HealthManagement, Volume 23 - Issue 4, 2023
XpanDH Project Support and Risks of a Delayed Regulation on the EHDS
This paper presents the journey towards the European Electronic Health Record Exchange Format (EEHRxF) as a process of standardisation as social actors in Europe accept how necessary it is for digital health interoperability to be a reality to reap the benefits of digital transformation. The way the XpanDH project is set up and how it is providing its contribution to this effort is presented with a reflection on the risks associated with a delayed or amputated European Health Data Space Regulation.
Key Points
- Digital health standardisation is as much a process as it is a necessary activity to ensure health as a human right is achieved.
- XpanDH project, alongside other initiatives, is there to support the European digital health ecosystem to co-create and adopt the European Electronic Health Record Exchange Format (EEHRxF). It is central to ongoing efforts while preparing to hand over and expand through other projects and initiatives.
- The EHRxF is more than a set of format dispositions in communications, recommendations and the proposal for a regulation on the European Health Data Space (EHDS); it is a necessary instrument to achieve EU-wide health data interoperability and better care for all.
- There is a risk to the formal dimension of the EEHRxF if the regulation on the EHDS is not co-legislated in early 2024, or it is but at the expense of significant amputation.
Introduction
The digital transformation in the health sector was initiated in the 80s and intensified in the early 2000s (Marques et al. 2020). With the urgent need to digitalise health data and create the first healthcare systems, there was a decentralised development and implementation of these systems in the European Member States (MS) in an independent way that resulted in a lack of interoperability among the systems.
The national development of eHealth solutions identified the need to exchange health data among the EU MS to facilitate and improve the patient treatment that was outside their home country or looking for specialised treatment outside their home country.
Standardisation is the process of developing and agreeing on common technical specifications for products, services, and processes. It is a key enabler of innovation and economic growth and holds a relevant role in ensuring the interoperability and compatibility of technologies (Feng 2003).
Two main perspectives on standardisation can help us: the functionalist perspective and the constructivist perspective. The functionalist perspective views standardisation as a rational and objective process driven by the need to improve efficiency and reduce costs. The constructivist perspective, on the other hand, views standardisation as a social process influenced by the interests and power of different stakeholders.
Standards have a long tradition, dating back to ancient China, yet they can be used and are often key to achieving process innovation (improving how things are done) and product innovation (creation of new products or services). Standards play a vital role in the global economy. They help ensure that products and services are compatible and interoperable, which is essential for trade and commerce (Tamura 2021).
Standards also help to improve safety and quality. Quality standards help to ensure that products meet certain performance requirements, for example, preventing accidents and injuries. These have been progressively associated with quality of care and patient safety initiatives.
By providing a common framework for innovation, standards can help to reduce the cost and risk of developing new products and services. Only with large integrated and purposeful sets of health data can we truly change health systems into learning ecosystems where patients not only access and own their data but can meaningfully use it and make informed decisions about their health and wellbeing (Moen et al. 2022).
Past Projects, Initiatives and Legislation
Considering the real need to exchange, integrate, and cross-country mobilise health data, many projects and initiatives have arisen to support interoperability development in the health sector in Europe. They were supported by funding, communications and recommendations from the European Commission.
The need for interoperability to access and exchange health data among the European MS has mobilised the European Commission and the MS to achieve interoperability in a cross-border context (Release of a Recommendation on 2 July 2008 (2008/594/EC).
The project epSOS (2008-2014) pioneered evaluating and piloting the first electronic exchange of health data in Europe. It has supported the creation of the MyHealth@EU.
The project CALLIOPE (2008-2010) has developed an interoperability roadmap for eHealth that was published a few years ago and is still valid, especially for semantic interoperability (Directive on applying patients’ rights in cross-border healthcare (2011/24/EU) of 2011). The legal foundation was created within it to set up the eHealth Network (art. 14), whose main objective is to ‘work towards delivering sustainable economic and social benefits of European eHealth systems and services and interoperable applications […]’.
