrop, the Spanish National Health System has been establishing lines of action to foment the digital transformation of the country’s healthcare system. Based on recommendations from the World Health Organization's digital health platform and current European programmes, these actions include the development of digital health solutions yielding added value, harnessing of data, and the creation of knowledge through artificial intelligencebased analytics systems. Other lines focus on digital training for professionals, an important aspect of this revolution. All of this must be based on a hybrid cloud architecture in a shared-operability environment where compliance with stringent cybersecurity standards and the legislation in force is assured.
This digital transformation extends, of course, to intensive care units and other hospital units. Here, it begins with the technological improvement of a centre’s processes and the growing use of wearables and other devices for the treatment and monitoring of patients, whether remote or in situ. These aspects are already present to some degree in most units, but we will see more of this in the near future. Next, the integration of data and processes in clinical record programmes and other digital tools will be paramount and will culminate in the large-scale storage and advanced analysis of data (Big Data), leading to the execution of artificial intelligence (AI) projects. This kind of digitalisation is ultimately the driving force behind the digital transformation and will take us from a reactive healthcare system to a proactive one that focuses on prediction and prevention.
In our field, one of the main objectives of the digital transformation process is the design and development of tools, scores, and algorithms. Some of these allow us to quantify, express, and even predict hospital occupancy and case complexity, helping to efficiently organise operations and human resources. Others stratify certain patient risks and may even help us anticipate their clinical evolution. In general, these tools allow us to implement healthcare strategies and treatments that can alter the natural course of a disease by employing a more global approach. They are designed to support, and not replace, healthcare professionals in decision-making tasks, thus shortening wait times and minimising risks by offering a higher level of information and more in-depth analyses; in short, they add value.
Next, we will highlight the key points to consider in a digital transformation process based on our experience in Hospital Sant Joan de Déu (Barcelona).
Data Sources
Data has traditionally been generated by medical professionals entering information into patients’ clinical records. However, the emergence of devices, wireless tools, sensors, and other technology increases the quantity, quality, and variability of data (the so-called unregulated data). Moving beyond merely clinical data, new systems will be able to receive inputs and analyse data stemming from different sources, such as genomics.
The data obtained in an intensive care unit has characteristics that make it ripe for the development and execution of projects based on data management. Huge volumes of extremely accurate data are generated here at very high speeds, and yet they are varied as regards their type and origin, all of which make them very valuable. When working with data, it is important that we not forget that a series of barriers related to the quality, governance, anonymisation, variability, terminology, and conceptualisation of data must also be addressed. Data can be quite heterogeneous in its behaviour and come from many different platforms. The vocabulary used to describe it can also be quite variable, leading to uncertainty and a lack of consensus regarding specific concepts in data management. For this reason, it has been necessary to ensure internal and external interoperability through the creation of data catalogues and business glossaries based on standards.
In intensive care units, it is imperative that the data available be used as optimally as possible to benefit the patient when it comes to safety, quality of care, and the diagnostic and therapeutic process. Everything mentioned above makes an intensive care unit a natural and, consequently, ideal place for executing a data management project.
Clinical Applications
With data analytics drawing from large datasets as a basis, artificial intelligence solutions can be developed to undertake the actions that a human being would naturally perform but more quickly and efficiently.
These solutions can be divided into four fields of application:
- Solutions to improve the patient-healthcare provider relationship (i.e. patient portals, intelligent assistants, etc.)
- Discovery solutions
- Solutions that support decision-making (i.e. image analysis, risk stratification scores, predictive algorithms of poor clinical evolution, etc.)
- Solutions that support management and operations (i.e. operational panels, smart hospital systems, etc.)
During our intensive care unit’s architectural, technological, and digital transformation process, we have created solutions in each of these fields.
Digitally Transforming a Paediatric Intensive Care Unit
Hospital Sant Joan de Déu, located in Barcelona (Catalonia, Spain), is a highly specialised maternal and children’s hospital that emphasises a multidisciplinary approach. The hospital has 320 beds and is one of the most important paediatric centres in Europe, especially in neurosurgery, cardiovascular surgery, and comprehensive care for paediatric oncology patients.
In 2018, the hospital's new paediatric intensive care unit was built, which entailed an architectural, technological, and digital revolution.
