ICU Management & Practice, Volume 18 - Issue 4, 2018
The concepts for good sedation include defining the range of sedation, the need for agents with rapid response that can be easily and rapidly varied in restless and confused patients, various modes of ventilation, continuous supervision and adequate monitoring.
The benzodiazepines era brought diazepam, lorazepam, midazolam, but they are associated with delirium, whatever the drug or dose (Ely et al. 2001; Pandharipande et al. 2007). Propofol has a better pharmacokinetic profile, but in most RCTs there was difference in time to extubation, and no difference in ICU discharge (Ely et al. 2001; Pandharipande et al. 2007). Propofol infusion syndrome limits the use of propofol as the main agent for sedation in the ICU for more than two days or at a dose of more than 4mg/kg/h (Bray 1998).
Current practice
Use boluses
Build a sedation strategy
A sedation strategy should include:
- A daily sedation stop, which can reduce duration of mechanical ventilation (Kress et al. 2000).
- Choice of drug. An RCT published in 2006 showed there were more ventilator-free days when propofol was used with daily sedation interruption (Carson et al. 2006).
- Monitoring (De Jonghe et al. 2005).
- Progress towards no sedation. An example is from Strøm et al. (2010).
Reduce sedation by titration
De Jonghe et al. (2005) developed a management protocol based on an algorithm relying on monitoring by a nurse, and a target based on a score. The nurse is in charge of the flow of the sedation agent to keep the patient in a predefined target. Cooperation between the nurse and the patient is important (Reade et al. 2016; Flükiger et al. 2018).
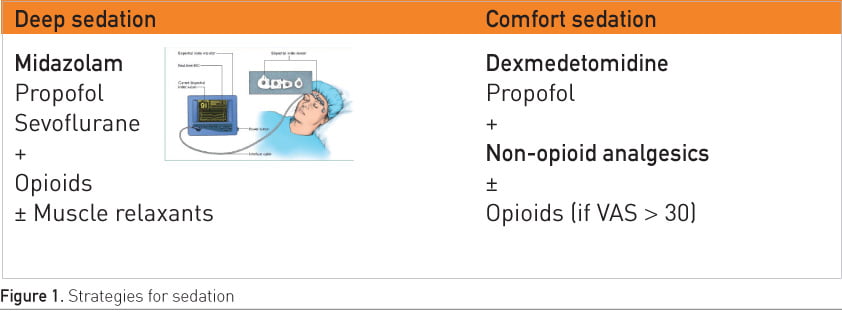
Strategies are required for deep and light/comfort sedation (Figure 1). Deep sedation is required for patients with acute respiratory distress syndrome (ARDS) and who require intracranial pressure monitoring. Deep sedation targets a RASS score of -4 or -5. For light sedation a RASS score of 0 ensures that the patient is awake, not agitated and can cooperate with the nurses. There is no middle approach.
The future of sedation
Target-controlled infusion (TCI)
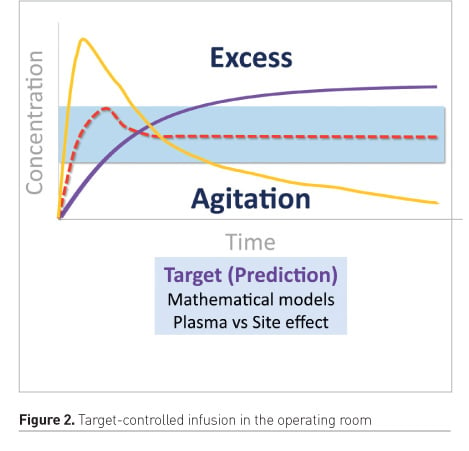
TCI rapidly loads plasmatic compartment up to the peak effect. This approach enables to reach the desired concentration effect very quickly. If continuous infusion is used, there is a long time to reach the target. Anyway, without a close titration, there is a risk of exceeding the target and of over-sedation (Figure 2).
TCI is based on predictive models (Struys et al. 2016). The target is set to also include patient features such as body mass index (BMI), gender and age. In future creatinine clearance or liver function could be included. The TCI system could have a pharmacokinetic parameter set in an infusion device and a user interface in a single smart pump. The concentration target can be set according to stimulation provided to the patient. For example, in the ICU, during nursing care, increase the target, when no nursing care is taking place, or at night, decrease the target.
There are few publications on using TCI in the ICU for sedation. Sufentanil and ketamine, compared in a RCT using a TCI system, found the model was quite predictive for sufentanil but unpredictive for ketamine and midazolam (Bourgoin et al. 2005). The study showed that the increase in sufentanil or ketamine plasma concentrations using TCI was not associated with adverse effects on cerebral haemodynamics in patients with severe brain injury. A more recent paper used a TCI propofol Marsh model system for general anaesthesia and sedation in neurosurgical patients and found a bias of -34.7% and precision of 36% (Cortegiani et al. 2018). More data for specific pharmacokinetic models are needed for TCI to be used in ICU patients.
