PRINT OPTIMISED
Speech and language therapists play an integral role in identifying dysphagia risk factors, facilitating oral intake, and improving clinical outcomes.
Speech and Language Therapists (SLT) are recognised members of the multi-disciplinary team working in the Intensive Care Unit (ICU), with a focus on the rehabilitation of communication and swallowing difficulties (oropharyngeal dysphagia). Patients who are admitted to the ICU are likely to need support for at least two organs and this may include ventilatory support necessitating a tracheostomy. A number of studies have identified a link between insertion of an artificial airway and disruption to laryngeal functions, which includes both voice and swallowing (Brodsky 2018). In the UK, the role of SLT extends to the optimal management of secretions, supporting the weaning process from assisted ventilation to self-ventilation through to decannulation as well as facilitating a return to oral intake (Royal College of Speech and Language Therapists 2014). A great deal of therapy intervention may be required prior to consideration of oral intake during which time a patient will require non-oral nutrition to support them through their rehabilitation.
Normal Swallowing
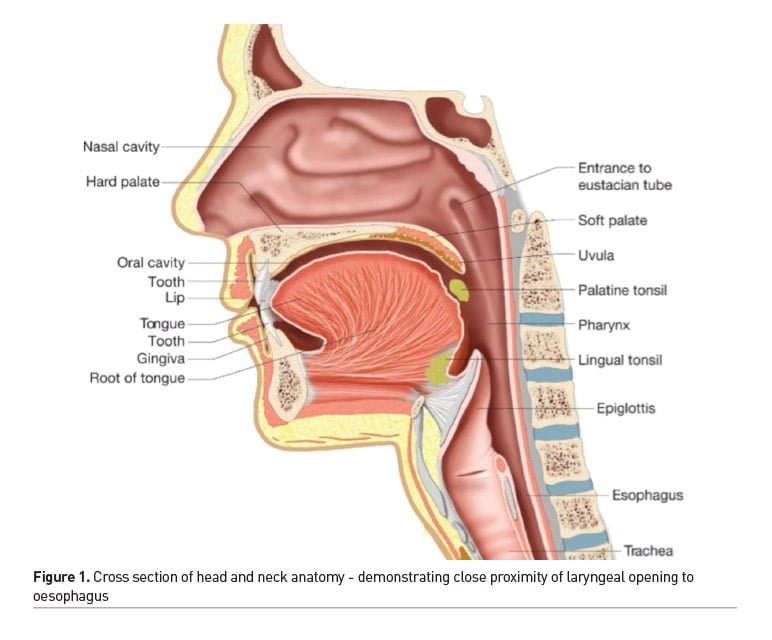
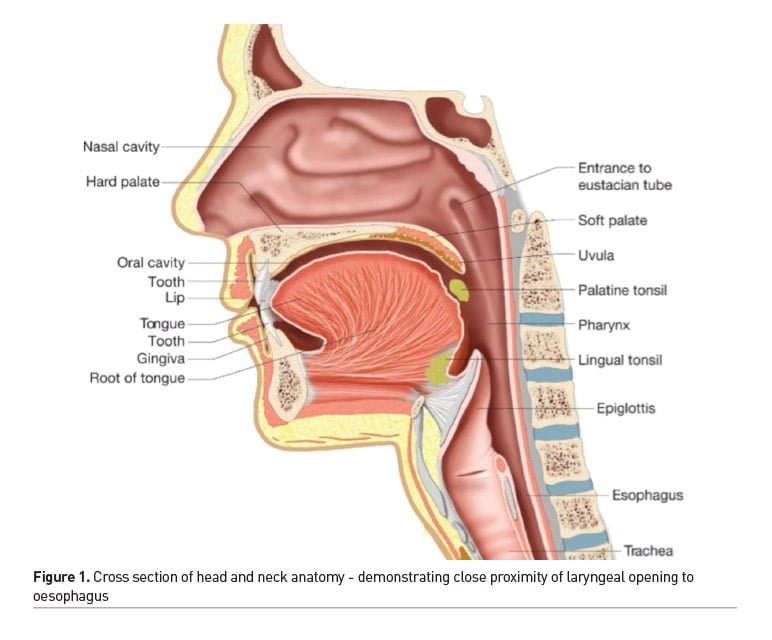
To better understand the disruption to swallowing, it is valuable to be familiar with the normal process of swallowing. This involves the precise coordination of reflexes and muscle movements across a three stage process (Groher and Crary 2015). At the oral stage, food or fluid is introduced into the mouth through the lips, then manipulated and controlled by the tongue to form a cohesive bolus that is then forced into the pharynx by the back of the tongue under pressure. This triggers the pharyngeal stage of swallowing leading to a series of biomechanical movements which raises and tilts the larynx to enable closure of the airway whilst simultaneously opening the oesophageal entrance (Figure 1). During the oesophageal stage the bolus transfers through the oesophagus to the stomach for further digestive processing (McRae 2018). Any disruption to the timing or range of movements at the oral or pharyngeal stage results in a risk of food or fluid entering the airway, with negative health consequences, such as chest infection and respiratory compromise. If food or fluid is not being absorbed into the digestive system, there is a loss of nutritional value which further compromises patients’ immunity to fight infection.