Prior to that, the unit had a semi-circular distribution with a centralised nature, similar to other intensive care units built in Spain in the 1970s. It had a surface area of 500 m2 , hosting a total of 18 beds. However, the bays were open, with no physical separation between them, and the area had a single surveillance post equipped with a monitoring centre, essentially reducing space for caregivers.
In the new unit, which currently has 28 beds and around 1500 admissions per year, the surface area was quadrupled to 2200 m2 , moving to a decentralised model with closed bays and thus increasing usable space for caregivers. The new model is an essential part of the paediatric therapeutic and recovery process but also serves to increase the visual and auditory privacy of patients.
It is a highly technologically advanced unit, equipped with electronic clinical record systems and semi-protocolised pharmacological prescription systems based on pathology and patient weight. It also has an intelligent drug management and dispensing cabin and continuous infusion pumps with an inserted library of standard concentration solutions. Additionally, the unit is equipped with operating and isolation bays, patient monitoring systems, and state-of-the-art therapeutic devices (continuous extrarenal purification, plasmapheresis, and ECMO systems), all of which send continuous data to external systems.
This process entailed an inevitable paradigm shift that created stress, healthcare fatigue, and resistance to change, but it was ultimately successful and well-received by the team. For the viability of the project, the inclusion of remote systems was essential. First, a system was developed based on establishing a matrix of alarms that are activated when a single parameter changes. Mobile devices were introduced that allow alarms to be transferred to the nurse when they are not physically in front of the device or monitor where the alarm is coming from. The system allows for alarms with different light and sound features depending on the criticality of the alarm. These are escalated in a predetermined manner to other professionals to ensure that all alarms are correctly attended to, increasing patient safety
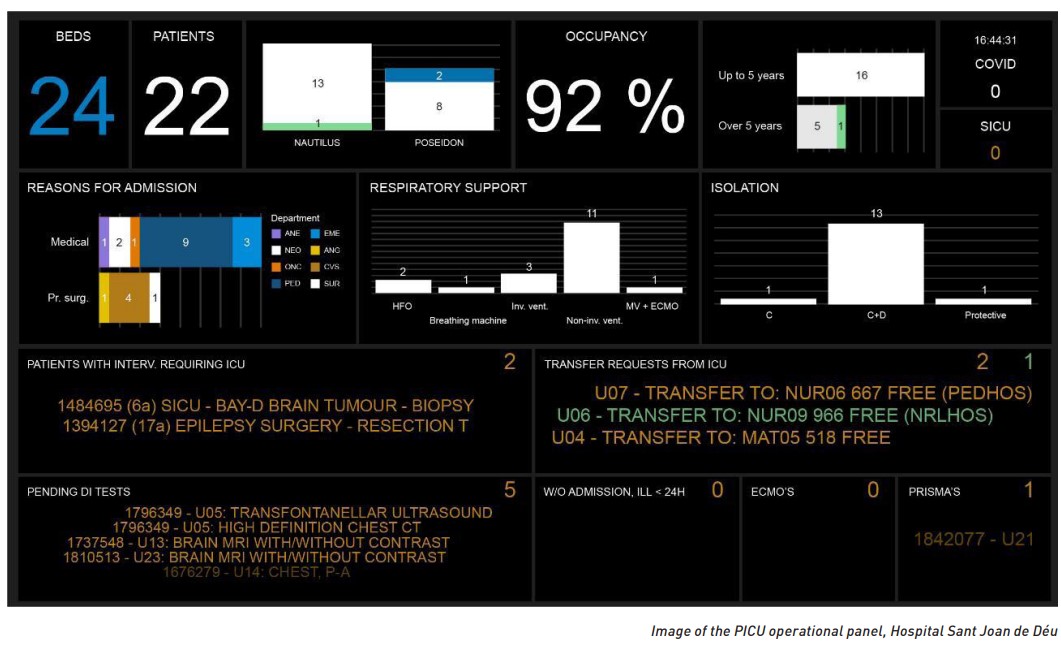
An operational panel was created for managing data generated in the different systems of the unit. It extracts data in realtime through analytics software, which has a dashboard displaying occupancy, a forecast of patient admission/discharge flows, and the complexity of the patients hospitalised in the unit. Therefore, it is also capable of showing human resources requirements (from cleaning staff to nursing and medical care staff) in near real-time and helps streamline patient movements between the PICU and the different areas of the centre.