Closed-loop systems
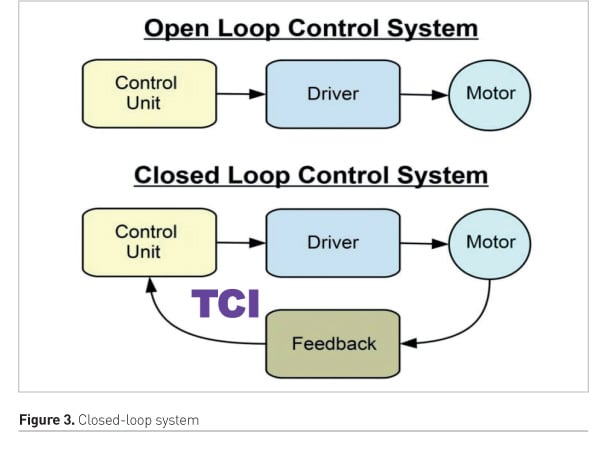
A closed-loop system requires a relevant target value (setpoint), strong monitoring that is not influenced by artefacts, a drug with a short delay and short half-life and an adaptive control algorithm with a dynamic learning strategy or fuzzy logic system (Le Guen et al. 2016). Closed-loop systems have been used in the operating room (Figure 3). A trial that compared dexmedetomidine to saline as a placebo using a bispectral index-guided closed-loop system found that dexmedetomidine significantly reduced propofol and remifentanil consumption during anaesthetic induction and reduced propofol use during maintenance of anaesthesia (Le Guen et al. 2014).
The most commonly used target for ICU patients is bispectral index, and can include respiratory rate (RR) or blood pressure (BP) if it is important that the patient was not hypotensive (Haddad et al. 2009). Alternatively drug plasma concentration can be targeted directly. A future composite index might include cerebral activity, sedation score, RR, BP and blood plasma concentration.
Use fewer opioids
Conclusion
In the past sedation patients received massive sedation. Now sedation relies on good cooperation between patients, nurses and intensivists. The future will bring target-controlled infusion in a closed-loop system, reduced use of opioids and a multimodal approach to sedation.
Key Points
- Include in the protocol a daily interruption of sedation
- Cooperation between patients, nurses and intensivists is vital in sedation
- In future, target-controlled infusions in a closed-loop system may be used in the ICU
References:
Arroliga A, Frutos-Vivar F, Hall J et al. (2005) Use of sedatives and neuromuscular blockers in a cohort of patients receiving mechanical ventilation. Chest, 128(2):496-506.
Bourgoin A, Albanèse J, Leone M et al. (2005) Effects of sufentanil or ketamine administered in target-controlled infusion on the cerebral hemodynamics of severely brain-injured patients. Crit Care Med, 33(5):1109-13.
Bray RJ (1998) Propofol infusion syndrome in children. Paediatr Anaesth, 8(6):491-9.
Carson SS, Kress JP, Rodgers JE et al. (2006) A randomized trial of intermittent lorazepam versus propofol with daily interruption in mechanically ventilated patients. Crit Care Med, 34(5):1326-32.
Cortegiani A, Pavan A, Azzeri F et al. (2018) Precision and bias of target-controlled prolonged propofol infusion for general anesthesia and sedation in neurosurgical patients. J Clin Pharmacol, 58(5):606-12.
De Jonghe B, Bastuji-Garin S, Fangio P et al. (2005) Sedation algorithm in critically ill patients without acute brain injury. Crit Care Med, 33(1):120-7.
Ely EW, Gautam S, Margolin R et al. (2001) The impact of delirium in the intensive care unit on hospital length of stay. Intensive Care Med, 27(12):1892-900.
Flükiger J, Hollinger A, Speich B et al. (2018) Dexmedetomidine in prevention and treatment of postoperative and intensive care unit delirium: a systematic review and meta-analysis. Ann Intensive Care, 8(1):92.
Haddad WM, Bailey JM (2009) Closed-loop control for intensive care unit sedation. Best Pract Res Clin Anaesthesiol, 23(1):95-114.
Kamdar NV, Hoftman N, Rahman S et al. (2017) Opioid-free analgesia in the era of enhanced recovery after surgery and the surgical home: implications for postoperative outcomes and population health. Anesth Analg, 125(4):1089-91.
Kollef MH, Levy NT, Ahrens TS et al. The use of continuous IV sedation is associated with prolongation of mechanical ventilation. Chest, 114(2):541-8.
Kress JP, Pohlman AS, O'Connor MF et al. (2000) Daily interruption of sedative infusions in critically ill patients undergoing mechanical ventilation. N Engl J Med, 342(20):1471-7.
Le Guen M, Liu N, Chazot T et al. (2016) Closed-loop anesthesia. Minerva Anestesiol, 82(5):573-81.
Le Guen M, Liu N, Tounou F et al. (2014) Dexmedetomidine reduces propofol and remifentanil requirements during bispectral index-guided closed-loop anesthesia: a double-blind, placebo-controlled trial. Anesth Analg, 118(5): 946-55.
Pandharipande PP, Pun BT, Herr DL et al. (2007) Effect of sedation with dexmedetomidine vs lorazepam on acute brain dysfunction in mechanically ventilated patients: the MENDS randomized controlled trial. JAMA, 298(22):2644-53.
Payen JF, Chanques G, Mantz J et al. (2007) Current practices in sedation and analgesia for mechanically ventilated critically ill patients: a prospective multicenter patient-based study. Anesthesiology, 106(4):687-95.
Reade MC, Eastwood GM, Bellomo R et al.; DahLIA Investigators; Australian and New Zealand Intensive Care Society Clinical Trials Group (2016) effect of dexmedetomidine added to standard care on ventilator-free time in patients with agitated delirium: a randomized clinical trial. JAMA, 315(14):1460-8. Erratum in: JAMA, 316(7):775.
Strøm T, Martinussen T, Toft P (2010) A protocol of no sedation for critically ill patients receiving mechanical ventilation: a randomised trial. Lancet, 375(9713):475-80.
Wøien H, Stubhaug A, Bjørk IT (2012) Analgesia and sedation of mechanically ventilated patients - a national survey of clinical practice. Acta Anaesthesiol Scand, 56(1):23-9.




















