HealthManagement, Volume 23 - Issue 4, 2023
The health sector occupies a unique position as a contributor to carbon emissions but also a sector that pays for the damages of climate change through health impact. By decarbonising, the health sector has a dual opportunity to meet the challenges and benefit from sustainable changes. For this, a systems approach to change is needed that considers the most vulnerable and marginalised, ensuring a just transition.
Key points
- Decarbonising the health sector has the opportunity to not only help mitigate and adapt to climate change but also to improve public health and decrease the current and future burden on health systems.
- By rising to the challenges of decarbonisation and sustainability, the health sector will decrease its impact, and will also stand to gain from a number of co-benefits, inside and outside of public health, and act as an advocate to other sectors.
- Decarbonisation works hand in hand with health promotion and disease prevention, and efforts to improve population health will positively impact climate footprint.
- Technological improvements will not be enough to prevent climate; systems change is needed to move away from models based on fossil fuel extraction and consumption.
- International collaboration and support are essential in adapting to change and building provision, capacity and resilience.
The Healthcare System and Carbon Footprint
Amid the pressing global issue of climate change, a comprehensive effort to decarbonise every facet of society has gained urgency. Surprisingly, the health sector often evades attention in climate discourse despite its sizeable contribution to carbon emissions. If ranked as a country, the health sector would be the fifth-largest carbon dioxide emitter, accounting for 4.4% of global carbon emissions (Health Care Without Harm and ARUP 2022), which accounts for more than the aviation and shipping sectors combined (Gabbatiss 2019). Carbon footprint varies across different systems; the average per capita health carbon footprint in 2014 (in Organisation for Economic Co-operation and Development (OECD) countries, and China and India) was 0.6 tonnes of carbon dioxide (tCO2) per capita, varying between 1.51 tCO2 per capita in the United States, and 0.06 tCO2 per capita in India (Pichler et al. 2019). This emphasises the imperative of health sector decarbonisation, not only for mitigating climate change but also for bolstering the sector’s resilience against climate-induced health and environmental crises. Systems thinking is needed to tackle such complicated problems.
In the context of this paper, the health sector refers to not only acute care facilities but also the structures for health protection and prevention, as well as organisational and social structures working towards health, such as disability and elderly care.
Climate change is a justice issue, and the disparities between different populations highlight the inequity and inequality in health status. The Global North has contributed the most to a changing environment, yet it is the Global South that is suffering and will suffer more greatly from climate events (Deivanayagam et al. 2023; Hickel 2020; Intergovernmental Panel on Climate Change 2023). The Global South contributes the least to global emissions, yet they often have less capacity for health systems, technological, economic and infrastructure resilience to weather shifting climates (Intergovernmental Panel on Climate Change 2023). For example, the impacts of flooding on health sector operations and public health status in low-lying Pacific Island nations, including infectious disease risk (Paterson et al. 2018; WHO 2017), or the effects of prolonged drought in a sub-Saharan nation (Masih et al. 2014), stand to significantly impact health. The Global North need to not only decarbonise but also assist in boosting the resilience of nations that are bearing the brunt of the climate crisis, despite their negligible contribution to its cause.
The health sector’s substantial carbon footprint stems from a number of factors in different scopes of emissions. Scope 1 emissions are related to the direct use of sector-owned or controlled resources, which encompass waste management, transportation, and on-site fuel combustion sources, such as boilers and gas appliances (Health Care Without Harm and ARUP 2022). Scope 2 emissions are indirect and come from the consumption of purchased energy from a utility provider, including electricity, heat and cooling (Health Care Without Harm and ARUP 2022). Scope 3 is by far the largest contributor to the health sector’s carbon footprint, accounting for, on average, 71% of the footprint (Health Care Without Harm and ARUP 2022). These emissions are indirect and arise principally from procurement, goods and materials distribution, transportation including patient commuting, pharmaceuticals (including medical gases), construction, waste generated in operations (such as catering), and use of products by patients, all when not directly under the control of the sector (Health Care Without Harm and ARUP 2022).
