HealthManagement, Volume 23 - Issue 1, 2023
Key Points
- While mortality from the pandemic mainly affected older people, the pandemic also affected greatly the mental and physical health of young people in Europe, with large numbers reporting unmet needs for mental health care.
- In addition, the disruption of health services during the peak waves of the COVID-19 crisis created a backlog of patients waiting to receive primary, mental health, cancer, chronic and elective care, with the recovery period in different countries affected by the length and degree of disruptions and the ability to mobilise additional resources to increase activities following these disruptions.
- The pandemic has revealed the need to prioritize not only communicable disease prevention, but also the prevention of non-communicable diseases notably by addressing behavioural and environmental risk factors that have major impacts on people’s health and mortality.
Introduction
The pandemic has had a dramatic impact on people’s lives in Europe and around the world. It has led to a reduction of more than one year in life expectancy in the EU in 2021 compared with the pre pandemic level – the largest drop observed in most EU countries since World War II. By the end of October 2022, more than 1.1 million COVID 19 deaths had been reported across the 27 EU countries. Over 90% of these deaths have occurred among people aged over 60.
The 2022 edition of Health at a Glance: Europe examines key challenges European countries must address to develop stronger and more resilient health systems following the acute phase of the COVID-19 pandemic. It includes a special focus on how the pandemic has affected young people’s mental and physical health, and assesses the pandemic’s disruption of a wide range of health services for non-COVID patients and the policy responses to minimise the adverse consequences of these disruptions. The report also addresses a number of important risk factors to health that have exacerbated the impact of the pandemic, highlighting the need to put a greater focus on the prevention of both communicable and non-communicable diseases.
A Major Impact on the Mental and Physical Health of Young People
While few people’s lives have been unaffected by the pandemic, there have been concerns about the mental and physical health of the millions of young Europeans whose formative years have been marked by fear, uncertainty and disruption – particularly given the critical importance of early experiences in shaping health and well-being later in life. Prolonged periods of social isolation and break in education and employment opportunities seriously disrupted the lives and routines of young people at a critical time of their physical and social development.
School closures, the closure of sports facilities and other mobility restrictions were associated with a reduction in physical activity amongst children and adolescents in virtually all European countries with available data. Alongside a decline in physical activity during the pandemic, many children and young people experienced a worsening of their nutrition habits and developed increased sedentary behaviour such as staying seated and screen time, with indications of a rise in child overweight and obesity in some countries.
The pandemic and the measures implemented to contain it fuelled an unprecedented worsening of population mental health, with the prevalence of symptoms of depression amongst young people (aged 18-29) more than doubling in several European countries such as Belgium, Estonia, France, Sweden and Norway (Figure 1). Young people in precarious financial circumstances and young people at risk of exclusion were at particularly high risk of mental distress.
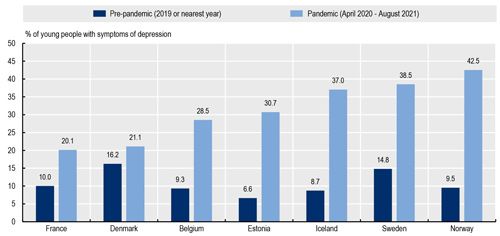
Source: OECD/European Union (2022), Health at a Glance: Europe 2022, Chapter 1
The pandemic also
disrupted mental health services, particularly during the first wave. The
measures implemented to contain the pandemic not only disrupted the
prevention and identification of mental health issues, but also their
treatment. Following the initial disruption, the demand for mental health care
has increased in many European countries, challenging alreadystretched mental
health care systems. One in two young Europeans with unmet healthcare needs
reported that these unmet needs were related to mental health care in spring
2021 and in spring 2022 (Figure 2).
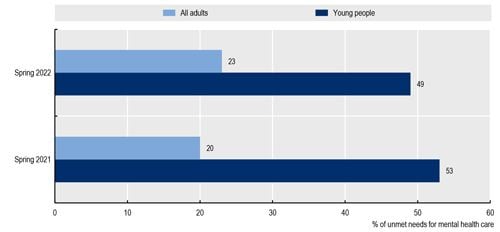
Source: Eurofound (2022), Fifth round of the Living, working and COVID-19 e-survey: living in a new era of uncertainty, reproduced in OECD/European Union (2022), Health at a Glance: Europe 2022, Chapter 1.
