HealthManagement, Volume 15 - Issue 3, 2015
Patient portals are secure online websites that offer patients
access to personal health information. Basic portals (portals 1.0) are windows
into electronic records, built into or added on to existing electronic health
records (EHR). Portals 2.0 have advanced functionality, including health
information exchange and web 2.0 capabilities such as social networking. These
enable patients to make appointments, view test results, discharge summaries,
prescriptions or patient information material, update contact information, make
payments and exchange secure email with healthcare providers. The U.S.
government’s HealthIT.gov website declares: “With patient portal
implementation, your organization can enhance patient-provider communication,
empower patients, support care between visits, and, most importantly, improve
patient outcomes” (www.healthit.gov).
A ‘pull’ factor for patient portals is patient empowerment.
Patients and their families expect online access to their healthcare services
similar to what airlines, retail stores and banks offer, for example. In the U.S.
federal incentives provide the ‘push’ factor that obliges healthcare facilities
to provide portals. Meaningful Use (MU) refers to a U.S. federal government
incentive programme promoting implementation of EHR. From 2014, U.S. healthcare
services received incentives for having 50% of their eligible patient
population registered for access to a patient-facing portal website linked to
the EHR; having 5% of their eligible patient population actively viewing,
downloading, and transmitting health information through the portal; and
providing patient educational materials on these websites. Due to slow take-up,
the programme granted a one year extension until the end of 2015 for systems to
meet early patient engagement goals. Lyles and colleagues (2015) argue that
impediments to greater use appear to be issues with usability and medical
jargon and language written at a level requiring high educational attainment. They
write: “Healthcare providers often find themselves in the uncomfortable position
of needing to comply with the meaningful use mandate and therefore delivering
EHR-generated visit summaries that are full of medical jargon, do not reinforce
their recommendations, and do not enhance comprehension.” They recommend that
physician advocate for improvements in portal usability and that the government
body overseeing the programme, the Office of the National Coordinator for
Health Information Technology (ONC) supports usability testing among diverse populations
with significant health needs, creates standards for literacy and language appropriateness
for patient information, and provides incentives for broader implementation of
portal interfaces in multiple languages.
The Evidence
In theory, patient portals benefit both patients and healthcare
services. Staff time is saved when patients book appointments online, for
example. Against this are offset the costs of support and maintenance of the
portal. Patient satisfaction has been shown to increase when secure messaging
with healthcare staff is available, but it can add to staff workload (Shenson
et al. 2015). While patients over 65 do use patient portals, questions remain
about how to facilitate access by proxy for caregivers of patients who are unable
to access portals directly, but who wish to retain control of their information
(Crotty et al. 2015).
Providing access to a patient portal is a way to engage patients
in their own healthcare. A review by Irizarry and colleagues (2015) published
in the Journal of Medical Internet
Research explored research on patient
engagement through patient portals. Research has found that interest and
ability to use patient portals is linked to age, ethnicity, health literacy,
level of education, health status and caregiver role. People with disabilities
and chronic illness, frequent users of health services and caregivers of
elderly parents or children tend to be the most interested in patient portals.
Usability, such as easy registration and navigation, attention to privacy and
security considerations and endorsement by the healthcare provider also enhance
patients’ ability to engage with portals. The top patient portal functions were
regarded to be personalisation and collaborative communication between patients
and providers. The authors note that it is important to evaluate health literacy
and health numeracy “to identify specific risk factors and design flaws that could
impact patient comprehension and the accuracy of patient input and
interpretation of results." They add: “Ideally, interactive sites would
collect information on individuals’ health, health behaviours and personal
goals, and assess health literacy and functional ability, which would then
inform the adaptation of the patient portal to accommodate the needs of the individual
and/or what additional or alternative resources may be useful.” Kruse and
colleagues (2015a), in a systematic review of patient and provider attitudes
toward the use of patient portals for the management of chronic disease, found
that portals lead to improvements in self-management and improve the quality of
care. The positives of portals included patient-provider communication, while
the negatives were security concerns and user-friendliness. Cost was mentioned
in only a few of the articles they reviewed, and they suggest that the incentives
for meaningful use may lessen the cost barrier. The authors recommend that a
standard patient portal design providing patients with the resources to
understand and manage their conditions would improve portal adoption. In another
study they reviewed the effect of patient portals on quality outcomes and its
implications to meaningful use (Kruse et al. 2015b). Patient portal use showed
a higher retention rate of patient loyalty and lower missed appointment rates.
