Despite evidence and guidelines for appropriate imaging use in patients with low-risk prostate cancer, studies have shown only gradual reductions in inappropriate imaging use, according to an article published in Journal of the American College of Radiology.
See Also: MRI Improves Prostate Cancer Detection, Avoids Unneeded Biopsy
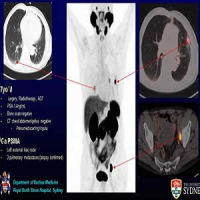
Waste contributes to healthcare cost, and the use of unnecessary and inappropriate imaging has been identified as a target for improving cost-effective care. Specifically, CT scans, nuclear medicine bone scans, and 18F-fluorodeoxyglucose (FDG) PET examinations in the setting of low-risk prostate cancer have been singled out as being wasteful.
The majority of men diagnosed with prostate cancer have serum prostate-specific antigen (PSA) elevation, leading to ultrasound-guided prostate biopsy. There are concerns that this practice results in overdiagnosis and overtreatment of low-risk and clinically insignificant. The US Preventive Services Task Force issued a statement in 2012 opposing the use of PSA as a screening test. In a previous study, investigators concluded that the use of CT in men with prostate cancer and PSA < 25 ng/mL should be considered unjustified.
Clinical Guidelines from Professional Groups
The “best practices” guidelines of the American Urological Association cover imaging in patients with low-risk prostate cancer along with serum PSA testing. The document advises that the routine use of bone scans is not required for asymptomatic men with clinically localised prostate cancer and serum PSA < 20 ng/mL. Meanwhile, the ACR Appropriateness Criteria judge bone scans and CT scans in patients with clinically established low-risk prostate cancer in the lowest category, “usually not appropriate”.
Multiple societies, including the American Society of Clinical Oncology, collaborated on the Choosing Wisely campaign, introduced by the American Board of Internal Medicine in 2012 to reduce wasteful healthcare spending. The ongoing campaign includes low-risk prostate cancer, with the American Society of Clinical Oncology recommendation that PET, CT, and bone scans not be performed in the staging of men at low risk for metastases (stages T1c-T2a, PSA < 10 ng/mL, and Gleason score < 6).
Targeted Interventions
In the JACC article, the authors describe how targeted interventions and initiatives – including the Radiology Support, Communication, and Alignment Network (R-SCAN) programme – have been effective in reducing rates of inappropriate imaging. In Sweden, for example, a national effort to educate clinicians on appropriate imaging over a 10-year period led to significantly reduced use, particularly in patients with low-risk prostate cancer (from 45% to 3%).
Similarly, a large group of urologists participating voluntarily in a quality improvement collaborative of diverse practices in Michigan pledged to follow guidelines that included appropriate imaging use in low-risk patients. Assessments that were made after the interventions show a reduction in inappropriate use of bone scans from 11.0% to 6.5% and a drop in inappropriate use of CT from 14.7% to 7.7%.
"These efforts point to the effectiveness of interventions that are modelled appropriately and could be successfully duplicated in state-based or insurance coverage-based systems, voluntary or otherwise," the authors write.
Source: Journal of the American College of Radiology
Image Credit: Nithin Rao
References:
Eberhardt, Steven C. Shah, Satyan K. (2017) R-SCAN: Appropriate Imaging for Low-Risk Prostate Cancer. Journal of the American College of Radiology; doi.org/10.1016/j.jacr.2017.01.041
Latest Articles
prostate cancer, imaging, inappropriate imaging use, low-risk patients
Despite evidence and guidelines for appropriate imaging use in patients with low-risk prostate cancer, studies have shown only gradual reductions in inappropriate imaging use, according to an article published in Journal of the American College of Radiolo