Traditionally, early warning scores (EWS) using vital signs and risk indicators have been proposed to assess children at risk of clinical deterioration to intervene quickly to reduce the impact of deterioration and risk of death among these patients. However, EWSs are based on measurements performed at a single time point without incorporating trends or prior patient information. Moreover, some of these measurements rely on subjective assessment, leaving them susceptible to different interpretations. All these limitations could explain why the implementation of EWSs in high-resource settings has failed to show a significant decrease in hospital mortality. Using artificial intelligence-based algorithms, we could automatically integrate data from different sources and nature to predict a patient’s risk of deterioration.
In the test environment, we now have several algorithms to improve the identification of paediatric patients at high risk for clinical deterioration following cardiac surgery (Garcia-Canadilla et al. 2022), including a bronchiolitis score and a predictive score for anticipating and diagnosing sepsis.
In 2020, our sepsis score (PESERS), which is based on the transformation of the Catalonian sepsis code to a quantitative score, was validated in our children’s hospital (Solé-Ribalta et al. 2022). The PESERS score was found to not only improve the screening of sepsis but was also shown to be useful in predicting the evolution thereof. The automation of this score through the instant capture of a patient’s variables allows for a continuous calculation of the score, utilising a traffic light alarm system to promptly alert the required healthcare professional. Similarly, the automation of the Bronchiolitis Score of Sant Joan de Déu (BROSJOD) (Balaguer et al. 2017) makes it possible to objectively and continuously categorise the severity of bronchiolitis episodes, allowing therapeutic decisions such as respiratory support escalation or patient transfer to be made.
Today, what we have are scores that tell us what is currently happening to the patient, but in a second, future phase, we intend to apply machine learning tools so our algorithms can learn, increase in complexity, and improve their predictive capacity. This, along with the development of new algorithms, will help us detect the events we want to identify, even before they occur.
The Cortex Project
The digital transformation process undertaken at Hospital Sant Joan de Déu gave rise to something unprecedented - the Cortex project. We have seen that today’s healthcare centres simultaneously carry out multiple processes and procedures where a myriad of operational information systems coexist, all generating large volumes of data. Hospital management teams must be able to carry out a posteriori analyses of these data to align their efforts with the needs and characteristics of a new reality in healthcare, one in which active patient participation is just another part of the care process, decision-making cycles are increasingly shorter, and quality standards are increasingly demanding. As highlighted by the COVID pandemic, having reliable, stable, and, above all, real-time information is a critical factor in today’s healthcare management.
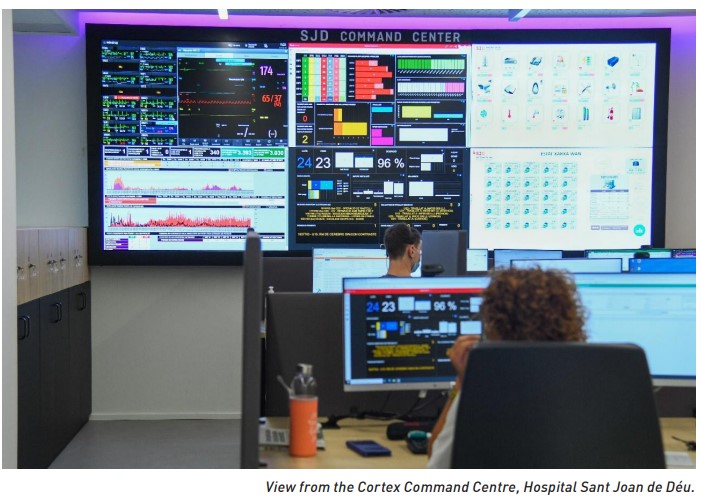
With this in mind, Cortex was launched as the centre’s global monitoring station, with a proactive and predictive overview, in which three large areas converge in a proactive and predictive manner: E-care, Command centre, and Contact centre.