Causes of Oropharyngeal Dysphagia
As survivorship of patients increases in ICU, the awareness of the incidence of oropharyngeal dysphagia has also increased, due to its negative impact on mortality. Causes appear to be multi-factorial and include the primary diagnosis, especially neurological, respiratory interventions and ICU acquired weakness (Schefold et al. 2017). For this reason, it has been difficult to identify incidence with reports ranging from 3 to 62% (Skoretz et al. 2010).
Primary Diagnoses
A number of neurological disorders cause disruption to muscle strength and movement and interfere with normal swallowing. This includes stroke, progressive neurological disorders and traumatic brain injury. Infections and tumours in the oropharynx or nervous system can also cause disturbances to swallowing functions. Patients with neurological conditions in ICU are reported to require increased mechanical ventilation and extended lengths of stay with persisting dysphagia (Macht et al. 2013).
Respiratory Interventions
Many ICU patients will require an endotracheal tube or tracheostomy tube to assist ventilation during their admission. An increasing amount of evidence indicates that these can lead to mechanical and physiological disruption to laryngeal functions (Brodsky et al. 2018; Skoretz et al. 2010). This has been termed post-extubation dysphagia (PED) and is acknowledged as being a hidden condition with a high rate of silent aspiration, which demands early identification and intervention (Kwok et al. 2013; Perren et al. 2019).
ICU Acquired Weakness
This describes varying degrees of muscle weakness and atrophy that occurs in up to 80% of critical care patients, often due to immobilisation and disuse (Jolley et al. 2016). Pharyngeal dysfunction and dysphagia has been associated with muscle weakness in critically ill patients and linked to increased risk of aspiration, with poorer outcomes (Mirzakhani et al. 2013; Ponfick et al. 2015).
Regardless of cause, dysphagia has a negative impact on overall health status and mortality with higher healthcare costs (Altman et al. 2010). Despite increased awareness, routine swallow screening with a planned intervention is not standard practice in ICUs, but this may help to prevent symptoms of aspiration (Zuercher et al. 2019).
The Personal Impact of Dysphagia
It is important to consider the personal impact of not eating and drinking. Oral intake not only provides nutritional benefits but has psychological and emotional importance, adding significantly to quality of life (Barr and Schumacher 2003). Communal eating is often attached to family and social events, with many cultures using food and drink in celebration of life events. This needs to be a consideration in the clinical decision-making process, to ensure that social inclusion is maintained without compromise to health (Watson and Bell 2014). Studies have demonstrated the negative impact of not being able to eat that included shame, anxiety and dependence (Carlsson et al. 2004; Jacobsson et al. 2000; Larsen and Uhrenfeldt 2013). For patients in ICU, the process of resuming oral intake signifies recovery and a return to normality through reintegration into the daily routine of mealtimes and sharing food with friends and family (Segaran 2006). Consideration of the impact on quality of life is important when decisions are being made about long-term nutritional needs.
