At
first glance, America is making great strides toward a medical and
cultural shift in its approach to end-of-life care: More and more
providers are recognizing the benefits of hospice, more people are dying
at home, and many health care organizations are institutionalizing the
discussions between providers and patients that would help patients
formalize their wishes for end-of-life care through an advance
directive.
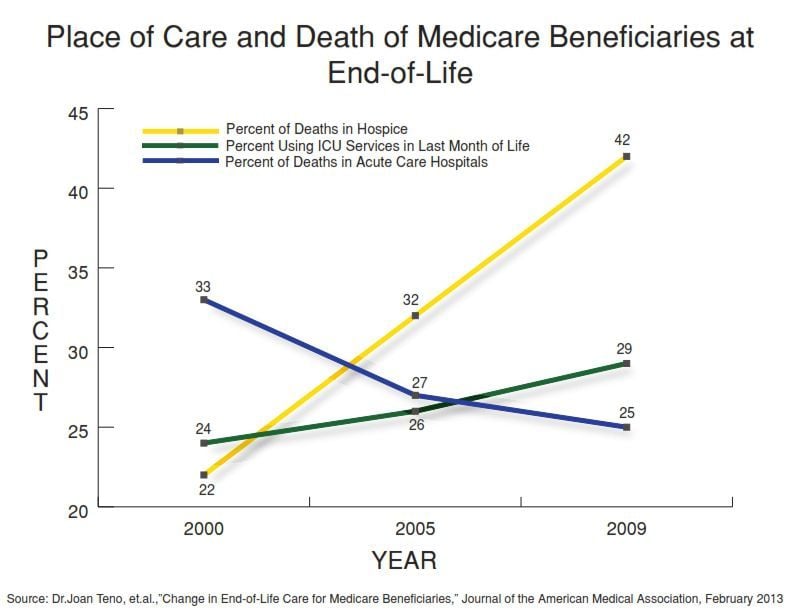
But pull up the curtain on these statistics, and the
drama that unfolds tells a very different story. End-of-life care
continues to be characterized by aggressive medical intervention and
runaway costs.
Like so many other problems plaguing the financing
and quality of health care in America, the end-of-life dilemma is
rooted in Medicare’s fee-for-service payment structure, says Joan M.
Teno, MD, lead author of a revealing study published in the Journal of the American Medical Association in February.
The
study found that fewer individuals are dying in hospitals than in the
past and more are receiving hospice care. Yet more patients are
receiving care in an intensive care unit in their last month of life and
a growing number are shuffled around between different care sites in
their final 3 months.
“What you pay for is what you get,” Teno
said in an interview with JAMA after the study’s release. “There are
financial incentives to provide more care in fee-for-service care. We
don’t get paid to talk with patients about their goals or care or
probable outcomes of care. We do pay for hospitalizations, and there are
financial incentives for nursing homes to transfer patients back to
acute care.”
End-of-Life Care Costs
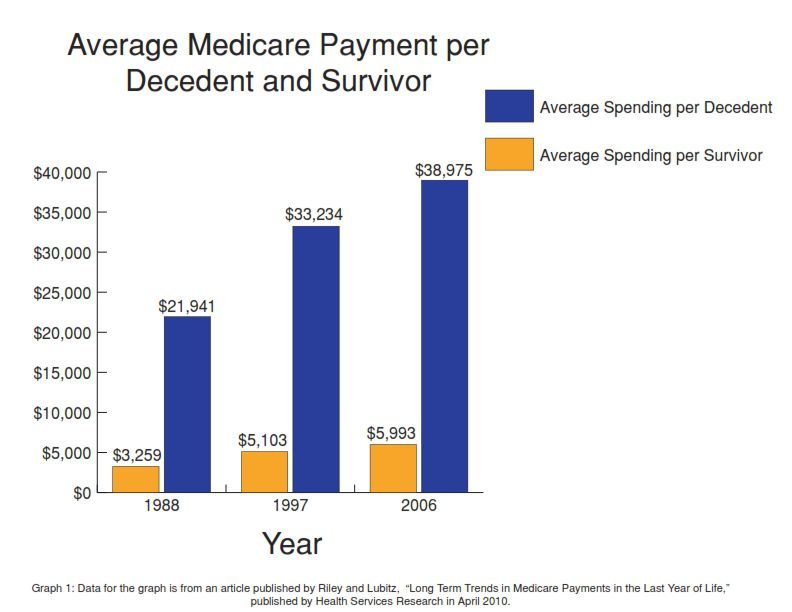
The
merits of increasingly aggressive treatment have been debated, but most
experts say that the use of multiple and intensive services at the end
of life is of little clinical benefit to the patient, and in many cases,
brings chaos and pain to what could otherwise be a peaceful dying
experience. Dr. Atul Gawande’s account, “Letting Go,” inThe New Yorker illustrates the heartbreaking effects of over treatment.