Portal use in the studies reviewed appeared to increase patient-to-provider
communication without unduly increasing workload or office visits. However,
results varied on improved outcomes. They recommend that
as most patient portal programmes are in their early stages, there is a need to
benchmark their advantages. Their review did not examine the effect of
Meaningful Use on portal use, due to insufficient data. They advocate that
patient portals be implemented “to allow for fewer timeconsuming encounters
between patients and providers as well as to enhance the accuracy of
information being exchanged” (Kruse et al. 2015b).
Patient Portals in Radiology
Radiology
is a clear candidate for patient portals. Image and report sharing can potentially
eliminate duplicate exams, improve communication and save money by removing the
need to produce and post CDs of images. Providing information to patients via a
portal has challenges, however, according to a survey by Henshaw and colleagues
published in the Journal of the American College
of Radiology (2015). They surveyed patients and
referring physicians following Kaiser Permanente Hawaii’s implementation of an
online patient portal in which doctors could manually release radiology reports
to patients (no images were included, but physicians can enter comments). The
researchers also held a group interview with referring physicians to gauge the
usefulness of releasing radiology reports through the patient portal, doctors’
preferences regarding automatic release, and the effect of releasing the reports
on workloads. The survey assessed patients’ opinions on accessibility,
importance of portal-released radiology reports, and communications with
referring physicians prior to and following the release of the reports (see
Figure 1).
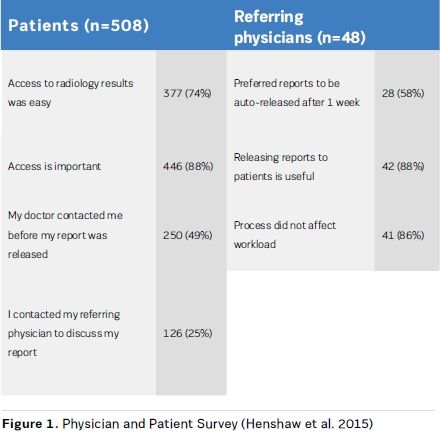
More
than half (58%) of the referring physicians favoured automatic release of x-ray
reports (with a 1 week delay). Fewer were in favour of auto-release of CT and
MRI reports. Most were in favour of communicating with patients when radiology
reports were released, using the messaging function within the system, which
includes smart phrases – standard text phrases entered with keyboard shortcuts.
Asked if using patient-friendly language in reports would remove the need to
communicate with patients when the report was released, most felt they still
needed to communicate. They did not favour using simpler language, as reports
would no longer meet their needs. However, they felt that a standard format for
the report would aid explanation of the results. In the case of more detailed
reports, such as for CT and MRI, they believed that communication could include
the most important information rather than including incidental findings.
The
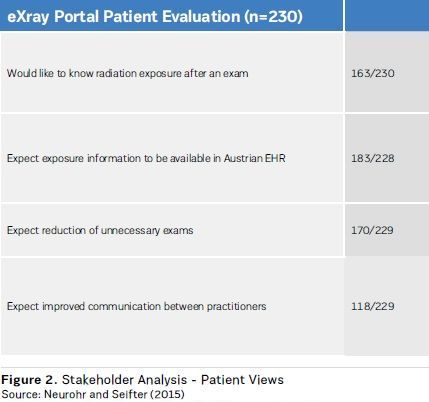
European Union project PAtients Leading and mANaging their healThcare through
Ehealth (PALANTE) included a pilot that enables patient access to a summary of
x-ray examination dosages in a personal record (Neurohr and Seifter 2015). The
eXray-Record extracts data directly from the hospital information system to
calculate relevant results of exposure to radiation during examinations and the
total acquired exposure in Styrian Hospital Cooperation (KAGes) hospitals. It
is integrated into the patient portal of the KAGes and is accessed via the
Austria Card. As of March 2015 over 1,400 physicians have accessed the record
with their patients and 270 patients have accessed the record outside the
hospital. Figure 2 shows patient expectations of the portal from a
pre-implementation stakeholder analysis.