Clinical Management of Oropharyngeal Dysphagia
Recent UK guidance for critical care recommend that all tracheostomy patients are assessed by SLT as standard (Faculty of Intensive Care Medicine & Intensive Care Society 2019) although current levels of SLT staffing are unlikely to be able to achieve this. Instead, frontline staff, such as nurses, doctors and allied health professionals are expected to identify risk factors for dysphagia in order to expedite a referral to SLT for swallowing assessment.
Swallow Screening
A number of screening tools have been developed for early identification of dysphagia. The Water Swallow Test offers a quick assessment of aspiration by checking for overt signs of coughing or wet voice after taking sips of progressive amounts of water (Suiter & Leder 2008). For ICU patients, there remains a risk of false negative results in the event of silent aspiration so additional detailed SLT assessments may be required to verify clinical signs (Brodsky et al. 2016). Other screening tools employ a two-stage process, where staff first review a checklist of risk factors for dysphagia, if passed, the second stage allows water trials. Examples are the GuSS-ICU (Christensen and Trapl 2018) and the PEDS tool (Johnson et al. 2018) which allow early commencement of oral intake for those with no risk factors or dysphagia signs.
SLT Assessment
A swallow assessment by SLT will firstly involve a bedside evaluation to check range and strength of oral-motor movement, swallow timing, voice and cough. Gold standard instrumental assessments that support a definitive dysphagia diagnosis are Fibreoptic Endoscopic Evaluation of Swallowing (FEES) and Videofluoroscopy (VFS). For patients restricted to ICU, FEES offers portability and can be undertaken at the bedside to directly view the functions of the pharynx and larynx for speech, breathing and swallowing tasks (Langmore 2001). In contrast, VFS is a video-x-ray that takes place in the radiology department, with the patient being given radio-opaque coated food and drink of varying textures which is then recorded and analysed for swallow timing, speed and effectiveness (Logemann 1998). Based on these assessments, an intervention plan can be developed to address specific swallowing impairments.
Dysphagia Management Options
Non-oral
If assessments show that swallowing function is unsafe for fluids or food consistencies and there is evidence of aspiration, the SLT may make a recommendation for the patient to remain nil by mouth in order to undertake a programme of therapy to rehabilitate the swallowing impairment. To maintain nutrition, the team would need to decide on short- or long-term options for enteral feeding which may be via a nasogastric (NGT) or gastrostomy tube. National guidance recommend that those with dysphagia should have a 2-4 week trial of nasogastric feeding prior to a team review to consider prognosis and future feeding requirements (National Collaborating Centre for Acute Care 2006). There has been evidence to suggest that NGT can disrupt swallow physiology (Pryor et al. 2014), so if dysphagia is likely to be prolonged, a percutaneous endoscopic gastrostomy should be considered (Dwyer et al. 2002). This is a reversible procedure, so that when oral intake resumes the tube can be removed.
Dry Mouth
A strong feature of the acute experience of many ICU patients is the feeling of a dry mouth and a strong desire to drink to achieve relief from thirst (Arai et al. 2013). Dry mouth is often a side effect of medication, reduced oral intake and mechanical ventilation (Kjeldsen et al. 2018; Stotts et al. 2015). A dry mouth and throat can make it difficult to swallow or talk but for those with dysphagia who need to be nil by mouth drinking poses a dilemma, as this may introduce a risk of aspiration. Regular mouthcare as well as oral moisturisation using artificial saliva products (McRae 2011) or a thirst care-bundle (Puntillo et al. 2014) can help to provide relief whilst minimising risk and improve wellbeing during acute care.