Gawande’s
story chronicles the medical care of Sara Monopi—a young woman
diagnosed with cancer who suffered through four rounds of chemotherapy,
radiation, numerous hospitalizations and at least two experimental
treatments, even though her doctors knew her condition was incurable.
Sara eventually succumbed to her death, but only after undergoing
expensive and unnecessary treatment that left her pained, exhausted and
eventually unconscious. Gawande writes, “Almost nothing we’d done to
Sara—none of our chemotherapy and scans and tests and radiation—had
likely achieved anything except to make her worse. She may well have
lived longer without it.”
Hospice physician Dr. Joanne Lynn
describes the current approach to end-of-life care as wasteful and
misdirected. Lynn, Director of the Center for Elder Care and Advanced
Illness at the Altarum Institute, a health systems research and
consulting organization, says per-capita costs will go down
significantly if we reduce the number of hospitalizations and procedures
Medicare beneficiaries endure during their last days.
“Right now
there’s nearly a blank check on Medicare-type costs,” Lynn said. “We
can have people go through extra imaging studies, we can have them go to
surgeries, we can have them go into hospitals over and over again. If
instead we mobilized services to their homes and greatly adapted the
services so that they really met people’s needs, we probably would use
hospitalization much less. We would use high-cost interventions and
imaging studies and diagnostic tests much less.”
Research supports Lynn’s observations. A 2009 Social Security Advisory Board report advocates
for a decrease in treatments and procedures that ultimately do not
benefit patients. The report states that research on Medicare costs and
services suggests that the government could achieve savings across the
health care spectrum by reducing the use of unnecessary medical services
that don’t actually improve beneficiaries’ health.
Others in the
field, such as Terry Berthelot, a senior attorney with the Center for
Medicare Advocacy and member of the National Council of Hospice and
Palliative Care Professionals, have voiced similar skepticism about the
over-use of medical services in end-of-life care.
“Currently,
the way we provide health care at the end of life is sort of crazy, only
focusing on the immediate problem rather than on the person,” Berthelot
said. “The health care system focuses on patching a person up and
sending her home when she shows up at the hospital. Long-term care plans
for the trajectory of a patient’s illness beyond the hospital doors are
often neglected. That kind of care is driving up our cost.”
Not only is it driving up costs, says Lynn, but Medicare’s
orientation toward hospitalization and excessive use of health services
at the end of life could cause a tragic setback in the fragile cultural
gains the United States has made in caring for its frail elderly.
When Lynn first started working in nursing homes in 1978, there were states where many frail and elderly patients were tied to their beds day in and day out. Since then, the way the United States treats the old and infirmed has improved.
As the baby boomer population ages into
Medicare, which is already suffering from its own poor financial health,
the consequent rising health care costs could break the back of our
nation’s long-term care system. Unless we change the way we approach
care management for those nearing the end of life, she says, we could
easily slip back to the darker days of nursing home care.
"We
will either bankrupt families and communities and the nation as a whole,
or we will learn to walk out on people. The better course would be to
try to find highly efficient ways to take care of one another in a
reliable way," she said. "Are we really going to learn to just warehouse
people again, tie them down to the bed, just ignore pressure ulcers,
ignore liberty and choice? Now is the time to do one step better. The
better has to be more efficient. It can’t just run up the costs."
Containing Costs by Planning for the End
Research
has shown that planning ahead for end-of-life care through advance
directives, which allow patients, if they are incapacitated, to specify
ahead of time what actions should be taken regarding their treatment,
could reduce spending. The use of advance directives specifying
end-of-life care limitations led to significantly lower levels of
Medicare spending in geographic regions that had had relatively high
end-of-life costs, according to a 2011 study published in The Journal of the American Medical Association.