To support the eHealth Network and health interoperability efforts, the joint action eHAction, following a series of other joint actions, aimed to reflect digital health importance as a complementary resource for public health and services. We are striving to explore technologies and tools to facilitate chronic disease management, increase the sustainability and effectiveness of health systems, enable personalised care, and empower people.
The European EHRxF was first discussed in Lisbon during an eHAction activity, contributing to the deliverable “Policy document about technology report”. At the time, it was considered that the format should aim to “make it possible for people to access their health records across EU borders as needed for cross-border healthcare purposes such as in case of accidents while travelling, or to seek treatment of chronic conditions, or rare diseases. In any situation where a person requires healthcare treatment in another Member State, having access to their personal health records will support and improve the quality of this care, for example, by enabling faster, more accurate diagnosis and improved prognosis”. It is intended to facilitate the flow of information of health data among the MS in an interoperable way.
In February 2019, the European Commission released the “Recommendation on a European Electronic Health Record Exchange format (C(2019)800) of 6 February 2019”, where a set of common principles, cluster of standards and the acknowledgement of the need to focus efforts on five priority health data domains was the core message. These five areas were: i) patient summaries, ii) electronic prescriptions and electronic dispensations, iii) medical images and image reports, iv) laboratory results and v) discharge reports.
From this recommendation, some EU projects initiated the development of services and improvements to speed up the achievement of health interoperability in the EU. Based on the EEHRxF recommendation, the X-eHealth project aimed to promote a faster and sustainable EU digital transformation by elaborating specifications and architecture propositions for implementing the five health domains indicated in the EEHRxF regulation.
XpanDH - Expanding Digital Health Through a Pan-European EHRxF-Based Ecosystem
XpanDH project supports an expanding ecosystem of individuals and organisations developing, experimenting and adopting the EEHRxF, providing a crucial contribution to the European Health Data Space (EHDS). It is a two-year Coordination and Support Action financed by the Horizon Europe Framework Programme.
Our focus is empowering individuals and organisations to create, adapt, and explore interoperable digital health solutions that truly make a difference. That is why we are mobilising and building capacity to ensure the widespread adoption of the EEHRxF.
The project has a stepwise approach for collecting specifications (functional, technical, semantical) feedback to support the creation of the required assets to implement solutions based on the EEHRxF. XpanDH is also working with all others who have already made progress in this area, and it is also talking to patients to make sure their needs are heard in a co-creation process.
Proposal for Regulation on the European Health Data Space
The EHDS is an initiative from the European Commission that intends to support the citizens to have control of their health data, better healthcare delivery and enable the MS to exchange health data in a secure and interoperable way.
The EHDS will be a health-specific ecosystem delimited by rules, common standards and practices, infrastructures, and governance framework. It will provide a trustworthy setting for secure access to and processing a wide range of health data.
The European Commission has presented a proposal for a Regulation on the EHDS, where different aspects regarding the scope and requirements, as well as the implementation mechanism for the EEHRxF, are established by legal means, as well as the associated EHR certification needs which intimately relate to the format and the capacity for the format to truly exert its harmonisation effect. As the EHDS relates to the processing and exchanging of health data that is highly sensitive, the approval of its regulation will officialise the rules that must be adopted by the MS, ensuring the security and further developments that shall be in place for its full implementation. The discussion of the proposed regulation started in May 2022 and is taking place in the EU. Both the European Parliament and the Council have been incredibly active in view of getting to a vote by no later than April 2024, after which, due to European Election and its aftermath, we could expect a delay of two to three years, projecting the practical effects of the Regulation, particularly regarding EHRs, certification and the use of an European EHR Format for as near as 2030 (if approval moves from 2024 to 2027, with two to three years of entry into full effect plus the time for the publication of implementing decisions).
How XpanDH is Developing the EEHRxF
XpanDH is an ongoing project aimed at maturing and accelerating a sustainable and scalable interoperability environment in Europe for digital health innovations based on the EEHRxF, involving both the supply and demand sides of healthcare provision.