Adding to this, the health sector’s large carbon footprint paradoxically aggravates a range of health issues. The system will be burdened with further costs through increased service demand, escalated stress, and damage to infrastructure and social systems. Climate change poses an increasing risk to global public health and disease management, leading to a greater incidence of morbidity and mortality due to direct and indirect causes. Direct causes will include infectious disease and pandemic risk, as well as direct environmental stressors, such as heat, severe weather and flooding, while indirect causes will include decreased water security, distorted and strained food systems, forced migration and negative mental health impacts, among others (European Public Health Alliance 2023; WHO 2019). The effects of these proximate causes are unevenly felt across society and by both non-vulnerable and vulnerable populations. Vulnerable populations include older people, children, pregnant women, those with a mental illness or an underlying condition like respiratory disease and diabetes, and people of lower socioeconomic status (Guivarch et al. 2021). Thus, decarbonising the health sector presents a dual opportunity: curtailing its contribution to global carbon emissions, thereby reducing its public health impact and enhancing the resilience of health services to climate change-induced health threats.
According to the WHO, the health sector plays a crucial role in spearheading the necessary global transformation needed to meet the challenges of climate change and having an opportunity for public health prevention in terms of climate change related risk (WHO 2019).
Strategies for Healthcare Decarbonisation
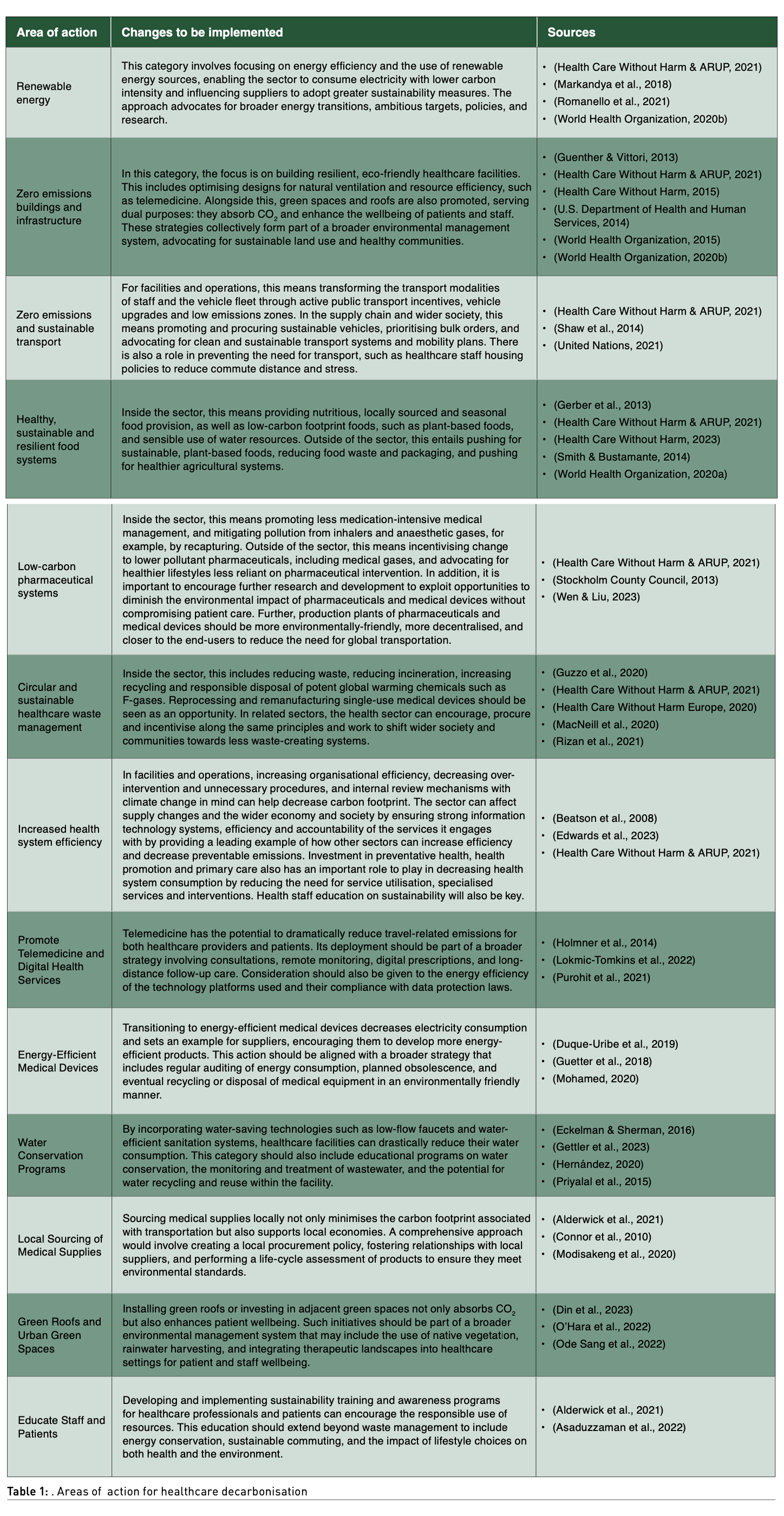
To drive and accelerate the decarbonisation of the health sector, several strategies have been developed, some of which are currently being deployed across various settings. As extensively outlined by Health Care Without Harm in a collation of recommendations from the World Health Organization and World Bank, these strategies fall into three areas: (1) facilities and operations, (2) supply chain, and (3) the wider economy and society (Health Care Without Harm and ARUP 2021). Table 1 shows an overview of actions in these areas. To achieve a more comprehensive scope, additional areas of action from various sources have been integrated, enhancing the overall coverage of healthcare decarbonisation.