At
the Hospital of the University of Pennsylvania (HUP) in the U.S., patient access
to radiology reports proved popular, according to Seetharam Chadalavada, who presented
at the Radiological Society of North America annual meeting in 2013 (Radiological
Society of North America 2014). Between May 2012-March 2013 over 150,000
patients activated portal accounts. Patients read about half of the radiology
reports available — comparable to lab result viewing. Release is delayed for three
days, except in the case of mammogram reports, for which a summary in lay language
is mandated. There was no change in the number of patient calls to clinics and
radiologists compared to the period before reports were made available.
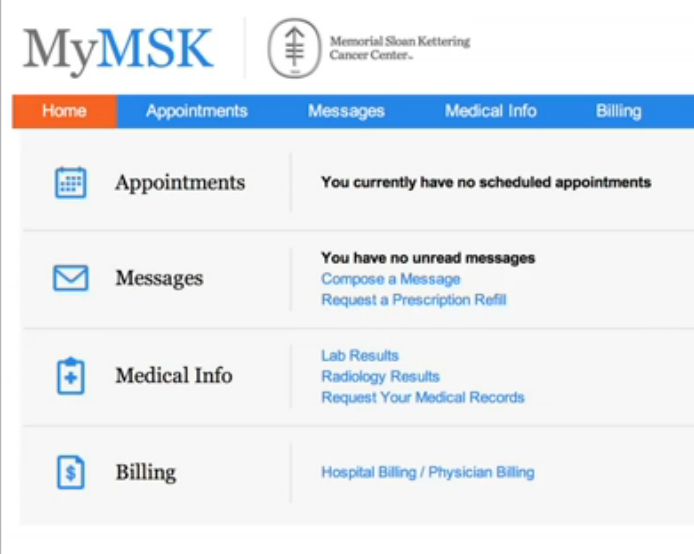
Memorial Sloan Kettering Cancer Center MyMSK Portal
Memorial
Sloan Kettering Cancer Center (MSKCC) in New York is the world’s oldest, largest
private cancer centre. The centre has 471 beds and has 935 attending physicians
and 2,221 nurses. In 2013, 138,338 patients were seen, there were 22,326
inpatient stays and 571,922 outpatient visits. The MyMSK portal application was
developed by MSK staff, and interfaces with many of MSKCC’s clinical backend
systems, as well as their own institutional database.
The portal went live in November 2006. In 2012 MKSCC released a fully
re-architected version 2.0, and in February 2015 the Center went live with an
iOS mobile version of MyMSK, which has topped 5000 downloads since. In June
2015 the Portal was certified for Meaningful Use - View Download Transmit.
HealthManagement.org
The Journal spoke to Kevin Shannon,
Manager of Patient Portal Development, to find out more about their experiences
in enabling patients to interact online with the Center.

Kevin Shannon
Manager of Patient Portal Development
Memorial Sloan Kettering Cancer Center
Features
MyMSK offers access to lab test results, the ability to make
appointments and secure messaging. Lab results go live when available.
Radiology results have a delay of four business days, which gives physicians
time to discuss findings with their patients. Patients can view medical information
related to each encounter and securely transmit that information to other
providers. The Portal Secure Messaging application allows staff to view and
reply to messages. The Information Systems department monitors usage and
response time to make sure all messages are replied to within 48 hours. Users
can also choose to send secure messages to the EHR to document communications
when appropriate.
