Late-breaking research presented in a Hot Line session at the ESC Congress 2023 reveals that Optical Coherence Tomography (OCT)-guided percutaneous coronary intervention (PCI), results in a larger minimum stent area. However, it does not reduce the two-year rate of target vessel failure when compared with angiography-guided PCI. The use of OCT-guided PCI significantly reduced stent thrombosis.
Previous clinical studies have demonstrated improved outcomes associated with intravascular imaging-guided PCI compared to angiography guidance alone. The ILUMIEN IV trial explored whether OCT-guided PCI is better than angiography-guided PCI for minimum stent area and target vessel failure in cases involving complex patients and lesions.
The trial included patients with medication-treated diabetes and/or complex lesions. Complex lesions were defined as non-ST-segment elevation myocardial infarction (NSTEMI), late-presenting ST-segment elevation myocardial infarction (STEMI; >24 hours), stent length of ≥28 mm, severe calcification, two-stent bifurcation, in-stent restenosis, or chronic total occlusion. The trial spanned 80 sites across 18 countries, specifically focused on complex patients and lesions for their anticipated potential to benefit from OCT guidance. The participants were randomly divided into two groups – one undergoing OCT-guided PCI and the other undergoing angiography-guided PCI. Blinded OCT assessment was performed after PCI in the angiography group.
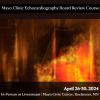
The primary study endpoints included post-PCI minimum stent area assessed by OCT, and the two-year rate of target vessel failure, defined as a composite of cardiac death, target vessel myocardial infarction, or ischaemia-driven target vessel revascularisation. The study included 2,487 patients, with 1,233 receiving OCT-guided PCI and 1,254 undergoing angiography-guided PCI.
As per the results of the study, the OCT-guided group exhibited a larger minimum stent area than the angiography-guided group. Over a two-year period, 88 OCT-guided patients experienced target vessel failure compared to 99 angiography-guided patients.
From a safety perspective, OCT guidance resulted in fewer angiographic complications. Apart from the larger minimum stent area, the OCT-guided approach resulted in fewer cases of major dissection, malapposition, tissue protrusion, and untreated reference segment disease. Stent thrombosis within two years occurred in 6 OCT-guided patients and 17 angiography-guided patients. Although the number of cardiac deaths and myocardial infarctions was lower in the OCT group, these distinctions were not statistically significant.
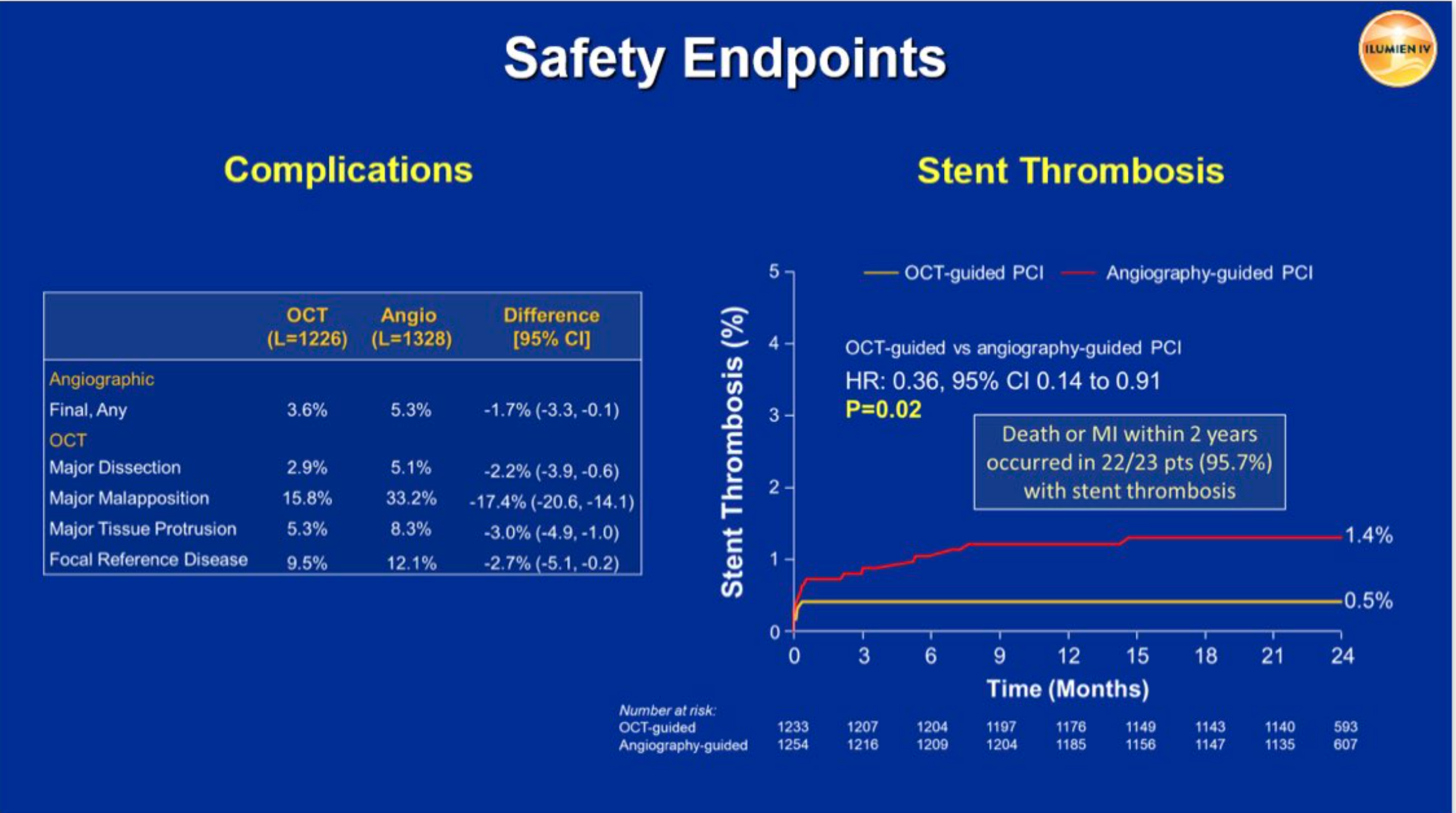
Study author Dr Ziad Ali of St. Francis Hospital in Roslyn, USA, concluded that OCT-guided PCI led to a larger minimum stent area, enhanced the safety of the PCI procedure, and resulted in an almost two-thirds reduction in stent thrombosis during the two-year follow-up. However, OCT guidance did not reduce the two-year rate of target vessel failure compared to angiography-guided PCI due to a low and almost identical rate of target vessel revascularisation in both arms of the study.
Source: ESC Congress 2023
Slide and Image Credit: ESC Congress 2023