University of Glasgow researchers have found that some microvascular complications of Type 2 diabetes can be predicted by an assessment of cardiac biomarkers. The results indicate that an underlying cardiac condition may precede peripheral microvascular disease processes. Peripheral microvascular events common to diabetic patients include nephropathy and retinopathy, which affect the kidneys and eyes, respectively.
The research team examined data from 439 diabetic patients who exhibited microvascular events during a median five-year clinical trial follow-up. 283 patients developed nephropathy and 183 developed retinopathy. The patients who presented microvascular complications had elevated levels of high-sensitivity troponin T (hsTnT) compared to the 2,946 patients who did not develop complications; the respective baseline levels were eight and five ng/L. Additionally, N-terminal pro-B-type natriuretic peptide (NT-proBNP) levels were higher in the microvascular patients (119 compared to 78 pg/mL).
Net Reclassification Index
Each deviation past the standard corresponded with a microvascular risk increase of 67 percent for hsTnT and 63 percent for NT-proBNP. When the researchers corrected these figures for confounding factors such as a history of cardiovascular disease and other vascular threats, the 40 percent hsTnT and 41 percent NT-proBNP microvascular risk increases remained significant.
Baseline clinical variables loaded into a prediction model were moderately successful at predicting which patients developed nephropathy or retinopathy, with the former more accurately predicted by the model. When cardiac biomarkers were added, there was a significant positively difference in the proportion of patients classified correctly. The net reclassification index was improved in categorical and continuous models alike.
Cardiac Biomarkers and Diabetic Nephropathy
Current guidelines do not include the prediction of microvascular events for diabetes patients. Naveed Sattar, the study’s lead investigator, attributes this to a lack of evidence-based therapy research, which might influence the onset of such events. This is the case despite intense interest in the development of agents that might prevent or delay the progression of diabetic nephropathy, in particular. By combining clinical predictors with cardiac biomarkers, patients at risk for microvascular events may be more readily identified for intervention to reduce their susceptibility.
The Challenge of Retinopathy
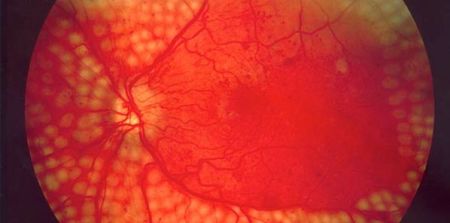
While cardiac biomarkers assisted in the classification of patients with nephropathy, the same effect was not shown for retinopathy. According to the research team, it is possible that different risk mechanisms are at play in the two microvascular events. Whereas nephropathy was better predicted by albumin-to-creatinine ratio, retinopathy’s strongest risk factors were glycated haemoglobin levels and the duration of diabetes. Retinal scanning therefore remains important in the detection of retinopathy in diabetic patients.
The research appears in the journal Diabetes Care.
Source: News Medical
Photo Credit: Google Images / Wikimedia
The research team examined data from 439 diabetic patients who exhibited microvascular events during a median five-year clinical trial follow-up. 283 patients developed nephropathy and 183 developed retinopathy. The patients who presented microvascular complications had elevated levels of high-sensitivity troponin T (hsTnT) compared to the 2,946 patients who did not develop complications; the respective baseline levels were eight and five ng/L. Additionally, N-terminal pro-B-type natriuretic peptide (NT-proBNP) levels were higher in the microvascular patients (119 compared to 78 pg/mL).
Net Reclassification Index
Each deviation past the standard corresponded with a microvascular risk increase of 67 percent for hsTnT and 63 percent for NT-proBNP. When the researchers corrected these figures for confounding factors such as a history of cardiovascular disease and other vascular threats, the 40 percent hsTnT and 41 percent NT-proBNP microvascular risk increases remained significant.
Baseline clinical variables loaded into a prediction model were moderately successful at predicting which patients developed nephropathy or retinopathy, with the former more accurately predicted by the model. When cardiac biomarkers were added, there was a significant positively difference in the proportion of patients classified correctly. The net reclassification index was improved in categorical and continuous models alike.
Cardiac Biomarkers and Diabetic Nephropathy
Current guidelines do not include the prediction of microvascular events for diabetes patients. Naveed Sattar, the study’s lead investigator, attributes this to a lack of evidence-based therapy research, which might influence the onset of such events. This is the case despite intense interest in the development of agents that might prevent or delay the progression of diabetic nephropathy, in particular. By combining clinical predictors with cardiac biomarkers, patients at risk for microvascular events may be more readily identified for intervention to reduce their susceptibility.
The Challenge of Retinopathy
While cardiac biomarkers assisted in the classification of patients with nephropathy, the same effect was not shown for retinopathy. According to the research team, it is possible that different risk mechanisms are at play in the two microvascular events. Whereas nephropathy was better predicted by albumin-to-creatinine ratio, retinopathy’s strongest risk factors were glycated haemoglobin levels and the duration of diabetes. Retinal scanning therefore remains important in the detection of retinopathy in diabetic patients.
The research appears in the journal Diabetes Care.
Source: News Medical
Photo Credit: Google Images / Wikimedia
Latest Articles
Research, Biomarkers, diabetes, type 2 diabetes, cardiac biomarkers, retinopathy, nephropathy, microvascular
University of Glasgow researchers have found that some microvascular complications of Type 2 diabetes can be predicted by an assessment of cardiac biomarke...