Care Disruptions During the Pandemic Led to Backlog of Patients for Cancer and Elective Care
The pandemic also disturbed the provision of care for other non-COVID patients. Disruptions in primary care, cancer screening and treatment, care continuity for people with chronic conditions, and elective (non-urgent) surgery were especially severe during peaks of the epidemic and lockdown periods.
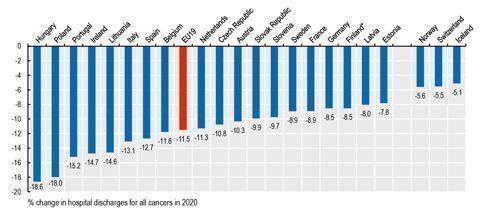
During the first months of the pandemic in spring 2020, disruptions in cancer screening and early detection programmes resulted in increased number of cancer cases being diagnosed at a later stage, reducing survival probabilities. Many countries were able to offset some of the initial reductions in cancer screening by scaling up activities in the second half of the year. However, screening rates for breast and cervical cancer still fell by 6% on average in EU countries in 2020. Delays in cancer screening resulted in a substantial reduction in the number of patients admitted to hospital for cancer care in 2020 (Figure 3), raising concerns about timely treatment.
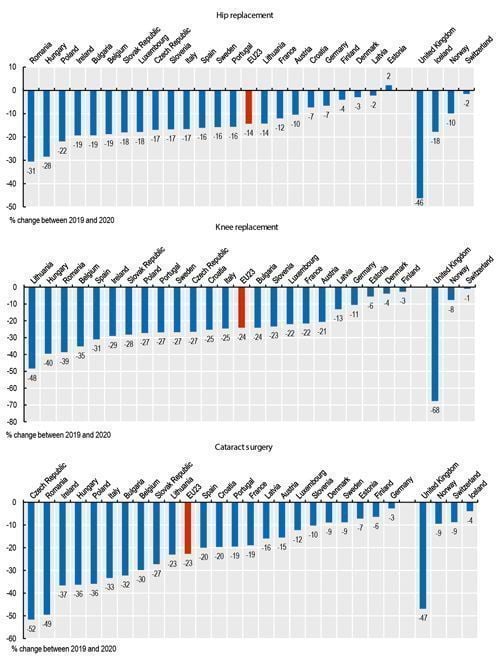
Most EU countries
suspended elective care at different times during the pandemic to divert
efforts towards COVID-19 patients and avoid people being infected while
seeking care. This created a backlog of patients awaiting elective
interventions, generating longer waiting lists and waiting times. In 2020, 2
million fewer elective surgical procedures were performed than in 2019 across
EU countries – a decrease of one sixth compared to pre pandemic volumes.
Hip replacements fell on average by 14% in 2020 compared with 2019, whilst
reductions in knee replacements and cataract operations were even larger in
most EU countries, falling by 24% and 23% on average (Figure 4). These “missing
volumes” of operations have increased waiting times for patients. Many EU countries
have provided additional funding to address these backlogs, but the main
constraint to scaling up volumes of surgical procedures has been shortages of
health workers. Incentives were provided to staff to work longer hours, but
these clearly had limits and ran the risk of leading to burnout and
resignation.
The Development of Teleconsultations Offset at Least Partly the Reduction in In-Person Consultations
On a more positive side, the rapid development of teleconsultations at the beginning of the pandemic helped to maintain access to care, in particular for patients with chronic conditions. In some countries, the overall number of teleconsultations and in-person consultations in 2020 exceeded the number in 2019 because the increase in teleconsultations more than offset any reduction in in-person consultations (Figure 5). Although it is encouraging that the vast majority of people who used telemedicine expressed high satisfaction, there are nevertheless concerns that some teleconsultations provide little benefit and that teleconsultations pose risks of widening health inequalities through digital exclusion for older and poorer people and those living in rural areas.