Swallow Therapy Interventions
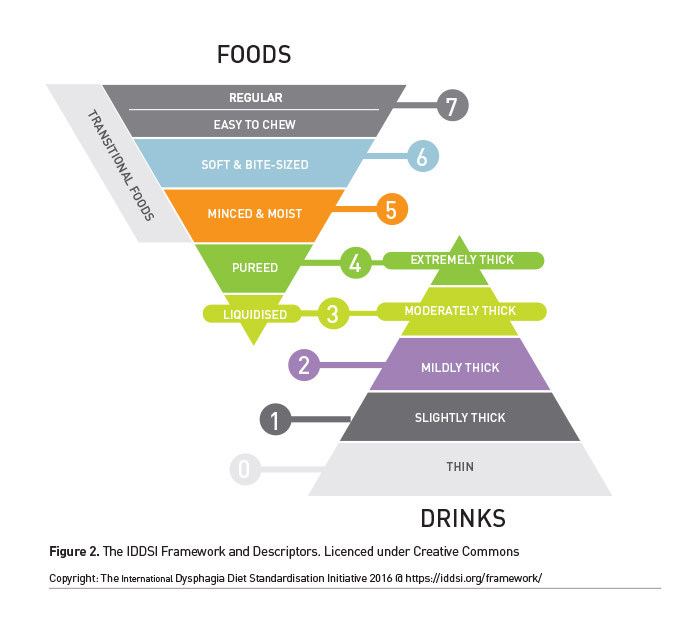
The SLT may identify specific impairments that can still permit safe swallowing with diet modifications to minimise risk of aspiration. The International Dysphagia Diet Standardisation Initiative (IDDSI) provides a universal framework to describe food and fluid textures on a continuum of eight levels (Figure 2). Oral intake will need to be supervised and a food chart kept, to track both amount and consistency of food and drink taken so that informed decisions are made to upgrade or downgrade diet textures.
Alongside a modified diet, SLTs may recommend a range of swallow exercises or strategies to improve motor and sensory functions of the oropharyngeal system to improve swallow safety and return to normal diet (Martino and McCulloch 2016).
Risk Feeding
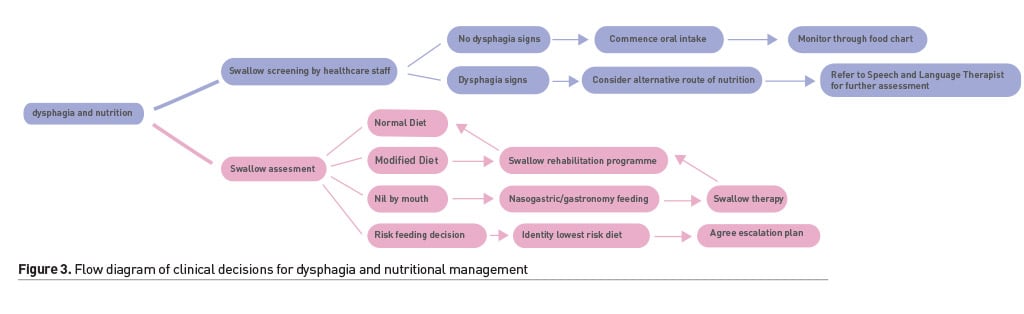
In some instances, there may be a decision to continue oral diet that is at risk of being aspirated, if alternatives are not an option. This is termed ‘risk-feeding’ or Eating and Drinking with Acknowledged Risk (EDAR). This may be considered as an option for patients who have significant multi-system impairments with poor prognosis, and alternative methods of nutrition may be unsuitable or unsafe (Hansjee 2018). This requires discussion and documentation of decisions with staff, family members and the patient, if possible. The SLT’s role will be to assess the patient’s swallowing to ensure the most risk-free textures are provided. As a team it is crucial to achieve an agreement on the course of action in the event of clinical deterioration. Use of a decision tool (Figure 3) for those with complex dysphagia can ensure that patients experience less time being nil by mouth and a patient-centred approach to decision-making (Sommerville et al. 2019).
Outcome Measures
There are a number of outcome measures to evaluate progress in dysphagia rehabilitation. Some are used by SLTs with instrumental assessments to describe the degree of impairment, such as the Penetration Aspiration Scale (Rosenbek et al. 1996), the Secretion Severity Rating scale (Murray et al. 1996) and Yale Pharyngeal Residue Severity Rating scale (Neubauer et al. 2015). Patient reported outcome measures provide insight into the impact dysphagia on the person and environment. The Functional Oral Intake Scale (FOIS) is a seven-point scale that describes the degree of swallowing function and oral intake or tube feeding required (Crary et al. 2005). The Swallowing Quality of Life Questionnaire (SWAL QOL) (McHorney et al. 2002) is a 44 item self-rating scale that helps to describe dysphagia symptoms, whilst the Eating Assessment Tool (EAT-10) (Belafsky et al. 2008) is a shorter 10 item list for people to describe their dysphagia severity and monitor changes.