By implementing these recommended changes in different areas of action, the healthcare sector could stand to drastically reduce its environmental and climate impact. In this process, however, the healthcare sector can also stand to profit from a range of related co-benefits for the health and wellbeing of populations, as well as its own operations, efficiency and resilience. With healthcare staff being among some of the most trusted professions in society (Ipsos 2022), such a healthcare system and its staff, with a focus on sustainability and low climate impact, will be able to inspire other sectors and wider society to take sustainability seriously.
Co-Benefits from Healthcare Decarbonisation
Decarbonisation must be a goal of all industries for a sustainable future. At the same time, it offers an opportunity for co-benefits while reimagining how sectoral activities are organised and re-centred around planetary health.
Healthcare spaces and processes can thus be purposely (re)designed to be more people- and community-friendly. Together with infrastructure resilience, indoor air quality can be improved by designing for better insulation, better natural ventilation, and more efficient heating and cooling in healthcare facilities, with the air exchange rate deliberately incorporated in the building design. The use of green spaces can counteract the heat island effect, encourage socialisation, and have beneficial effects on mental health and mild effects of physical activity (WHO 2016).
Additionally, with health experts emphasising that a diet rich in plant-based foods and with fewer animal-source foods brings about improved health, healthcare facilities should be leading the way in making sure the foods they offer are tailored to nutritional needs and do not further threaten climate stability (Department of Health and Social Care U.K. 2020). Food waste deserves a special mention too, as it has been estimated that it can range from 6% to 65% in healthcare facilities (Health Care Without Harm 2016). This comes with planetary and monetary consequences – according to the NHS Hospital Food Review, food waste costs are around £230 million annually only in the UK (Department of Health and Social Care U.K. 2020), at a time when climate change threatens food systems (European Public Health Alliance 2023).
Ensuring waste efficiency could greatly modify the effect of the health system on public health. With a significant percentage of the waste generated within healthcare facilities classified as hazardous, it is essential that it is handled and disposed of responsibly and that these processes are considered in healthcare systems with a view to increasing their sustainability (Health Care Without Harm Europe 2020). One of the notable co-benefits of efficiently managing waste would be lowering the risk of spreading environmental antimicrobial resistance (AMR), which on its own threatens to exert a massive burden on healthcare in the future (Marschang and de Stefani 2016). As with climate change, AMR risks creating a feedback loop of deterioration, impacting healthcare and provision. Rethinking the food systems in healthcare facilities would, therefore, have triple benefits for the people, planet and economy and improve population health, decreasing the burden from the health system.
The Progress of Healthcare Decarbonisation
Health sectors are beginning to rise to the task of decarbonisation, with a number of countries publishing plans to reduce their carbon impact. Whole-sector transformation has become the ambition of some health systems, such as the British National Health Service establishing in 2022 its Net Zero Plan to decrease their climate impact (NHS England 2022). Building upgrades, technological upgrades, such as energy efficiency management systems and artificial intelligence (AI), on-site renewable energy generation, staff transport modal shift and transport electrification, reducing the environmental impact of medicines and pharmaceutical, and reforming the way food and catering are managed, aim to greatly reduce emissions in all scopes. The Plan signals to the supply chain and procurement that they are expected to decarbonise as well. Patient care will lean more towards the prevention of chronic disease, focus on digitalisation, and on capacity building. Importantly, the Plan acknowledges the health inequalities of different populations, such as greater environmental hazard exposure faced by marginalised populations (for example, from air pollution), as well as less access to positive environments (such as green space) and the way that a changing climate will change energy needs.