An ecosystem approach to Digital Health Innovation and creating conditions for new cross and intra-border interoperable environments around a proposed set of standards – in this case, an EEHRxF-based infrastructure – differs from the EU cross-border initiatives that have been mostly governmental lead. Understanding digital health as an ecosystem means accepting some systemic properties:
1. Open innovation.
2. Multiple leadership
3. Concepts over action plans
4. Industry involvement and co-creation spaces
5. Government as coordinators
XpanDH understands an “infrastructure based on the EEHRxF” as a “publicly driven bundle of interoperability assets that allow the secure and ethical exchange of health data according to the EEHRxF related specification, guidelines and ethos” that was herewith named as the X-Bundle, which is conceived as a technical, personnel and processes infrastructure. The X-Bundle does not imply using a particular or unique IT infrastructure or level of interchange. This means its applicability extends from intra-organisational infrastructures and health data exchanges (i.e., inside an HCP using its interoperability infrastructure) to inter-organisational exchanges at local, regional, national or cross-border levels.
An adoption domain specifies the application of a use case to one or more particular care pathways and patient groups (or clinical/organisational/inter-organisational workflows) for which the digital solutions implementing the use case are expected to deliver value. It, therefore, provides a focus on the use case. As such, the EEHRxF adoption domain could be considered as “an instantiation of a use case, with a specific case application, that has meaning from a health system or clinical perspective, with defined implementable requirements (simple if only one EEHRxF priority category is uses or composite if data from more than one is required), that satisfies all the conditions for users to be ready to implement data exchange in conformity to EEHRxF guidelines and specifications”.
Finally, following a bottom-up approach, we understand the required feasibility verification to mean the capacity to show how organisations were able to get ready to adopt and hence adapt to the EEHRxF through different degrees of testing and usage that can be perceived as intra-organisational experimentation. “Experimentation bubbles’’ are sets of organisations collaborating within the project to jointly adopt and demonstrate the use of digital solutions (including interoperability) for an adoption domain. The bubble somehow includes the technical solution providers as it strives to exemplify how one or more healthcare organisations would jointly or separately procure, install, and use interoperable solutions from one or more ICT providers, mimicking the market situation.
For the necessary scale and pan-European impact, XpanDH will deploy the activities mentioned above through the XpanDH X-Nets - networks of stakeholders (EU or MS organisations) that, linked by similar interests, form the existing pan-European (Digital) Health space and can potentially use or benefit from the widest adoption of the EEHRxF.
Preliminary XpanDH Achievements
XpanDH has already defined six adoption domains to proceed with experimentation in collaboration with the project network. These serve to identify gaps, details to be further defined and issues that could come up with the EEHRxF implementation. They are distributed into two different domains: discharge reports and laboratory reports. The experimentation on the adoption domains intends to demonstrate the feasibility of EEHRxF-related solutions and recommendations for adoption.
The project also expands and brings awareness to the stakeholder community through the X-nets (networks of digital health ecosystem actors that need to be engaged with the Format). It will start to mature a “community of doers” with hopes to kick-start a patient-industry-led lead movement of concrete, hands-on support for promoting and developing EEHRxF tools and assets. Through the X-nets, XpanDH is raising awareness and collecting key information for developing the specifications and the bundles of assets necessary for an organisation to produce or implement EEHRxF-compatible digital health solutions (so-called X-bundles).
Expected Impact of EEHRxF for Digital Health Ecosystem
XpanDH project, by supporting the EEHRxF, is contributing to achieving the following impacts established for the Implementing Decision C (2021)1940: “European standards, including for operations involving health data, ensure patient safety and quality of healthcare services as well as effectiveness and interoperability of health innovation and productivity of innovators.” as well as “Health industry is working more efficiently along the value chain from the identification of needs to the scale-up and take-up of solutions at the national, regional or local level, including through early engagement with patients, healthcare providers, health authorities and regulators ensuring suitability and acceptance of solutions”.