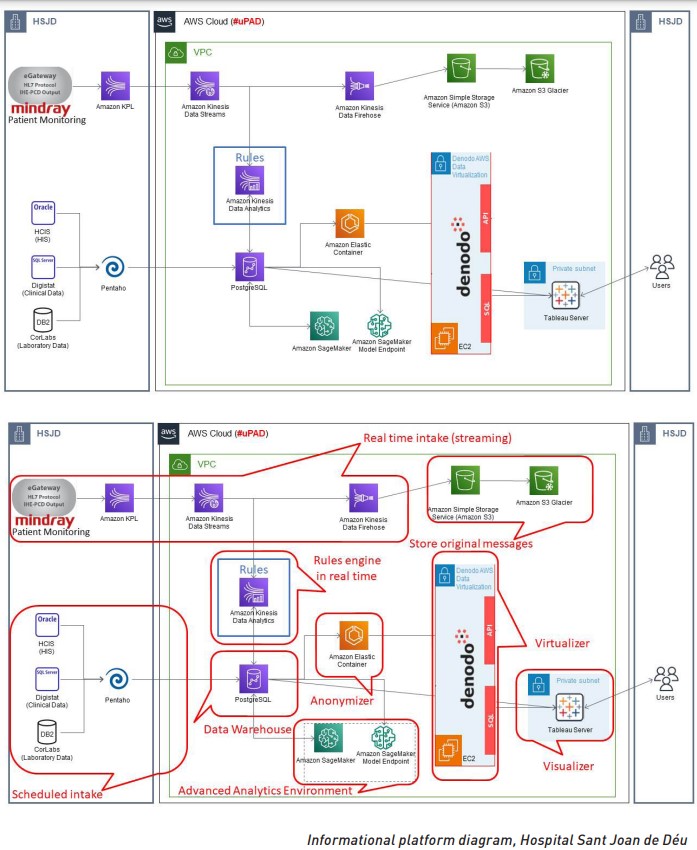
In order to carry out this project, one of the actions performed at Hospital Sant Joan de Déu was defining a global data ecosystem, including all the data generated by the systems present in the hospital, located in a cloud system. It is essential to have a Data Control Office in charge of data management, governance, and ethical use in line with current regulatory systems. This is now a reality, and the data ecosystem feeds the Cortex project, providing valuable inputs.
Taking a look at the different areas of Cortex, in the E-care area, we can find the remote monitoring systems and E-care tools, which are defined as those rules or algorithms that allow for stratification by clinical status or the risk of disease evolution for a particular pathology. This helps us execute healthcare or therapeutic strategies in a manner that can alter the natural course of a disease. The main goal is to anticipate and improve decision-making, moving from our current reactive medicine to preventive and proactive medicine.
Next, the Contact Centre area is a more administrative part that manages the information and contact with all of the centre's patients. This is done through a multi-channel service that covers different forms of communication between the centre and its contacts based on Customer Relationship Management (CRM) software. It is a virtual proximity model that uses the personalisation of care to improve the quality of responses, especially since it is sometimes the first point of contact with the centre. Overall, it helps anticipate the needs of the patients and families and provides support during the hospitalisation process.
Lastly, the Command Centre area is intended to manage the operations of the hospital, much like the air traffic control tower of an airport. It represents a comprehensive change in how hospital flows are managed, using process reengineering and a technological platform similar to that found in the centre of operations. For this, we have designed tools that show useful and near-real-time information coming from sensitive areas (the PICU, surgical block, hospital ward, etc.) and algorithms for the control and management of flows, human resources, and materials in the hospital. These tools display their results on what are called operational panels, which allow events to be anticipated so that responses can be organised in advance; it is also useful for decreasing wait times and improving the overall patient experience.
Conclusion
In conclusion, the digital transformation that our centre has undergone through the implementation of this project has allowed for better organisational foresight, especially in critical areas, along with more efficient processes, resource management, and hospital flows. This endeavour has and will continue to improve the detection of urgent situations, setting the stage for better predictive algorithms and the harnessing of AI in the service of patients and medical professionals. It is thus incredibly helpful as a decision-making aid at the centre, improving care and support for the patients and their families.
For a project like this to be successful, it is key to have transparent, accurate information that is available in real-time and to have a well-defined data management and governance strategy. As we develop and expand this cutting-edge venture, we hope to showcase what can be accomplished and serve as a blueprint for other centres wishing to implement a similar project.
Conflict of Interest
None.






