Attention to the physical infrastructure and working with nature (often termed nature-based solutions) have seen physical health sector infrastructure reduce its environmental impact but also increase its adaptation capacity and resilience. Last year, a Bangladeshi hospital won the global award for best building (The Guardian 2022). The building uses natural ventilation, plans space, light and shade to reduce energy use and increase efficiency, uses rainwater collection and harvesting, plans access around anticipated staff and patient flow, and provides courtyards and focal points for people to meet (ArchDaily 2022). By paying attention to the surrounding climate and geographical needs, in this case, in terms of rain, flooding and severe storms, as well as energy and lighting needs, infrastructure can be planned to reduce climate impact and improve resilience to a changing climate while catering to population needs.
Strict emissions reporting requirements are essential for effectively reducing carbon emissions in the health sector, ensuring transparency and accountability. The Dutch government is making significant strides in measuring healthcare emissions, which accounts for 4-8% (depending on the type of energy use and measure methodology) of the national carbon footprint, such as through the piloting of the Operation Zero methodology led by Health Care Without Harm (Health Care Without Harm n.d.). This initiative is a collaborative effort with the National Institute for Public Health and the Environment and the Ministry of Health, Welfare, and Sport. Phase one involved establishing a rigorous methodology to accurately measure carbon footprints, identify emission hotspots, and track progress. This included analysing emissions in material extraction, blue water consumption, land use, and waste generation. Drawing from the lessons learned, the pilot emphasised the importance of harmonising data with hard-to-measure sources, such as anaesthetic gas releases and employee commuting, to develop a comprehensive climate footprint analysis and decarbonisation roadmap.
Future Directions of Healthcare Decarbonisation
While a number of developing fields will assist in the mitigation of the healthcare sector’s impact on the environment and climate, technology alone will not resolve an issue deeply entrenched in a system of fossil fuel extraction and consumption. Systems change focused on shifting to cleaner systems based on energy efficiency, sustainability, and equity is the cornerstone of action in facing the climate crisis.
Tackling healthcare waste by developing cleaner, less plastic-based solutions can reduce environmental impact. Reducing systemic waste and promoting a circular economy based on decreased waste acceptance whilst allowing for recycling and safe disposal offers low-hanging fruit for the decarbonisation of the sector.
Technology is assisting this transition and presents various opportunities for the healthcare sector to decrease its impact, increase efficiency and resilience, and show global leadership to help protect the climate and global health. Telemedicine, popular during the COVID-19 pandemic, has been shown to be an effective intervention to reduce health sector-related emissions (Purohit et al. 2021). Promoting digital access and literacy can help aid in reducing climate impact. AI and Data Analytics also have the potential to streamline energy use in healthcare facilities, as outlined in the NHS Net Zero Plan. Machine learning algorithms, for example, can be employed to analyse patterns of energy use, anticipate future energy requirements, and implement strategies for energy conservation (Benti et al. 2023).
Successful health sector decarbonisation demands robust policy frameworks at the national and international levels. These policy frameworks should incorporate specific emission reduction targets, incentives for adopting green practices, and rigorous enforcement of environmental regulations. Policy can help enable and nudge the healthcare sector to secure the necessary transformations through financing, taxation and ring-fencing, and research and development. The healthcare sector can also significantly contribute to promoting change through the enforcement of diligent procurement standards, food system standards, land use management, and advocacy. The healthcare sector has notable political power as an anchor institution in communities to advocate for change, which ultimately stands to greatly benefit the sector by protecting public health (Reed et al. 2019). Similarly, the sector can lead by example, including through the example of healthcare staff, who should be leaders and educators when it comes to sustainability.
