Subsolid nodules, including pure ground-glass nodules (pGGNs) and part-solid nodules (PSNs), are increasingly detected through incidental findings or lung cancer screening. Despite their generally slow-growing nature, these nodules carry a high risk of malignancy. While some are transient inflammatory processes, persistent nodules are often associated with adenocarcinoma, ranging from precursors like atypical adenomatous hyperplasia to invasive adenocarcinoma. Current clinical staging guidelines and recommendations from organisations like the Fleischner Society and the American College of Radiology suggest noninvasive surveillance for pGGNs. However, recent research indicates that a notable portion of pGGNs turn out to be invasive adenocarcinomas upon resection, challenging these guidelines. Efforts have been made to predict invasiveness in pGGNs, with studies focusing on features like internal increased attenuation, which suggests a higher likelihood of malignancy. A distinction is made between pGGNs and "heterogeneous GGNs," the latter being characterised by internal solid components visible on lung windows but not on soft-tissue windows. This classification differs from standard clinical practice, raising questions about its applicability. While some studies have looked into the pathological diagnoses of heterogeneous GGNs, there is limited data on the clinical outcomes post-resection. To address these gaps, a recent study published in the American Journal of Roentgenology aims to compare the clinical outcomes of resected pGGNs, heterogeneous GGNs, and PSNs. Such analysis could help refine management guidelines for these subsolid nodules, considering their varying degrees of malignancy risk and potential for adverse outcomes.
Retrospective Analysis of Clinical Outcomes in Resected Subsolid Lung Nodules
In this retrospective study, 469 patients who underwent resection of lung adenocarcinoma appearing as subsolid nodules on CT scans were analysed. The patients, predominantly female (335) with a median age of 68 years, were observed between January 2012 and December 2020. Two radiologists independently classified each nodule as pure ground-glass nodules (pGGNs), heterogeneous ground-glass nodules (heterogeneous GGNs), or part-solid nodules (PSNs) using lung windows, with any disagreements resolved through discussion. Heterogeneous GGNs were defined as nodules with internal increased attenuation slightly less dense than pulmonary vessels, while PSNs were characterized by an internal solid component with attenuation similar to pulmonary vessels.
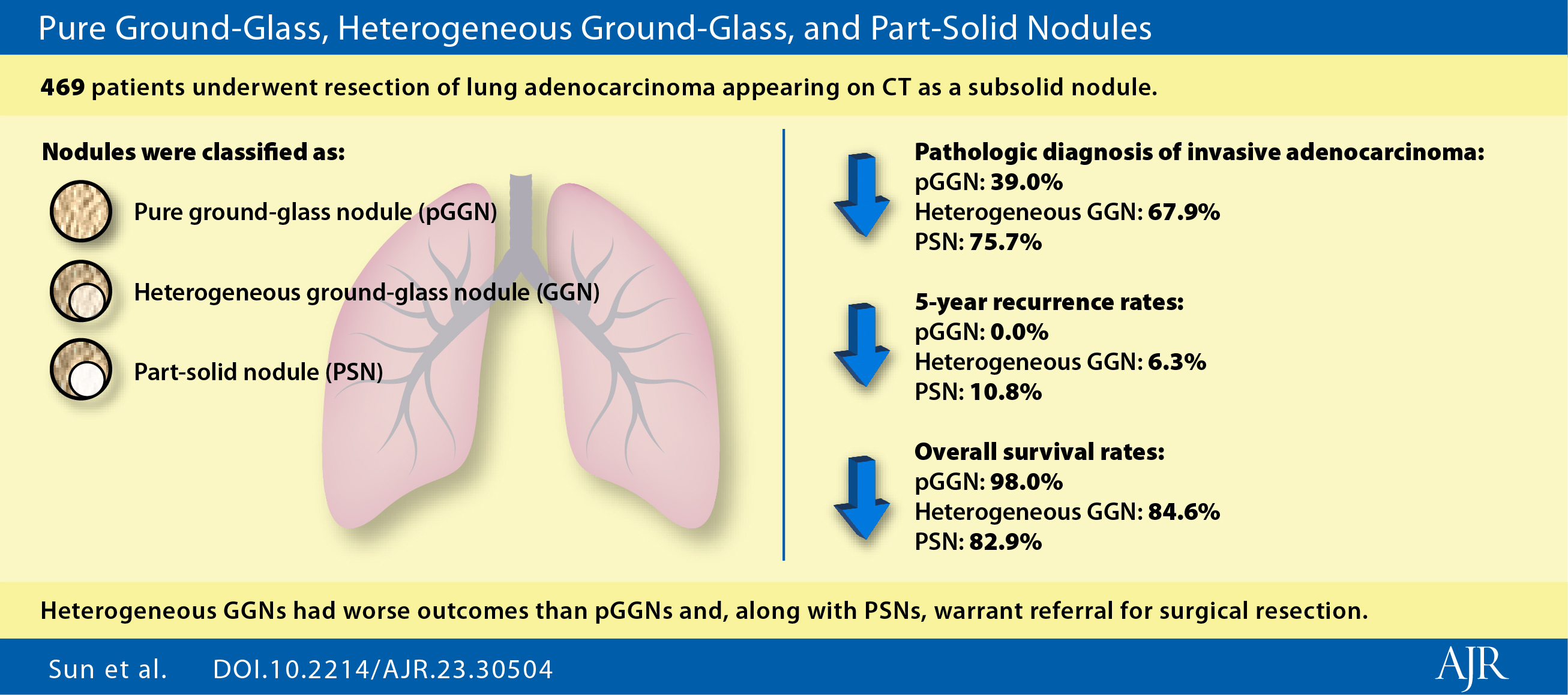
Image Credit: AGR
