The biggest obstacle to healthcare safety is culture, said Mark Chassin, President and CEO The Joint Commission. Speaking today at the 8th Middle East Quality Management in Healthcare conference at Arab Health, Dr. Chassin outlined the reasons why a culture of safety is the key to sustaining high performance.
Safety culture is about enabling a culture where anyone feels comfortable to report small things that are going wrong - before they pose huge risks to patients. Trust has to permeate the organisation, said Chassin. Individuals need to know that it’s ok to report the problem, and trust that management will take the report and use effective tools to fix the problem.
High reliability organisations depend critically on safety culture. Improving safety culture is the only way to fully empower staff to find unknown risks.
Chassin advised that it is important to understand the difference between blameless errors (for learning) and blameworthy ones (for discipline, applying equally across all professional groups). High reliability organisations balance learning and accountability. The aim is not to have a blame-free culture.
High reliability organisations eliminate intimidating behaviours, assess errors and patterns uniformly, and hold everyone accountable for consistent adherence
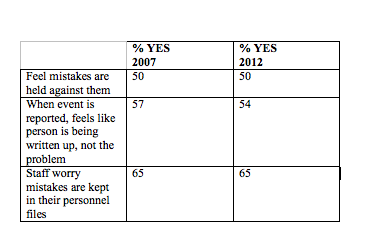
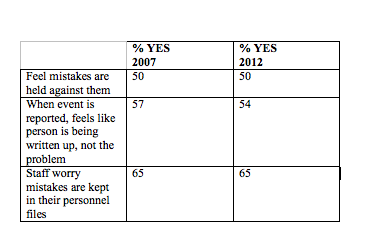
Chassin acknowledged that changing culture is difficult. He cited the U.S. Agency for Healthcare Research & Quality safety culture survey. In the five years between surveys, little changed in staff attitudes.
Merely tracking and trending measures of safety culture is not the way to improve. You need an organisation wide effort to improve, using standardise improvement methods.
Today, we mostly react to adverse events. But close calls should be viewed as “free lessons” that can lead to risk reduction - if they are recognised, reported and acted on. The ultimate goal is proactive, routine assessment of safety systems to identify and repair weaknesses - then the organisation gets closer to high reliability.
Intimidating Behaviours
Intimidating behaviour in healthcare is not uncommon, said Chassin. The most common intimidating behaviours are refusal to answer questions, or return phone calls or pages, using condescending tone or language, or impatience with questions. Chassin recommended the Joint Commission’s sentinel event alert on intimidating behaviours that talks about behaviours that undermine a culture of safety.
Such behaviour results in unsafe practices. The caregivers at the receiving end of such behaviour may assume the order is correct to avoid contact, ask colleagues to talk to the prescriber or feel pressured to act, despite safety concern. Therefore organisations need to establish a code of conduct for disrespectful behaviour.
Accountability
In deciding whether discipline should be considered in evaluating errors
there are four tests:
The substitution test asks if another person from same professional group with similar training and experience, behave the same way in similar circumstances? Were there deficiencies in training, experience or supervision? Were there mitigating circumstances? The answers plus the magnitude of risk taken by the individual lead to different levels of severity of disciplinary options. This then directs the degrees in discipline. For example, the UK published a decision tree for assessing errors and the U.S. also has a version.
Advised Chassin, the one thing you should not consider in looking at errors in judging whether it is blameworthy or blameless is the outcome to the patient. The judgement cannot be coloured by what happened in this particular patient. The odds are it would result in harm next time it happened.
A fully functional safety culture is essential to achieving high reliability in healthcare, concluded Chassin. It will take time and consistent effort on the part of all leaders and the Board. There are no guaranteed or foolproof methods. Expect setbacks and non-linear progress. Measure trust, intimidating behaviour, culture, he advised. Set goals, use Robust Process Improvement (RPI) to drive improvement. No challenge is more important or more difficult.
Safety culture is about enabling a culture where anyone feels comfortable to report small things that are going wrong - before they pose huge risks to patients. Trust has to permeate the organisation, said Chassin. Individuals need to know that it’s ok to report the problem, and trust that management will take the report and use effective tools to fix the problem.
High reliability organisations depend critically on safety culture. Improving safety culture is the only way to fully empower staff to find unknown risks.
Chassin advised that it is important to understand the difference between blameless errors (for learning) and blameworthy ones (for discipline, applying equally across all professional groups). High reliability organisations balance learning and accountability. The aim is not to have a blame-free culture.
High reliability organisations eliminate intimidating behaviours, assess errors and patterns uniformly, and hold everyone accountable for consistent adherence
Chassin acknowledged that changing culture is difficult. He cited the U.S. Agency for Healthcare Research & Quality safety culture survey. In the five years between surveys, little changed in staff attitudes.
Merely tracking and trending measures of safety culture is not the way to improve. You need an organisation wide effort to improve, using standardise improvement methods.
Today, we mostly react to adverse events. But close calls should be viewed as “free lessons” that can lead to risk reduction - if they are recognised, reported and acted on. The ultimate goal is proactive, routine assessment of safety systems to identify and repair weaknesses - then the organisation gets closer to high reliability.
Intimidating Behaviours
Intimidating behaviour in healthcare is not uncommon, said Chassin. The most common intimidating behaviours are refusal to answer questions, or return phone calls or pages, using condescending tone or language, or impatience with questions. Chassin recommended the Joint Commission’s sentinel event alert on intimidating behaviours that talks about behaviours that undermine a culture of safety.
Such behaviour results in unsafe practices. The caregivers at the receiving end of such behaviour may assume the order is correct to avoid contact, ask colleagues to talk to the prescriber or feel pressured to act, despite safety concern. Therefore organisations need to establish a code of conduct for disrespectful behaviour.
Accountability
In deciding whether discipline should be considered in evaluating errors
there are four tests:
- deliberate harm test
- incapacity test
- foresight test
- substitution test
The substitution test asks if another person from same professional group with similar training and experience, behave the same way in similar circumstances? Were there deficiencies in training, experience or supervision? Were there mitigating circumstances? The answers plus the magnitude of risk taken by the individual lead to different levels of severity of disciplinary options. This then directs the degrees in discipline. For example, the UK published a decision tree for assessing errors and the U.S. also has a version.
Advised Chassin, the one thing you should not consider in looking at errors in judging whether it is blameworthy or blameless is the outcome to the patient. The judgement cannot be coloured by what happened in this particular patient. The odds are it would result in harm next time it happened.
A fully functional safety culture is essential to achieving high reliability in healthcare, concluded Chassin. It will take time and consistent effort on the part of all leaders and the Board. There are no guaranteed or foolproof methods. Expect setbacks and non-linear progress. Measure trust, intimidating behaviour, culture, he advised. Set goals, use Robust Process Improvement (RPI) to drive improvement. No challenge is more important or more difficult.
Latest Articles
Safety, Arab Health 2015, #arabhealth, safety culture, high reliability organisations
The biggest obstacle to healthcare safety is culture, said Mark Chassin, President and CEO The Joint Commission. Speaking today at the 8th Middle East Qual...



