All of society can contribute to the healthcare sector’s decarbonisation, particularly through the application of a One Health and Planetary Health lens, which sees the health of people and the environment as inextricably linked. Policy approaches, such as Health-in-all-Policies (HIAP), take into account climate and can assist in decreasing morbidity and mortality, including from environmental exposures (such as air pollution) and chronic disease (such as cardiovascular disease related to transport noise). All policies have the potential to enable healthcare sector decarbonisation, working together to protect the environment and health.
The importance of prioritising population health cannot be overstated. The most sustainable impacts on healthcare can be achieved through reducing the need for healthcare and promoting a healthy lifespan, including into older age. Healthier populations with less need for healthcare (especially including older age populations) will mean a healthcare system using less resources and energy and producing less emissions. Robust measures to protect and promote population health will see a decrease in the impact of healthcare emissions.
Health equity and justice remain vital issues when looking at healthcare sector decarbonisation. Health inequities exist across society, including internationally and in terms of healthcare access. Action on the prevention of morbidity and mortality locally, regionally and internationally has a massive role to play in healthcare-related emissions. Ensuring that all populations, regions and nations have the resources to mitigate and adapt to climate change is essential in protecting health and ensuring health equity.
Conclusion
Decarbonising the health sector represents a unique opportunity to both mitigate climate change and improve public health outcomes. While the progress to date is encouraging, the path ahead is still long and requires sustained commitment. Ambitious actions and policies that 1) realise the tight interlinkage between healthcare sector emissions and public health and 2) see expenditure as the health investment that it is, are a vital component in protecting public health. All policies should take health and climate into consideration and work to reduce health inequity, both locally and further afield. International justice will be a key pillar for necessary change. Systems change needs to occur, with a rapid, deep, sustained shift to sustainable, low or no-carbon methods. Technology and innovation will offer opportunities to increase efficiency and decrease impact. It is necessary for climate change to be recognised as a profound threat to public health, recognising the role of each sector within health systems in facing climate change and ensuring a just transition that protects the marginalised and vulnerable through effective policies. Finally, we must acknowledge that countries are not on the same footing to tackle this dramatic transformation. The way to mitigate carbon footprint in very sophisticated healthcare organisations will be different, especially when needing to build a resilient healthcare system in countries where the basic needs are not yet covered. Systems approaches to complicated problems and stakeholder engagement with a focus on equity and inclusion are essential to truly protect public health.
Conflict of Interest
None. 
References:
Alderwick H, Hutchings A, Briggs A, Mays N (2021) The impacts of collaboration between local health care and non-health care organizations and factors shaping how they work: a systematic review of reviews. BMC Public Health. 21(1).
ArchDaily (2022) Friendship Hospital Satkhira/Kashef Chowdhury/URBANA.
Asaduzzaman M, Ara R, Afrin S et al. (2022) Planetary Health Education and Capacity Building for Healthcare Professionals in a Global Context: Current Opportunities, Gaps and Future Directions. In International Journal of Environmental Research and Public Health. 19(18).
Beatson A, Lings I, Gudergan SP (2008) Service staff attitudes, organisational practices and performance drivers. Journal of Management and Organization. 14(2):168–179.
Benti NE, Chaka MD, Semie AG (2023) Forecasting Renewable Energy Generation with Machine Learning and Deep Learning: Current Advances and Future Prospects. In Sustainability (Switzerland). 15(9).
Connor A, Lillywhite R, Cooke MW (2010) The carbon footprint of a renal service in the United Kingdom. QJM. 103(12):965–975.
Deivanayagam TA, English S, Hickel J et al. (2023) Envisioning environmental equity: climate change, health, and racial justice. The Lancet. 402(10395):64–78.
Department of Health and Social Care (UK) (2020) Report of the Independent Review of NHS Hospital Food. Available at http://www.nationalarchives.gov.uk/doc/open-government-licence/
Din SKJ, Russo A, Liversedge J (2023) Designing Healing Environments: A Literature Review on the Benefits of Healing Gardens for Children in Healthcare Facilities and the Urgent Need for Policy Implementation. In Land. 12(5).
Duque-Uribe V, Sarache W, Gutiérrez EV (2019) Sustainable supply chain management practices and sustainable performance in hospitals: A systematic review and integrative framework. In Sustainability (Switzerland). 11(21). MDPI.
Eckelman MJ & Sherman J (2016) Environmental impacts of the U.S. health care system and effects on public health. PLoS ONE. 11(6).