Berthelot
recommends that doctors receive training regarding how to carry on
discussions about end-of-life treatment decisions starting when the
patient is young and healthy, framing it so that the focus is on quality
of life and giving the patient the kind of care that they want. “Honesty in conversation, rather than constantly focusing just on what
the next medical procedure will be, would make a huge difference for
the kind of care people get, that they get to make real choices about
that kind of care,” she said.
Providers should engage in ongoing,
meaningful conversations with patients when they’re healthy about what
matters to them when it comes to the care they receive as they near the
end of life, she said.
Director of Research for the Hospice and
Palliative Care Nurses Association June Lunney agreed that doctors and
patients need to have conversations about end-of-life care so that
seniors can make informed decisions about the treatments they do or
don't want to receive. Lunney helped develop the support from the
National Institutes on Health for research on end-of-life issues and
worked at the RAND Corporation's Center for End-of-Life Care.
Berthelot says advance directives could be the holy grail of America’s end-of-life crisis.
“They
can save our system a great deal of money because currently folks are
getting all types of end-of-life care that’s very, very expensive that
doesn’t in any way save lives. It only prolongs life at a huge cost with
very, very little real benefit because of all of the misery at the end
of life when somebody’s dying in a hospital,” she said.
Is Hospice the Answer?
Hospice
care toward the end of life often helps people live longer, Berthelot
said. “A big part of that is the fact that they don’t bounce back and
forth between home and the hospital and the skilled nursing facility and
that their care is being managed,” she said. “Good hospice care is an
example of seeing the person as the unit of care, rather than the
illness. The focus is on the whole person…the focus is on quality of
life.”
There is a rise in the use of hospice care. Medicare
beneficiaries’ use of hospice services has nearly doubled over the past
decade, according to a 2012 MedPAC report.
In 2010, 44 percent of beneficiaries who died that year used hospice,
an increase from 23 percent in 2000. But again, these numbers depict a
false sense of progress.
Among the Medicare beneficiaries in
Teno’s study, more than a quarter were in hospice care for less than 3
days-not nearly long enough to realize the benefits of the program. And
among the patients referred to hospice late, more than 40 percent were
hospitalized and spent time in the intensive care unit prior to
referral.
Lunney echoed the concerns raised by the JAMA study.
She says that short hospice stays don’t lead to better quality of life
for patients in their last days.
“We don’t know what the ideal
length of stay is, but less than seven days is not enough time. Putting
people into hospice care at the last minute doesn’t allow time for
providers to manage the patients’ symptoms well,” she said.
The
median hospice stay length hasn’t changed significantly over the past
decade, Harvard Medical School professor David G. Stevenson wrote in a
2012 article in The New England Journal of Medicine. The
median stay only rose from 17 days in 2000 to 18 days in 2010,
reflecting the fact that a sizable minority of beneficiaries goes into
hospice care mere days before their deaths, Stevenson wrote.
Lynn said that the hospice model, while it laudably improves the quality of the dying experience, may not be the panacea of cost-savings Medicare needs. In fact, she says, increased use of hospice may actually end up contributing to the cost quandary afflicting end-of-life care because the benefit hasn’t been adapted to deal with the clinical picture of today’s dying.
She said the issue is that the hospice care model
is built around patients who are rapidly declining, rather than the
patients she classifies as the “frail population”: those with multiple
chronic conditions and ambiguous prognoses.
“For someone whose
main problem is dementia, the hospice design was not well adapted,” she
said. “It may even increase the costs because the timing of death is
quite unpredictable. Lots of people will end up having to be discharged
from hospice after having used many months of what is a pretty high-cost
intervention.”
The population that hospice care serves has
changed significantly since the advent of the Medicare benefit for it,
according to Stevenson’s article. In 1990, 16 percent of Medicare
hospice care recipients had non-cancer diagnoses. As of November 2012,
it was more than two-thirds, rather than conditions such as heart
failure and dementia, Stevenson wrote.
Lynn says hospice is part
of the solution to the U.S. health care system’s end-of-life care
issues, but it’s going to need some redesign first. Nevertheless, Lynn
believes it’s imperative that the country figure out and enact the
solution to the end-of-life care model’s issues, or Americans will face a
choice between bankrupting themselves or abandoning their elders.
Source: Medicare NewsGroup



























