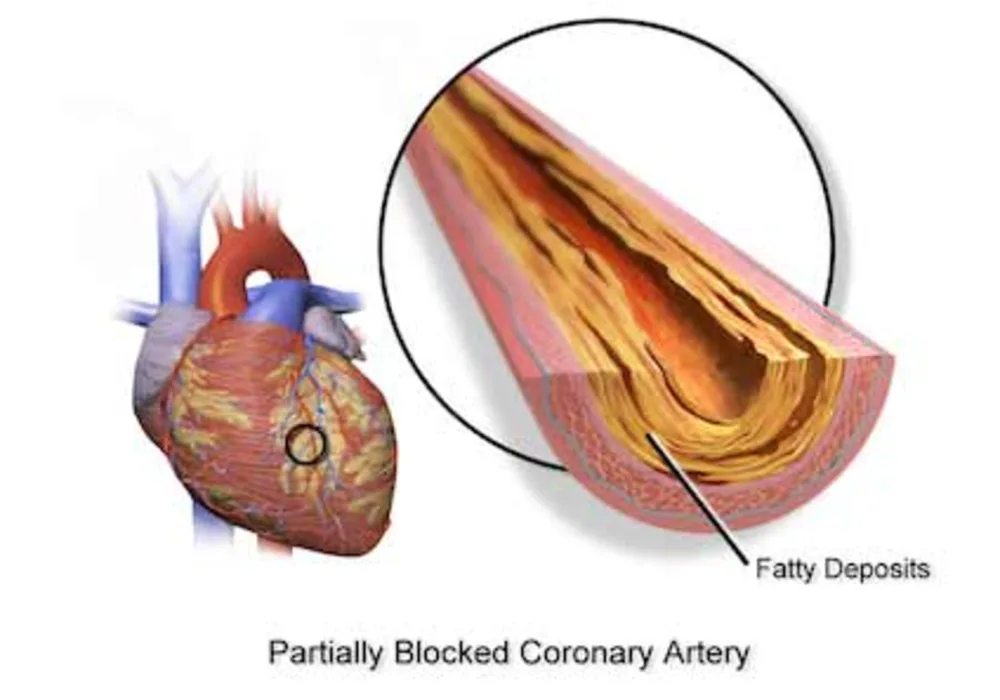
From the early days of percutaneous coronary intervention (PCI) it became apparent that the presence of severe coronary calcification was a predictor of worse clinical outcomes. In the era of plain old balloon angioplasty, severe coronary calcification was associated with an increased risk of coronary dissection and procedural failure, while in the bare-metal stent era, it was associated with a higher incidence of in-stent restenosis and target lesions revascularisations (TLR).
The advent of drug-eluting stents (DES) changed the landscape of coronary intervention through the reduced risk of restenosis and TLR, thereby allowing the interventional treatment of complex lesions and high-risk patients. Several studies have examined the efficacy of DES in heavily calcified lesions reporting mixed results.
The current study aims to investigate the long-term prognostic implications of coronary calcification in patients undergoing PCI for obstructive coronary artery disease (CAD).
Methods
Researchers analysed data from 6,296 patients enrolled in seven clinical DES trials to identify in angiographic images the presence of severe coronary calcification:
The baseline demographic data and the X-ray angiographic data of the patients were transferred to an independent academic research organisation (Cardialysis, Rotterdam, The Netherlands) for further analysis. Most of the studied patients were male with a history of hypertension and hypercholesterolaemia and were admitted because of an acute coronary event.
The studied patients were categorised into those with severely calcified coronary lesions and those without severe lesion calcification. Comparisons between the two groups were performed using the Mann–Whitney U test for the continuous variables, and the χ2 test for the categorical variables.
All the studied patients were followed-up for at 3 years. The primary end-point of this analysis was all-cause mortality at 3 years follow-up. Secondary end-points of this analysis were the combined end-points for death—all MIs (ST-elevation and non-ST-elevation MI)—and the composite end-point for—MI—any revascularisation.
Cox regression analysis was used to identify predictors of adverse events, that is, all-cause mortality,—MI, death—MI—any revascularisation, and ST. The hazard ratio (HR) and the 95% confidence interval (CI) for the continuous variables were estimated per unit increase. To exclude colinearity, the authors identified the variables that were highly correlated (r>0.5 and p<0.05), and included in the model only those variables that had a higher level of prognostic significance.
Results
Severe calcification was detected in 20% of the studied population. Patients with severe lesion calcification were less likely to have undergone complete revascularisation (48% vs 55.6%, p<0.001) and had an increased mortality compared with those without severely calcified arteries (10.8% vs 4.4%, p<0.001). The event rate was also high in patients with severely calcified lesions for the combined end-point death—MI (22.9% vs 10.9%; p<0.001) and death—MI—any revascularisation (31.8% vs 22.4%; p<0.001).
On multivariate Cox regression analysis, including the Syntax score, the presence of severe coronary calcification was an independent predictor of poor prognosis (HR: 1.33 95% CI 1.00 to 1.77, p=0.047 for death; 1.23, 95% CI 1.02 to 1.49, p=0.031 for death—MI, and 1.18, 95% CI 1.01 to 1.39, p=0.042 for death—MI—any revascularisation), but it was not associated with an increased risk of stent thrombosis.