Edwards N, Dunn S, Barach P, Vaughan L (2023) The Wolfson Prize: designing the hospital of the future. Future Healthcare Journal. 10(1): 27–30.
European Public Health Alliance (2023) The Heavy Duty Vehicle CO2 Emissions Standards.
Gabbatiss J (2019) Healthcare in world’s largest economies ‘accounts for 4%’ of global emissions. CarbonBrief. Available at https://www.carbonbrief.org/healthcare-in-worlds-largest-economies-accounts-for-4-of-global-emissions/
Gerber PJ, Food and Agriculture Organization of the United Nations (2013) Tackling climate change through livestock : a global assessment of emissions and mitigation opportunities.
Gettler E, Smith B, Lewis S (2023) Challenges in the Hospital Water System and Innovations to Prevent Healthcare-Associated Infections. Current Treatment Options in Infectious Diseases. 15:1–13.
Guenther R & Vittori G (2013) Sustainable Healthcare Architecture, 2nd Edition.
Guetter CR, Williams BJ, Slama E et al. (2018) Greening the operating room. The American Journal of Surgery. 216(4):683–688.
Guivarch C, Taconet N, Mejean A (2021) Linking Climate and Inequality. International Monetary Fund.
Guzzo D, Carvalho MM, Balkenende R, Mascarenhas J (2020) Circular business models in the medical device industry: paths towards sustainable healthcare. Resources, Conservation and Recycling. 160(104904).
Health Care Without Harm (n.d.) Operation Zero. Available at https://noharm-europe.org/issues/europe/operation-zero
Health Care Without Harm (2015) Buildings Guidance for Members. Available at https://greenhospitals.org/sites/default/files/2021-09/Buildings-GGHH-Guidance-Document-Sample.pdf
Health Care Without Harm (2016) Food waste in European healthcare settings: Case studies from around Europe and recommendations for preventing and reducing food waste in healthcare.
Health Care Without Harm. (2023). Healthy Food in Health Care. Available at https://noharm-uscanada.org/issues/us-canada/healthy-food-health-care
Health Care Without Harm & ARUP (2021) Global Road Map for Health Care Decarbonization: A navigational tool for achieving zero emissions with climate resilience and health equity. Health Care Without Harm Climate-Smart Health Care Series Annex C. Green Paper, Number Two.
Health Care Without Harm & ARUP (2022) Designing a Net Zero Roadmap for Healthcare: Technical Methodology and Guidance.
Health Care Without Harm Europe (2020) Sustainable healthcare waste management in the EU Circular Economy model .
Hernández D (2020) Water systems in healthcare facilities. Clinical Engineering Handbook, Second Edition. 694–698.
Hickel J (2020) Quantifying national responsibility for climate breakdown: an equality-based attribution approach for carbon dioxide emissions in excess of the planetary boundary. The Lancet Planetary Health. 4(9):e399–e404.
Holmner Å, Ebi KL, Lazuardi L, Nilsson M (2014) Carbon footprint of telemedicine solutions - Unexplored opportunity for reducing carbon emissions in the health sector. PLoS ONE. 9(9).
Intergovernmental Panel on Climate Change (2023) Synthesis Report of the IPCC Sixth Assessment Report (AR6) Summary for Policymakers 4.
Ipsos (2022) Ipsos Veracity Index 2022. Ipsos. Available at https://www.ipsos.com/en-uk/ipsos-veracity-index-2022
Lokmic-Tomkins Z, Davies S, Block LJ et al. (2022) Assessing the carbon footprint of digital health interventions: a scoping review. Journal of the American Medical Informatics Association. Oxford University Press. 29(12):2128–2139.
Macneill AJ, Hopf H, Khanuja A et al. (2020) Transforming the medical device industry: Road map to a circular economy. Health Affairs. 39(12):2088–2097.
Markandya A, Sampedro J, Smith SJ et al. (2018) Health co-benefits from air pollution and mitigation costs of the Paris Agreement: a modelling study. The Lancet Planetary Health. 2(3):e126–e133.