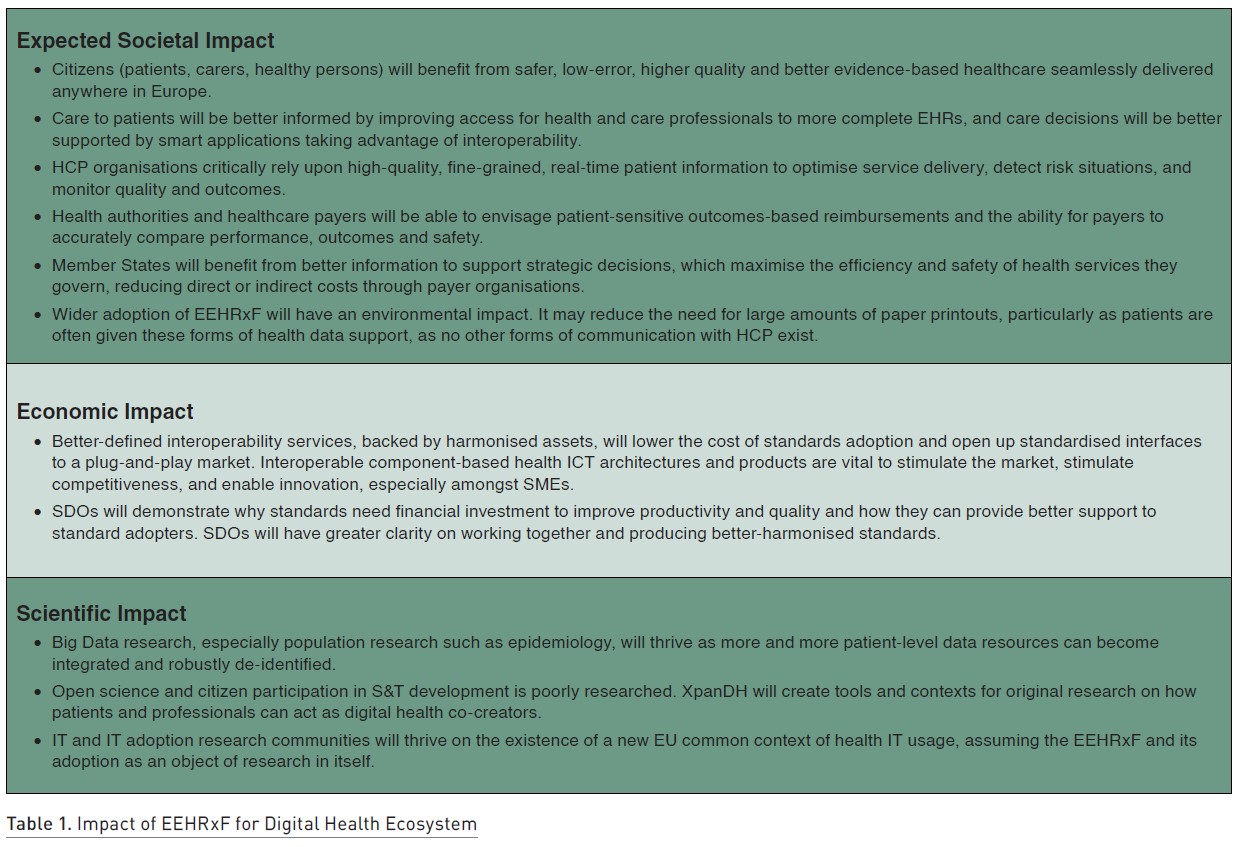
The digital health ecosystem is composed of many different actors. Their benefits have been anticipated (Table 1) due to our collective capacity to implement in MS and at the EU far more advanced interoperable solutions strengthening the digital transformation of health systems.
Co-Creation is a Keyword for EEHRxF
The best way to develop the EEHRxF is in collaboration with the eHealth community to identify the real needs of the patients and healthcare professionals (HCP) and create practical and useful solutions for health. In that sense, XpanDH has created the concept of a “community of doers, “ which joins patients, professionals, and programmers surrounding the EEHRxF to be ready to help others use and engage with digital health interoperability. These communities will co-create assets that support the adoption of the X-Bundle in real-life use cases. The ecosystem will showcase the drivers and benefits of interoperability and demonstrate how to capture value from it, while a community of doers will co-create assets for the X-Bundle and foster support to further adopters.