Usage
Over the lifetime of the system nearly 70,000 patients have signed
up to use the portal. MyMSK currently has 49,000 active users. In an average
month almost 50% of those users log on at least once. An average of 53% of
patients who have had an active treatment appointment in a month have a portal
account.
What’s the feedback from patients on the portal?
Previous surveys always showed a high satisfaction rate, and we
feel our usage numbers show that patients find value in the application. We
recently met with a group of Patient Advisors and the feedback is positive, but
they suggest a lot of new functionality they would like to see.
What future plans are there for the portal?
We are currently expanding the portal to be used
by patients before they come in for their first visit, to help ease them
through the process of scheduling an appointment. We are also looking at
expanding our current integration with our Patient & Caregiver Education site
(www.mskcc. org/cancer-care/patient-education) to allow for building patient care plans. We
are also working on building and integrating an electronic forms system to
allow patients to complete a base medical history form as well as provide
surgical patients with pre- and post-surgery outcome surveys. In 2016 we hope
to work on an Android version of the mobile app and start planning for our next
major upgrade Portal 3.0.
Have you evaluated the cost-effectiveness of the portal in any way, for example, telephone time saved in making appointments, reduced phone enquiries?
Although we know that secure messaging is popular and widely used
(104,000 messages were sent in 2014), there has not been any formal analysis.
We also allow patients to confirm appointments online. When they do so it
eliminates us making a reminder phone call. Also, nurses have noted that most
questions now come via the portal and phone calls are less likely.
Are there any lessons learned from implementing the portal that you are able to share?
There are many departments that have some involvement in what content is presented on the portal, such as Labs, Scheduling, Billing, Nursing, Physicians etc. We created a Portal Working Group to bring all these areas together to help prioritise development and to make sure the portal presented a unified user experience. As good as it is to have input, it’s also good to have one sponsor/project manager to make the final decision. We also made sure to build a support function for patients. Since go-live there has been a Portal Help desk, available by phone or secure message, to assist patients with any issues or questions. The help desk staff attend the developer meetings and provide any issues or feedback they get from patients. We have been able to resolve software issues in a short timeframe and get back to the patient to let them know their problem or suggestion has been addressed. I think that shows them how much we care that their experience with the portal is satisfying.
References:
Crotty BH, Walker J, Dierks M et al. (2015) Information sharing preferences of older Patients and their families. JAMA Intern Med, Jul 6. doi: 10.1001/jamainternmed.2015.2903.
Henshaw D, Okawa G, Ching K et al. (2015) Access to radiology reports via an online patient portal: experiences of referring physicians and patients. J Am Coll Radiol, 12(6): 582-586.e1.
Irizarry T, DeVito Dabbs A, Curran CR. Patient portals and patient engagement: a state of the science review. J Med Internet Res. 2015 Jun 23;17(6):e148. doi: 10.2196/jmir.4255.
Kruse CS, Argueta DA, Lopez L et al. (2015a) Patient and provider attitudes toward the use of patient portals for the management of chronic disease: a systematic review. J Med Internet Res, 17(2): e40.
Kruse CS, Bolton K, Freriks G (2015b) The effect of patient portals on quality outcomes and its implications to meaningful use: a systematic review. J Med Internet Res, 17(2): e44.
Lyles C, Schillinger D, Sarkar U (2015) Connecting the dots: health information technology expansion and health disparities. PLoS Med 12(7): e1001852.
Neurohr P, Seifter P (2015) Evaluation of the Styrian personal exray-record. Stud Health Technol Inform, 212: 198-205.
Radiological Society of North America (2014) Radiology adopts—and adapts to—online patient portals. RSNA News, April 1. [Accessed: 20 July 2015] Available from http://rsna.org/newsdetail. aspx?id=11527
Shenson JA, Cronin RM, Davis SE et al. (2015) Rapid growth in surgeons’ use of secure messaging in a patient portal. Surg Endosc, Jun 27. [Epub ahead of print]