The study assessed outcomes such as the pathological diagnosis of invasive adenocarcinoma, 5-year recurrence rates (locoregional or distant), and recurrence-free survival (RFS) and overall survival (OS) over 7 years. Analysis was performed using Kaplan-Meier and Cox proportional hazards regression methods, censoring patients with incomplete follow-up data.
Individualised Approach of Subsolid Lung Nodules Management
The study investigated the clinical outcomes of resected subsolid lung nodules, comparing three types: pure ground-glass nodules (pGGNs), heterogeneous ground-glass nodules (heterogeneous GGNs), and part-solid nodules (PSNs). Of the resected subsolid nodules, 23.2% were classified as heterogeneous GGNs. The frequency of invasive adenocarcinoma at resection was 39.0% in pGGNs, 67.9% in heterogeneous GGNs, and 75.7% in PSNs. The 5-year recurrence rate was 0.0% in pGGNs, 6.3% in heterogeneous GGNs, and 10.8% in PSNs. Analysis over 7 years revealed recurrence-free survival (RFS) of 97.7%, 82.0%, and 79.4% and overall survival (OS) of 98.0%, 84.6%, and 82.9% in patients with pGGNs, heterogeneous GGNs, and PSNs, respectively. RFS and OS were significantly different between pGGNs and heterogeneous GGNs. Previous studies have shown high rates of invasive adenocarcinoma in resected subsolid nodules, raising questions about optimal management. The current study supports an individualised approach, with surveillance recommended for strictly defined pGGNs due to their indolent course. Heterogeneous GGNs exhibited more aggressive behaviour similar to PSNs, suggesting a need for definitive therapy such as resection.
Nodule Classification and Clinical Implications: Discrepancies and Future Directions
Nodule classification was based solely on lung windows, consistent with Fleischner Society guidelines, differentiating heterogeneous GGNs by internal increased attenuation not as dense as pulmonary vessels. However, this approach contrasts with earlier studies that required solid components visible on soft-tissue windows. Notably, the study's findings contradict previous observations of no recurrence after resection of heterogeneous GGNs. The study's limitations include its retrospective nature, heterogeneous follow-up durations, varying CT protocols, and subjective nodule assessment. Additionally, only surgically resected adenocarcinomas were analysed, excluding other treatments or diagnoses. Future prospective trials are needed to validate these results.
In summary, the study stratified subsolid pulmonary nodules into distinct groups with differing clinical outcomes. Surveillance is suggested for strictly defined pGGNs, while consideration of surgical management is proposed for nodules with internal increased attenuation, even without a true solid component. Prospective trials are essential for further validation.
Source: AJR
Image Credit: iStock