This concept is also present at the policy level, where regulation of the EEHRxF is key and requires active and capacitated national digital health authorities in permanent communication with the EC and spaces such as the eHealth Network and its sub-groups. The European Commission assumes a leading position in this activity by guiding the developments, where the diverse stakeholders’ contributions would have a voice. In this way, the real needs of the patients, health professionals, researchers and others can be routed into the EEHRxF specifications and implementing decisions. However, it is via the active participation of the national government and authorities (digital health, certification, inspectorate and others) and how they relate to the digital health industry. The healthcare providers delivering interoperable tools for the health sector can become a reality in each of the 27 MS, and some are following and preparing to adopt the EEHRxF.
Risk if Regulation on EHDS is Not Co-Legislated in 2024
Multiple scenarios are possible, and a detailed analysis of what could happen if a specific article or provision is or is not included in the final text is beyond this paper. To look at the impact on the EEHRxF adoption and a European single digital health market, we can consider three main scenarios:
- The EHDS regulation will be co-legislated in 2024 with no significant changes to articles related to the EEHRxF or the EHR certification schemas.
- The EHDS regulation will be co-legislated in 2024, and there is a reduction in the scope and ambition for the EHRxF, particularly in timing and in implementing instruments, and with shy provisions on EHR certification schemas.
- The EHDS regulation is not co-legislated in 2024. It is postponed to the next political cycle, most likely recovered as a topic in 2025, looking at final voting in 2027 or later.
Scenario One: Regulation on the EHDS approved in 2024
In scenario one, XpanDH, and more recently xShare project, the new XT-EHR Joint Action and a set of other forthcoming initiatives will need to further align its work to deliver concrete support and boost government, industry, and providers capacity to implement and adopt the EEHRxF as early as 2025. In this scenario, an acceleration and interest in digital health interoperability and significant stress on National Authorities, as well as industry and health providers, is likely to arise, as preparation and gradual uptake of standards have been traditionally slow and lagging in the EU even compared with the United States and some other non-EU countries.
With the development and rise of new technologies in the context of the EEHRxF and by improving the health systems, it will receive a diverse range of data to support the accurate diagnostics of the patients and improve the treatment.
For example, the genomic data could also be integrated into the EHR, allowing GPs to identify early possible development of diseases, such as cancer and degenerative diseases, by defining regular check-ups for patients with a medium-high probability of developing any genetic disease. In addition, many genetic variants are associated with the drug metabolism. In this regard, a more accurate prescription could be available to the patients, supported by the adoption of EEHRxF. Nevertheless, as the genomic data are highly sensitive, there is a need to align security protocols to ensure the privacy of these patient data.
The development and training of Artificial Intelligence (AI) tools could support the diagnostics and indication of treatment if implemented as tools in the eHealth systems. AI tools can also be applied in other categories, such as patient morbidity or mortality risk assessment, disease outbreak prediction and surveillance, and health policy and planning (Schwalbe and Wahl 2020). However, developing these tools requires good quality data and coherent data about each patient, which can only be truly achieved if digital solutions can integrate data seamlessly.
Scenario Two: Shy regulation on the EHDS approved in 2024
The EHDS regulation was co-legislated in 2024 at the expense of significant compromise between different legislative interests and amongst MS scepticism of its need and the capacity of different national interests and industry capabilities to embrace interoperability. Scenario two is that of a shy final document, striped from ambitious articles, with some of the early ideas pushed and parked and recitals which few will read and even fewer will consider when considering investments in digital health.
If the reduction in the scope and ambition for the EHRxF, particularly in timing and in implementing instruments, means an amputated EEHRxF is what can be enforced in the Union, we are likely to get a paralysis effect. This means MS which were investing in health interoperability efforts, such as commonly agreed minimum datasets or other semantic and technical agreements between their digital solution providers and broad ecosystem actors, may be stopped or feel restrained to do this, alongside hesitation on digital health investment at scale and the national level.
If the deadlines presented are too far away to ensure compromise solutions between mature and less mature MS on their capacity to uphold EEHRxF demands, we can face a lack of necessary time-related stress. The need is there, but too far into the future.