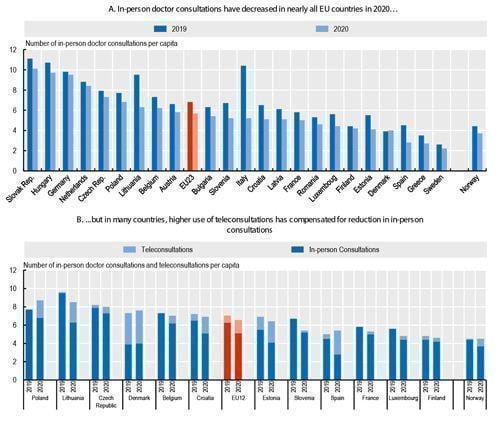
Source: OECD/European Union (2022), Health at a Glance: Europe 2022,Chapter 2
Reducing Risk Factors and Prioritising the Prevention of Infectious and Non-Communicable Diseases
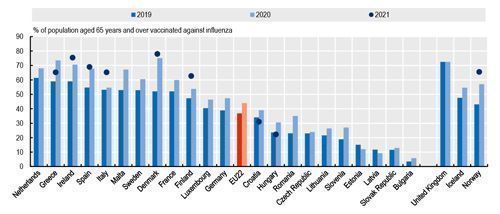
Health at a Glance: Europe 2022 also highlights that despite much talk about the importance of prevention, health spending remained overwhelmingly focused on curative care before the pandemic, with only 3% of total health spending going toward prevention on average. In 2020, most EU countries substantially increased their spending on prevention, at least temporarily, to fund testing, tracing, surveillance and public information campaigns related to the pandemic. In 2021, large additional resources were allocated to the roll-out of COVID 19 vaccination campaigns. The rapid deployment of vaccines was an important contributor to the management of the pandemic, although vaccination rates among vulnerable groups remain quite low in some countries.
During the pandemic, many European countries also made substantial progress in vaccinating vulnerable groups against seasonal flu, with the proportion of people aged over 65 vaccinated increasing by over 10 percentage points in several countries (Figure 6). Despite some temporary challenges in 2021, most European countries were also able to maintain childhood vaccination programmes.
One of the lessons
from the pandemic is that maximising people’s health and minimising their exposure
to risk factors before a crisis is critical. Obesity and chronic conditions,
such as diabetes and respiratory problems, were important risk factors for
serious complications and death upon COVID-19 infection. The prevention of
risk factors can go a long way to improving people’s health and reducing the
prevalence of chronic diseases and deaths.
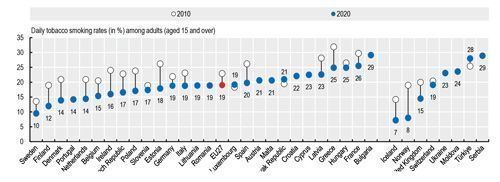
Despite progress in reducing smoking rates over the last decade, nearly one in five adults on average across EU countries still smoked daily in 2020 (Figure 7). Tobacco consumption remains the largest behavioural risk factor to health, accounting for about 780 000 deaths per year in the EU.
Alcohol consumption
has also been declining over the past decade, but harmful alcohol use remains
widespread and alcohol consumption is still responsible for nearly 300 000
deaths per year in the EU.
Conclusion
The COVID-19 pandemic is the largest shock many health systems have faced. The response of health systems to this crisis provides insights into their resilience. On the positive side, Health at a Glance: Europe 2022 highlights the rapid evolutions to new ways of safely delivering health care at the beginning of the pandemic with a doubling of the share of teleconsultations, and the rapid and widespread delivery of COVID-19 vaccinations. However, the report also highlights the extent and impact of disruptions in usual health services during the pandemic and the unmet health care needs that resulted from these disruptions, as well as the growing needs for certain types of care such as mental health services. The pandemic and the confinement measures to contain it resulted in an unprecedented worsening of population mental health, particularly among young people with evidence of a substantial increase in depression and anxiety symptoms that fluctuated during the various waves of the pandemic but generally remained higher two years into the pandemic than prior to the pandemic. European countries have implemented some measures to support young people’s mental health, but further action is needed to ensure the pandemic does not leave permanent scars on a generation of young people. European countries can use the experience gained since 2020, including the indicators shown in Health at a Glance: Europe 2022, to strengthen the recovery and resilience of their health systems. Lessons from the pandemic can help countries prepare and respond to other future shocks arising from climate change, armed conflict and anti-microbial resistance, among other risks.
Conflict of Interest
None.


