Conclusion
Patients with severely calcified lesions are at a high risk of experiencing a cardiovascular event. Severe lesion calcification appears to provide additional prognostic information to the Syntax score, which reflects lesion complexity, because it is a marker of extensive atherosclerosis, and because patients with severely calcified lesions do not receive complete revascularisation. Further research is needed to explore whether a decalcification strategy and complete revascularisation of these high-risk patients would have a beneficial effect on their prognosis.
Reference
Christos V Bourantas, Yao-Jun Zhang, Scot Garg, Javaid Iqbal, Marco Valgimigli, Stephan Windecker, Friedrich W Mohr, Sigmund Silber, Ton de Vries, Yoshinobu Onuma, Hector M Garcia-Garcia, Marie-Angele More, Patrick W Serruys. Heart. 2014;100(15):1158-1164. © 2014 BMJ Publishing Group Ltd & British Cardiovascular Society
Image credit: Wikipedia
The advent of drug-eluting stents (DES) changed the landscape of coronary intervention through the reduced risk of restenosis and TLR, thereby allowing the interventional treatment of complex lesions and high-risk patients. Several studies have examined the efficacy of DES in heavily calcified lesions reporting mixed results.
The current study aims to investigate the long-term prognostic implications of coronary calcification in patients undergoing PCI for obstructive coronary artery disease (CAD).
Methods
Researchers analysed data from 6,296 patients enrolled in seven clinical DES trials to identify in angiographic images the presence of severe coronary calcification:
- ARTS II (Arterial Revascularisation Therapies Study II)
- LEADERS (Limus Eluted From a Durable vs Erodable Stent Coating)
- MULTISTRATEGY (Multicenter Evaluation of Single High-Dose Bolus Tirofiban vs Abciximab With Sirolimus-Eluting Stent or Bare-Metal Stent in Acute Myocardial Infarction (MI))
- STRATEGY (Single High-Dose Bolus Tirofiban and Sirolimus-Eluting Stent vs Abciximab and Bare-Metal Stent in Myocardial Infarction)
- SIRTAX (Sirolimus-Eluting Stent Compared With Paclitaxel-Eluting Stent for Coronary Revascularization)
- SYNTAX (Synergy Between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery)
- RESOLUTE (Resolute All Comers)
The baseline demographic data and the X-ray angiographic data of the patients were transferred to an independent academic research organisation (Cardialysis, Rotterdam, The Netherlands) for further analysis. Most of the studied patients were male with a history of hypertension and hypercholesterolaemia and were admitted because of an acute coronary event.
The studied patients were categorised into those with severely calcified coronary lesions and those without severe lesion calcification. Comparisons between the two groups were performed using the Mann–Whitney U test for the continuous variables, and the χ2 test for the categorical variables.
All the studied patients were followed-up for at 3 years. The primary end-point of this analysis was all-cause mortality at 3 years follow-up. Secondary end-points of this analysis were the combined end-points for death—all MIs (ST-elevation and non-ST-elevation MI)—and the composite end-point for—MI—any revascularisation.
Cox regression analysis was used to identify predictors of adverse events, that is, all-cause mortality,—MI, death—MI—any revascularisation, and ST. The hazard ratio (HR) and the 95% confidence interval (CI) for the continuous variables were estimated per unit increase. To exclude colinearity, the authors identified the variables that were highly correlated (r>0.5 and p<0.05), and included in the model only those variables that had a higher level of prognostic significance.
Results
Severe calcification was detected in 20% of the studied population. Patients with severe lesion calcification were less likely to have undergone complete revascularisation (48% vs 55.6%, p<0.001) and had an increased mortality compared with those without severely calcified arteries (10.8% vs 4.4%, p<0.001). The event rate was also high in patients with severely calcified lesions for the combined end-point death—MI (22.9% vs 10.9%; p<0.001) and death—MI—any revascularisation (31.8% vs 22.4%; p<0.001).
On multivariate Cox regression analysis, including the Syntax score, the presence of severe coronary calcification was an independent predictor of poor prognosis (HR: 1.33 95% CI 1.00 to 1.77, p=0.047 for death; 1.23, 95% CI 1.02 to 1.49, p=0.031 for death—MI, and 1.18, 95% CI 1.01 to 1.39, p=0.042 for death—MI—any revascularisation), but it was not associated with an increased risk of stent thrombosis.
Conclusion
Patients with severely calcified lesions are at a high risk of experiencing a cardiovascular event. Severe lesion calcification appears to provide additional prognostic information to the Syntax score, which reflects lesion complexity, because it is a marker of extensive atherosclerosis, and because patients with severely calcified lesions do not receive complete revascularisation. Further research is needed to explore whether a decalcification strategy and complete revascularisation of these high-risk patients would have a beneficial effect on their prognosis.
Reference
Christos V Bourantas, Yao-Jun Zhang, Scot Garg, Javaid Iqbal, Marco Valgimigli, Stephan Windecker, Friedrich W Mohr, Sigmund Silber, Ton de Vries, Yoshinobu Onuma, Hector M Garcia-Garcia, Marie-Angele More, Patrick W Serruys. Heart. 2014;100(15):1158-1164. © 2014 BMJ Publishing Group Ltd & British Cardiovascular Society
Image credit: Wikipedia
Latest Articles
PCI, CAD, coronary artery disease, calcification, percutaneous coronary intervention
From the early days of percutaneous coronary intervention (PCI) it became apparent that the presence of severe coronary calcification was a predictor of wo...