Conclusion
SLTs are an integral member of the multidisciplinary team and have a role in the decisions around oral intake and interventions that may be required for those with dysphagia who will have compromised nutritional intake. Early identification of risk factors and management of impairments can help to ensure nutrition is optimised so that patients can participate in rehabilitation to improve their outcomes and quality of life.
Key Points
- In the UK, the role of Speech and Language Therapists (SLT) extends to the optimal management of secretions, supporting the weaning process from assisted ventilation to self-ventilation through to decannulation as well as facilitating a return to oral intake.
- Recent UK guidance for critical care recommend that all tracheostomy patients are assessed by SLT as standard.
- SLTs are an integral member of the multidisciplinary team and have a role in the decisions around oral intake and interventions that may be required for those with dysphagia who will have compromised nutritional intake.
Abbreviations
EAT Eating Assessment Tool
EDAR Eating and Drinking with Acknowledged Risk
FEES Fibreoptic Endoscopic Evaluation of Swallowing
FOIS Functional Oral Intake Scale
ICU Intensive Care Unit
IDDSI International Dysphagia Diet Standardisation Initiative
NGT Nasogastric
PED Post-Extubation Dysphagia
SWAL QOL Swallowing Quality of Life Questionnaire
SLT Speech & Language Therapists
VFS Videofluoroscopy
Conflict of Interest
None.
«« #LIVES2019: Highlights from the Opening Ceremony @ESICM
Join ICU Management & Practice at #LIVES2019 in Berlin
»»
References:
Altman KW, Yu GP, Schaefer SD (2010) Consequence of dysphagia in the hospitalized patient: impact on prognosis and hospital resources. Arch Otolaryngol Head Neck & Surg, 136(8):784-789.
Arai S, Stotts N, Puntillo K (2013) Thirst in Critically Ill Patients: From Physiology to Sensation American. Journal of Critical Care, 22(4):328-335.
Barr JT, Schumacher GE (2003) The need for a nutrition-related quality-of-life measure. Journal of the American Dietetic Association, 103(2):177-180
Belafsky PC, Mouadeb DA, Rees CJ, Pryor JC, Postma GN, Allen J, Leonard RJ (2008) Validity and Reliability of the Eating Assessment Tool (EAT-10). Annals of Otology Rhinology & Laryngology, 117(12): 919-924.
Brodsky MB, Levy MJ, Jedlanek E, Pandian V, Blackford B, Price C, Akst LM (2018) Laryngeal Injury and Upper Airway Symptoms After Oral Endotracheal Intubation With Mechanical Ventilation During Critical Care: A Systematic Review. Crit Care Med, 46(12):2010-2017.
Brodsky MB, Suiter DM, González-Fernández M, Michtalik HJ, Frymark TB, Venediktov R, Schooling T (2016) Screening Accuracy for Aspiration Using Bedside Water Swallow Tests: A Systematic Review and Meta-Analysis. Chest, 150(1):148-163.
Carlsson E, Ehrenberg A, Ehnfors M (2004) Stroke and eating difficulties: long-term experiences. J Clin Nurs, 13(7):825-834.
Christensen M, Trapl M (2018) Development of a modified swallowing screening tool to manage post-extubation dysphagia. Nursing in Critical Care, 23(2):102-107.
Crary MA, Mann GD , Groher ME (2005) Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch Phys Med Rehabil 86(8):1516-1520.
Dwyer KM, Watts DD, Thurber JS, Benoit RS, Fakhry SM (2002) Percutaneous endoscopic gastrostomy: the preferred method of elective feeding tube placement in trauma patients. J Trauma, 52(1):26-32.
