The digital health sector faces significant data challenges due to its fragmented nature, hindering effective collaboration and resulting in suboptimal care, inconsistent services, and financial waste. Despite the potential of interoperable data to address these issues, efforts have been inconsistent, leading to numerous incompatible standards. A recent paper in the Journal of Medical Internet Research introduces a typology of healthcare data needs and discusses the challenges and advantages of open data standards. It recognises the diversity of viewpoints and needs addressed by different standards and identifies three domains of healthcare data, each with unique characteristics and challenges. Common and domain-specific requirements are outlined to guide the design of interoperable systems.
Domains and Standards in Healthcare Data Management
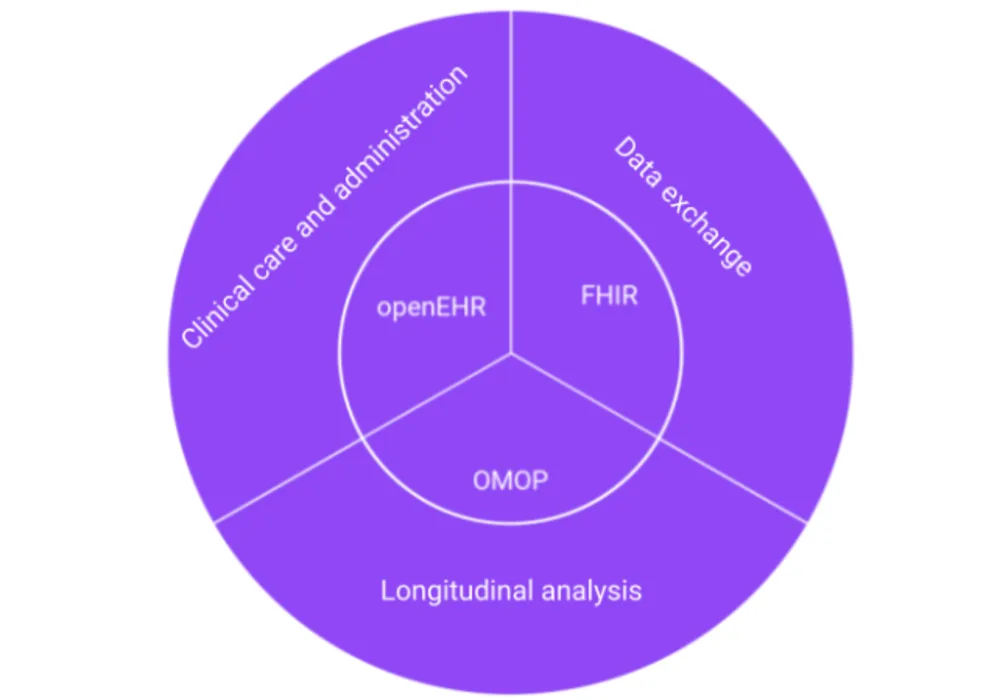
The three domains of health care data are Clinical Care and Administration, Data Exchange, and Longitudinal Analysis.
Clinical Care and Administration: This domain focuses on documenting clinical services for continuity of care and billing. Standards for electronic medical record interoperability aim to prevent vendor lock-in and enable easier transitions between systems using open standards.
Data Exchange: Records of care facilitate communication between healthcare providers and payers. Standards for data transmission should allow for immediate sharing of relevant information in small quantities, prioritising fidelity to local processes and terminology.
Longitudinal Analysis: This domain focuses on analysing patterns, trends, and predictors of health outcomes. Analytical methods require data aggregation from multiple sources and anonymisation to protect patient privacy. Fidelity to individual details is often sacrificed for statistical generalisations and patient privacy.
Role of Practicality, Feasibility, and Community in Healthcare Data Standards
Practicality, Feasibility, and Community play crucial roles in the effectiveness of data standards in the digital health sector. While technical suitability is essential, practical and socio-technical factors are equally significant. The balance between customizability and rigidity is crucial for standards to be implemented effectively. For example, the United States Core Data for Interoperability strikes such a balance, providing regulated core data elements that reduce the need for extensive customisation.
The adoption and improvement of data standards rely on community engagement. Standards widely used in the community are more beneficial for collaboration networks. Active community involvement fosters the evolution of standards, turning even basic ones into superior versions over time. Open standards have an advantage due to their accessibility for contribution and testing in diverse environments, although proprietary standards may have shorter improvement cycles due to more accessible governance.
Emerging Standards for Healthcare Interoperability
Emerging standards in healthcare interoperability aim to address the paradox of numerous overlapping standards, which complicate implementation and reduce interoperability. The proposal suggests converging on three key standards that are open, backed by active communities, and proven in their respective domains.
Clinical Care and Administration: openEHR offers a centralised database structure for health IT systems, facilitating efficient retrieval of patient records. Its patient-centric, extensible schema is preferred over proprietary formats, easing vendor transitions.
Data Exchange: HL7's FHIR standard provides a RESTful API for efficient data transfer, enabling real-world healthcare services like patient record management and appointment scheduling. FHIR's core sets streamline the continuity of care across different entities.
Longitudinal Analysis: OHDSI's OMOP Common Data Model is designed for longitudinal analysis of clinical records. Its patient-centric relational model facilitates complex queries to uncover patterns and trends using statistical and machine-learning techniques.
Paving the Way Towards Collaborative Harmonisation
Harmonisation efforts led by volunteer groups aim to provide standard transformations between these standards, facilitating interoperability. Collaborations between OHDSI, HL7, and openEHR foster a virtuous cycle of community participation, standard improvement, and simplification of harmonisation processes, benefiting global healthcare systems. When selecting a standard for healthcare interoperability, users can easily determine their focus on operational care delivery or analytics and identify the systems involved. An interoperable health system would use openEHR for data collection, FHIR for data transmission, and OMOP for data analysis. Transformations between standards can result in loss of fidelity, information, relationships, or accuracy, which should be minimised. Tacit or external knowledge can aid in this process.
Open standards with engaged communities offer advantages over proprietary ones, enabling broader contributions and continual improvement. True interoperability requires harmonisation among standards and migration pathways. Three open standards, openEHR, FHIR, and OMOP, are well-suited to their respective healthcare domains and supported by active and growing communities dedicated to their improvement.
Source & Image Credit: Journal of Medical Internet Research