Marschang S & de Stefani E (2016) Waste disposal in healthcare and effects on AMR. Hospital Healthcare Europe. Available at https://hospitalhealthcare.com/latest-issue-2016/waste-disposal-in-healthcare-and-effects-on-amr/
Masih I, Maskey S, Mussá FEF, Trambauer P (2014) A review of droughts on the African continent: a geospatial and long-term perspective. Hydrology and Earth System Sciences. 18(9):3635–3649.
Modisakeng C, Matlala M, Godman B, Meyer JC (2020) Medicine shortages and challenges with the procurement process among public sector hospitals in South Africa; Findings and implications. BMC Health Services Research. 20(1).
Mohamed A (2020) Energy Efficiency of Medical Devices and Healthcare Applications. London by Academic Press.
NHS England (2022) Delivering a “Net Zero” National Health Service.
Ode Sang Å, Thorpert P, Fransson AM (2022) Planning, Designing, and Managing Green Roofs and Green Walls for Public Health – An Ecosystem Services Approach. Frontiers in Ecology and Evolution. 10. Frontiers Media S.A.
O’Hara AC, Miller AC, Spinks H et al. (2022) The Sustainable Prescription: Benefits of Green Roof Implementation for Urban Hospitals. Frontiers in Sustainable Cities. 4. Frontiers Media S.A.
Paterson DL, Wright H, Harris PNA (2018) Health risks of flood disasters. Clinical Infectious Diseases. 67(9):1450–1454. Oxford University Press.
Pichler PP, Jaccard IS, Weisz U, Weisz H (2019) International comparison of health care carbon footprints. Environmental Research Letters. 14(6).
Priyalal WGSS, de Silva M L, Rajini PAD (2015) A Study on Water Management Strategies Practiced in Healthcare Facilities: A Literature Review. 6th International Conference on Structural Engineering and Construction Management 2015. Kandy, Sri Lanka, 11th -13th December 2015.
Purohit A, Smith J, Hibble A (2021) Does telemedicine reduce the carbon footprint of healthcare? A systematic review. Future Healthcare Journal. 8(1):e85–e91.
Reed S, Gopfert A, Wood S et al. (2019) Building healthier communities: the role of the NHS as an anchor institution. The Health Foundation. Available at https://www.health.org.uk/publications/reports/building-healthier-communities-role-of-nhs-as-anchor-institution
Rizan C, Bhutta MF, Reed M, Lillywhite R (2021) The carbon footprint of waste streams in a UK hospital. Journal of Cleaner Production. 286, 125446.
Romanello M, McGushin A, Di Napoli C et al. (2021) The 2021 report of the Lancet Countdown on health and climate change: code red for a healthy future. The Lancet. 398(10311):1619–1662.
Shaw C, Hales S, Howden-Chapman P, Edwards R (2014) Health co-benefits of climate change mitigation policies in the transport sector. Nature Climate Change 4:427–433.
Smith P & Bustamante M (2014) Agriculture, Forestry and Other Land Use (AFOLU).
Stockholm County Council (2014) Environmentally Classified Pharmaceuticals. Available at https://noharm-europe.org/sites/default/files/documents-files/2633/Environmental%20classified%20pharmaceuticals%202014-2015%20booklet.pdf
Wainwright O (2022) World’s best building award won by rainwater-harvesting hospital in rural Bangladesh. The Guardian. Available at https://www.theguardian.com/artanddesign/2022/jan/25/riba-best-building-award-friendship-hospital-bangladesh-kashef-chowdhury-david-chipperfield-wilkinson-eyre
United Nations (2021) Sustainable transport, sustainable development. Interagency report for second Global Sustainable Transport Conference.
U.S. Department of Health and Human Services (2014) Primary Protection: Enhancing Health Care Resilience for a Changing Climate.
Wen Y & Liu L (2023) Comparative Study on Low-Carbon Strategy and Government Subsidy Model of Pharmaceutical Supply Chain. Sustainability (Switzerland). 15(10).
World Health Organization (2015) Operational framework for building climate resilient health systems.
World Health Organization. Regional Office for Europe (2016) Urban green spaces and health.
World Health Organization (2017) Climate change and its impact on health on small island developing states. World Health Organization.
World Health Organization (2019) Health, environment and climate change.
World Health Organization (2020a) Guidance on mainstreaming biodiversity for nutrition and health.
World Health Organization (2020b) WHO guidance for climate resilient and environmentally sustainable health care facilities.










