HealthManagement, Volume 24 - Issue 1, 2024
Rise of smart devices, telecare, and IoT healthcare apps to facilitate diabetes diagnostics and management.
Key Points
- The number of people living with diabetes worldwide amounted to 529 million in 2023.
- Internet of Things (IoT) technology has opened many opportunities for simpler and earlier diagnostics, prevention, symptom management, and minimisation of the consequences of diabetes.
- Applications that help diabetic patients manage their diet and water intake, keep track of body weight, and control temperature and humidity in their homes are part of the favourable environment.
According to The Lancet, the number of people living with diabetes worldwide amounted to 529 million in 2023. And this number is projected to grow in the coming decade. The prognosis seems daunting, but healthcare professionals and specialists from multiple industries are actively working on controlling this condition.
The rise of smart devices, telecare, and IoT healthcare apps has aided in diabetes diagnostics and management immensely.Although glucometers are indispensable in the fight against diabetes, the Internet of Things technology has opened many more opportunities for simpler and earlier diagnostics, prevention, symptom management, and minimisation of the consequences. For example, a 2021 RELIEF study asserts that patients with type 1 diabetes who started using continuous glucose monitoring systems instead of usual glucometershad a 49% lower risk of diabetes-related hospitalisation (Roussel et al. 2021).
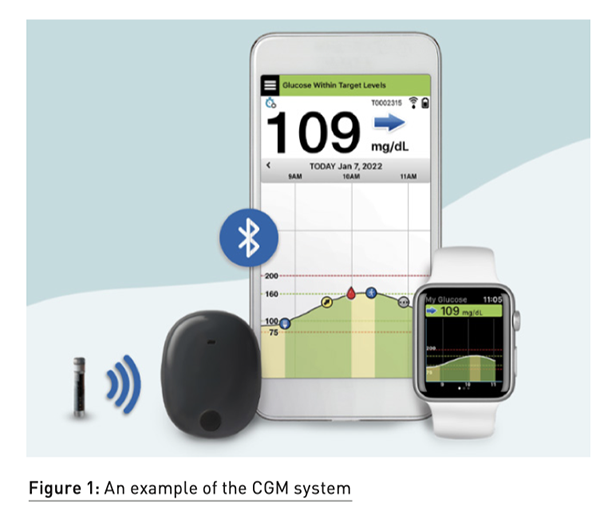
Smart Continuous Glucose Monitoring System
Patients with cognitive and memory problems, which are not uncommon among people living with diabetes, often forget to use their glucometers. The continuous glucose monitoring system tests its wearers’ blood without requiring any action from the patient. It has to be implanted and tuned by the doctor every few months, and then it does the job automatically. Moreover, the recent models of such a system alert patients and care providers in case of any abnormalities in measured metrics.
Smart Insulin Pens
Managing diabetes puts a strain on patients, mainly because of the amount of information they have to remember all the time. Many smart devices focus on storing relevant data so patients don't have to. An excellent example is smart insulin pens that connect to a smartphone or tablet application. These applications store the history of insulin injections transmitted from the pen, including the date and time of the injection and the amount of insulin delivered. This information is vital for patients and their doctors to prevent overdose and hyperglycaemia.
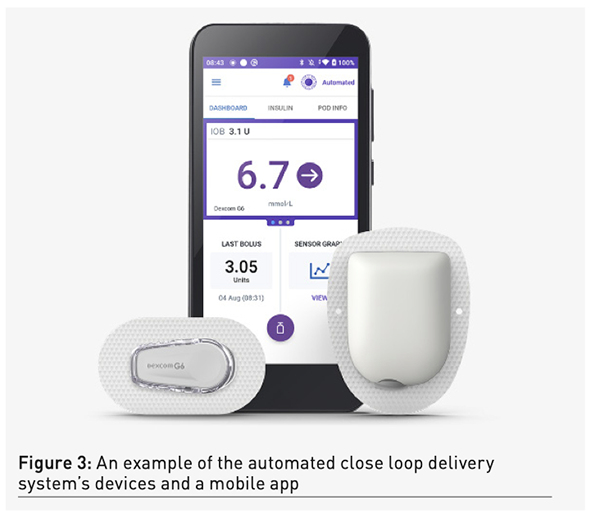
Automated Closed-loop Insulin Delivery System
An automated closed-loop insulin delivery system works as an artificial pancreas because it almost takes over the endocrine functions of this organ. These systems consist of three main components:
- A continuous glucose monitoring device
- A remotely controlled insulin pump
- A software solution that enables their coordination
The monitoring device regularly checks a patient's blood glucose levels and quickly delivers the results to the software installed on the user's smartphone or a special controller. The algorithm determines whether the patient's glucose levels correspond to the recommended parameters and, if not, triggers the insulin pump to dispatch the dose of insulin needed to normalise the glucose levels. This device makes life much easier for people living with type 1 diabetes, as they don't have to constantly perform glucose checks, count the amount of insulin they need, and manually inject it with an insulin pen they have to bring with them everywhere.
Wearable Sensors
One of the many dangers of diabetes is its frequent company of other disorders that include nerve and soft tissue damage, hypertension, and vascular problems. On top of managing their blood glucose levels to avoid unpleasant and dangerous symptoms of diabetes itself, patients have to control their blood pressure and nerve activity to identify any complications early.
Devices like blood pressure and heartbeat trackers, pulse oximeters, portable ECG monitors, and skin conductance sensors simplify this task. Such gadgets can be used separately but bring more value if integrated into one IoT ecosystem. This way, an additional healthcare analytic system can use data gathered from all the devices more effectively to discover patterns and trends in patients' conditions. Based on such findings, doctors can prevent potential issues faster with more positive outcomes.
Diabetic Ulcer Prevention And Rehabilitation Footwear
Diabetic ulcers are wounds or sores that can occur anywhere on the skin but usually affect diabetic patients’ feet. Up to 25% of people with diabetes suffer from this complication, which leads to limb amputation if untreated. Therefore, multiple devices were developed to prevent and treat this condition:
- Smart socks can be worn on their own or under regular socks. They monitor skin temperature, moisture levels, and pressure in foot blood vessels. Doctors use this data to identify areas at risk of developing sores or ulcers.
- Smart insoles are inserted into shoes just like regular ones. They perform the same functions as smart socks but focus more on foot pressure and movement, helping identify the beginning of diabetic neuropathy.
- Smart wound management footwear that is currently being developed and tested looks like a heavy boot and is used for diabetic ulcer treatment assistance rather than prevention. It has the same capabilities as smart socks and insoles but also can normalise the temperature and moisture inside the boot according to its readings. This footwear also has a built-in vibration system that provides feedback to the wearer when some adjustments in walking patterns are necessary.

Conclusion
Healthcare device manufacturers and software engineers develop, test, and put newer, more intelligent IoT devices into production every year. Besides, many general practice gadgets improve life for people with diabetes, even though they aren't connected to this condition directly. Applications that help users manage their diet and water intake, keep track of body weight, and control temperature and humidity in their homes are all a part of the favourable environment for people with diabetes. It is up to medical professionals and patients themselves to actively use such devices to improve health outcomes.
Conflict of Interest
None.
References:
Roussel R, Riveline JP, Vicaut E et al. (2021) Important Drop in Rate of Acute Diabetes Complications in People With Type 1 or Type 2 Diabetes After Initiation of Flash Glucose Monitoring in France: The RELIEF Study. Diabetes Care. 44(6):1368-1376.
The Lancet (2023) Diabetes: a defining disease of the 21st century. 401(10394):2087.
















