On Saturday, August 26, 2023, Philips researchers presented data at the European Society of Cardiology Congress in Amsterdam demonstrating how specific diagnostic referral codes [1] can potentially help to pre-determine how long a cardiology patient should receive mobile telemetry, or Holter monitoring, to monitor their symptoms remotely and possibly prevent further hospitalization.
Holter monitor electrocardiography (ECG) is used to detect potential cardiac arrhythmias, such as atrial fibrillation (AF) in patients experiencing symptoms like chest pain, shortness of breath, or palpitation. With conventional 24-hour ECG Holter monitoring, data analysis and reporting methods are often labor-intensive and inefficient, upfront costs may be high, turnaround times are often long, and patient compliance and satisfaction may be reduced due to inconvenient processes. Comparatively, extended-wear Holter (EWH) monitors, like Philips ePatch, are worn for several days of continuous monitoring and have become more common in clinical practice in the US, but are still far from the standard internationally, including in European countries.
At the 2023 American College of Cardiology World Congress of Cardiology in March, researchers from Philips compared 1, 7 and 14 days of retrospective data collected from Philips ePatch extended-wear Holter monitor. Results showed that extending ePatch monitoring resulted in twice the number of clinically actionable findings after 7 days and more than 2.5 times the findings after 14 days. With such strong initial findings, the team decided to continue their deep dive analysis to look closer at specific diagnoses to further understand the impact of using an extended monitoring solution.
When ordering Holter monitoring for a patient, clinicians must provide a referral diagnosis to indicate the reason for the study. Researchers once again compared retrospective ePatch data to determine the impact of referral diagnosis on overall diagnostic yield for clinically significant arrhythmias using ePatch for 1, 7 and 14 days. [fig. 1]
Figure 1
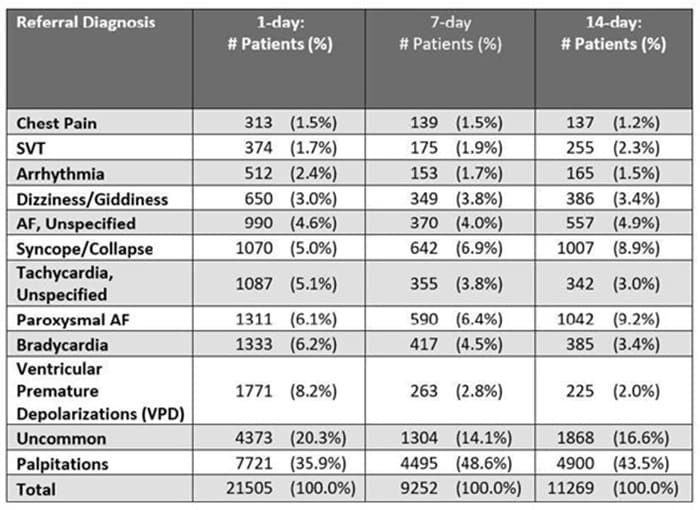
Philips analyzed data from over 40,000 ePatch patients and found three tiers of referral diagnoses based on the results seen with 1-day of monitoring.
- Tier 1: The five referral codes with the lowest diagnostic yield, or detection, at Day 1 [fig. 2] had the greatest increase with extended monitoring, suggesting these patients would benefit most from extended monitoring duration.
- Tier 2: Referral diagnoses with a 20-30% detection at Day 1 [fig. 2] matched our previous overall diagnostic detection findings with increases continuing to Day 14 of monitoring.
- Tier 3: The four referral diagnoses with the highest detection at Day 1 [fig. 2] had significant increases in diagnostic yield at Day 7 that continued to increase at Day 14 but not quite as dramatically as the Tier 1 referrals.
Figure 2
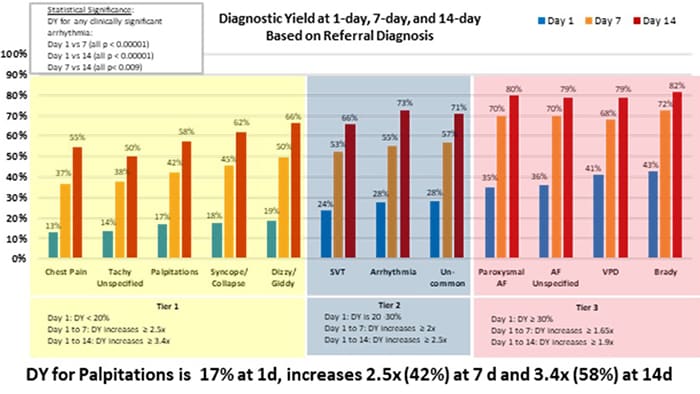
These results indicate that referral diagnosis can potentially guide prescribed monitoring duration. Philips poster presented at ESC 2023 can be found here.
On August 27, Philips customer Dr. Pere Blanch, Cardiologist at Hospital Sant Joan Despi Moises Broggi of Barcelona, also presented an abstract at ESC, entitled Initial clinical experience with new technology: ePatch extended Holter monitoring, which evaluates the quality and diagnostic efficacy – including diagnostic speed and accuracy and workflow simplicity – of Philips ePatch across various clinical settings.
“Philips ePatch technology has helped us to address many of the challenges associated with traditional Holter monitoring,” said Dr. Blanch. “We’re spending less time on logistics and set-up, and we’re seeing improved patient compliance thanks to the device’s ease of application and comfort. The data presented by Philips, along with the data that we found from our own evaluation of the diagnostic efficiency of EWH monitoring using ePatch, help to inform care decisions and offer peace of mind to both our patients and our staff.”
Philips helps to extend patient oversight beyond hospital walls and improve outcomes with a cardiac ambulatory monitoring portfolio that includes a range of monitors with flexible wear options to enhance patient compliance. Cloud-based AI and advanced algorithms quickly process high-quality ECG data into actionable reports that integrate with EMR to accelerate decision-making, support streamlined workflow, and enable patient-centered care.
To learn more about Philips broad portfolio of ECG solutions, visit https://www.gobio.com/heart-monitoring/
1. The tenth revision of the International Classification of Diseases, or ICD-10, is designed to promote international comparability in the collection, processing, classification, and presentation of mortality statistics.
Source: Philips
