Faculty of Intensive Care Medicine Intensive Care Society (2019) Guidelines for
the Provision of Intensive Care Services (GPICS) Edition 2 Retrieved from
https://wwwficmacuk/sites/default/files/gpics-v2pdf
Groher M E
Crary M (2015) Dysphagia: Clinical Management in Adults and Children
(Second Edition ed): Butterworth-Heinemann
Hansjee D (2018) An Acute Model of Care to
Guide Eating Drinking Decisions in the
Frail Elderly with Dementia and Dysphagia Geriatrics (Basel) 3(4)
doi:103390/geriatrics3040065
IDDSI (2019) International Dysphagia Diet
Standardisation Initiative Retrieved from https://iddsiorg/
Jacobsson C Axelsson K Osterlind P O Norberg A (2000) How people with stroke and
healthy older people experience the eating process J Clin Nurs 9(2) 255-264
doi:101046/j1365-2702200000355x
Johnson K L Speirs L Mitchell A Przybyl H
Anderson D Manos B Winchester K (2018)
Validation of a Postextubation Dysphagia Screening Tool for Patients After
Prolonged Endotracheal Intubation American Journal of Critical Care 27(2) 89-96
doi:104037/ajcc2018483
Jolley S E Bunnell A E Hough C L (2016) ICU-Acquired Weakness Chest
150(5) 1129-1140 doi:101016/jchest201603045
Kjeldsen C L Hansen M S Jensen K Holm A
Haahr A Dreyer P (2018) Patients'
experience of thirst while being conscious and mechanically ventilated in the
intensive care unit Nurs Crit Care 23(2) 75-81 doi:101111/nicc12277
Kwok A M Davis J W Cagle K M Sue L P Kaups K L (2013) Post-extubation dysphagia in
trauma patients: it's hard to swallow The American Journal of Surgery 206(6)
924-928 doi:http://dxdoiorg/101016/jamjsurg201308010
Langmore S (2001) Endoscopic evaluation and
treatment of swallowing disorders New York: Thieme
Larsen L K
Uhrenfeldt L (2013) Patients’ lived experiences of a reduced intake of
food and drinks during illness: a literature review Scandinavian Journal of
Caring Sciences 27(1) 184-194 doi:101111/j1471-6712201200977x
Logemann J (1998) Evaluation and Treatment
of Swallowing Disorders (2nd ed) Austin TX: Pro-Ed
Macht M King C J Wimbish T Clark B J Benson
A B Burnham E L Moss M (2013)
Post-extubation dysphagia is associated with longer hospitalization in
survivors of critical illness with neurologic impairment Crit Care 17(3) R119
Martino R
McCulloch T (2016) Therapeutic intervention in oropharyngeal dysphagia
Nature Reviews Gastroenterology
Hepatology 13 665 doi:101038/nrgastro2016127
McHorney C A Robbins J Lomax K Rosenbek J C
Chignell K Kramer A E Earl Bricker D
(2002) The SWAL-QOL and SWAL-CARE Outcomes Tool for Oropharyngeal Dysphagia in
Adults: III Documentation of Reliability and Validity Dysphagia 17(2) 97-114
doi:101007/s00455-001-0109-1
McRae J (2011) Dry mouth in spinal cord
injury: causes and treatment Dental Nursing 7(8) 446-449 Retrieved from
http://wwwdental-nursingcouk/cgi-bin/gopl/library/abstracthtml?uid=85492
McRae J (2018) The role of speech and
language therapy in critical care ICU Management Practice 18(2) 128-131
Mirzakhani H Williams J-N Mello J Joseph S
Meyer M J Waak K Eikermann M (2013)
Muscle Weakness Predicts Pharyngeal Dysfunction and Symptomatic Aspiration in
Long-term Ventilated Patients Anesthesiology 119(2) 389-397 doi:101097/aln0b013e31829373fe
Murray J Langmore S E Ginsberg S Dostie A (1996) The significance of
accumulated oropharyngeal secretions and swallowing frequency in predicting
aspiration Dysphagia 11(2) 99-103 doi:101007/bf00417898
National Collaborating Centre for Acute