Finally, if shy provisions on EHR certification schemas mean a loose EU harmonisation function, too laissez-faire approach to national certification is the outcome of the negotiations, then a very fragile implementation strategy is possible to achieve a truly single digital health market. For example, the absence of mechanisms, even if only progressive, for mutual recognition of certification for digital health solutions regarding their adherence to EEHRxF requirements would mean that a company may need to file for certification in all or many of the 27 MS, which could mean more barriers to entry than at present when the ethos of the EHDS is that digital health solution providers could grow as their offer grows from a national footprint to an EU-wide one.
Scenario Three: Regulation on the EHDS delayed to 2027 or beyond
The EHDS regulation is not co-legislated in 2024 in scenario three. It is postponed to the next political cycle, the configuration of which is unknown and highly unpredictable, particularly in a post-COVID era, where health is losing political attention to war in Europe, energy crisis and other permacrisis elements. At best, the topic of a common space of rules, data and digital for health is recovered in 2025, which may mean revamping the proposal and/or looking at a final vote in 2027 or later.
MS will continue to work to use digital for better health, stimulated by compelling evidence, powerful speeches and stimulating Digital Health events such as the recent 2nd Symposium on Digital Health by WHO Europe, the HIMSS Europe enthusiasm or the Radical proposals from the Helsinki Festival. This is not bad, and apart from the occasional unhealthy competitiveness, cooperation and sharing instruments such as the eHealth Network and several EU-funded projects will continue to contribute to divergence forces. However, in the absence of regulation on the EHDS or similar, there will be NO convergence that could mean a common market of interoperable solutions. Establishing national discrepancies in certification schemas will inevitably further fence national and niche markets, rendering our companies as small as our ambition to have a large European Health Data Space.
Conclusions
The EEHRxF is not to be seen as a standard itself but makes use of and will surely live off standards. Its co-creation, implementation and adoption are nonetheless a standardisation process. Two main perspectives on standardisation can help us: the functionalist perspective and the constructivist perspective. While the constructivist perspective of standardisation would help us understand how the EHDS is influenced by the interests and power of different stakeholders and could fool us into accepting a possible delay or downsizing as inevitable. A functionalist perspective would suggest that such unwanted outcomes would impact the realisation of the vision for an adoptable EEHRxF resulting in lost opportunities for improvements in efficiency and reduction of costs, in quality of care and avoidance of risks to patients’ lives.
While the XpanDH project, in its humble contribution to supporting the efforts for a European Electronic Health Record Exchange format, is progressing well with its work, it now turns is concern to the sizable risk of seeing its core object – the EEHRxF – losing momentum or consistency as the negotiations for voting on a final text of the Regulation on the European Health Data Space unfold to a conclusive drawn in 2024, or towards postponement into the future. On the other hand, XpanDH and a family of projects directly or indirectly related to the EEHRxF are gathering forces. They can influence the ecosystem, which, democratically, can reach its European Parliamentarians and elected governments, advocating for the need for a worldwide innovative way of moving digital health together, harmonised and co-creating.
Conflict of Interest
Henrique Martins and Anderson Carmo are coordinators and project managers for the EU-funded project XpanDH, which is a Coordination and Support Action to promote the development and adoption of the European Electronic Health Record Exchange Format.
References:
Feng P (2003) Studying Standardization: A review of the Literature. ESSDERC. Proceedings of the 33rd European Solid-State Device Research.
Marques ICP, Ferreira JJM (2020) Digital transformation in the area of health: systematic review of 45 years of evolution. Health Technol. 10:575–586.
Moen A, Chronaki C, Martins H, Ferrari G (2022) People Centric Model to Harness User Value: Personal Data Spaces in Transformation of Health & Care. HealthManagement The Journal. 22(2):58-62.
Schwalbe N, Wahl B (2020) Artificial intelligence and the future of global health. Lancet. 395(10236):1579-1586.
Tamura S (2021) The Role and Historical Development of Standards. Available at https://www.rieti.go.jp/en/columns/a01_0641.html


