Care (2006) Nutrition Support for Adults Oral Nutrition Support Enteral Tube
Feeding and Parenteral Nutrition: methods evidence and guidance (CG32)
Retrieved from https://wwwniceorguk/guidance/cg32
Neubauer P D Rademaker A W Leder S B (2015) The Yale Pharyngeal Residue
Severity Rating Scale: An Anatomically Defined and Image-Based Tool Dysphagia
30(5) 521-528 doi:101007/s00455-015-9631-4
Patel D A Sharda R Hovis K L Nichols E E
Sathe N Penson D F Francis D O (2017)
Patient-reported outcome measures in dysphagia: a systematic review of
instrument development and validation Dis Esophagus 30(5) 1-23
doi:101093/dote/dow028
Perren A Zürcher P Schefold J C (2019) Clinical Approaches to
Assess Post-extubation Dysphagia (PED) in the Critically Ill Dysphagia
doi:101007/s00455-019-09977-w
Ponfick M Linden R Nowak D A (2015) Dysphagia—A Common Transient
Symptom in Critical Illness Polyneuropathy: A Fiberoptic Endoscopic Evaluation
of Swallowing Study Critical Care Medicine 43 365–372 Retrieved from http://wwwncbinlmnihgov/pubmed/25377021
Pryor L N Ward E C Cornwell P L O'Connor S
N Finnis M E Chapman M J (2014) Impact
of nasogastric tubes on swallowing physiology in older healthy subjects: A
randomized controlled crossover trial Clin Nutr doi:101016/jclnu201409002
Puntillo K Arai S R Cooper B A Stotts N
A Nelson J E (2014) A randomized
clinical trial of an intervention to relieve thirst and dry mouth in intensive
care unit patients 40(9) 1295-1302 doi:101007/s00134-014-3339-z
Rosenbek J C Robbins J A Roecker E B Coyle
J L Wood J L (1996) A
penetration-aspiration scale Dysphagia 11(2) 93-98 Retrieved from
https://wwwncbinlmnihgov/pubmed/8721066
Royal College of Speech and Language
Therapists (2014) Speech and Language Therapy in Adult Critical Care: Position paper
Retrieved from
https://wwwrcsltorg/members/publications/publications2/criticalcare_positionpaper_060114
Schefold J C Berger D Zürcher P Lensch M
Perren A Jakob S M Takala J (2017)
Dysphagia in Mechanically Ventilated ICU Patients (DYnAMICS): A Prospective
Observational Trial Critical Care Medicine 45(12) 2061-2069
doi:101097/ccm0000000000002765
Segaran E (2006) Returning to normal: The
role of eating in recovery from a critical illness BJNN 2(3) 141-148
doi:doi:1012968/bjnn20062321103
Skoretz S A Flowers H L Martino R (2010) The incidence of dysphagia
following endotracheal intubation: a systematic review Chest 137
doi:101378/chest09-1823
Sommerville P Lang A Archer S Woodcock
T Birns J (2019) FORWARD (Feeding via
the Oral Route With Acknowledged Risk of Deterioration): evaluation of a novel
tool to support patients eating and drinking at risk of aspiration Age and
Ageing 48(4) 553-558 doi:101093/ageing/afz050
Stotts N A Arai S R Cooper B A Nelson J
E Puntillo K A (2015) Predictors of
thirst in intensive care unit patients Journal of Pain and Symptom Management
49(3) 530-538 doi:101016/jjpainsymman201407001
Suiter D M
Leder S B (2008) Clinical utility of the 3-ounce water swallow test
Dysphagia 23(3) 244-250 doi:101007/s00455-007-9127-y
Watson N
Bell C (2014) Cultural Considerations in Tube Feeding Decision-Making
SIG 14 Perspectives on Communication Disorders and Sciences in Culturally and
Linguistically Diverse (CLD) Populations 21(2) 63-73 doi:101044/cds21263
Zuercher P Moret C S Dziewas R Schefold J C (2019) Dysphagia in the
intensive care unit: epidemiology mechanisms and clinical management Critical
Care 23(1) doi:101186/s13054-019-2400-2