Anita Orlando, MD, Servizio di Anestesia e Rianimazione I, Fondazione IRCCS Policlinico San Matteo, Pavia, IT
Background
Asynchronies are a frequent issue in ventilated patients.1They represent a mismatch between the inspiratory and expiratory times of patient and ventilator, and thus a failure to provide ventilated patients with optimal assistance. This results in prolonged mechanical ventilation, difficult weaning, reduced patient comfort, an increased risk of diaphragmatic damage, and a potential increase in morbidity and mortality.2, 3, 4, 5, 6
Over the last few years, there has been increasing interest in asynchronies and ICU physicians have learned how to detect them by looking at the ventilator waveforms.7, 8
The aim of this paper is to describe the phenomenon of asynchrony by looking at the pathophysiology, the clinical impact and the different management possibilities, including the application of new automatic triggers implemented in modern ICU ventilators.
Classifications
There are several different classifications of patient-ventilator asynchronies, each of them considering a different aspect of the phenomenon:9, 10
Phase classification
Asynchronies can be classified as inspiratory or expiratory, depending on the respiratory phase that is affected; inspiratory asynchronies are delayed triggering, ineffective efforts and autotriggering, while expiratory asynchronies are late and early cycling, and double-triggering.
Relevance classification
Asynchronies can be classified as major or minor, depending on the type of assistance provided by the ventilator. If there is no relation at all between the patient’s request and the ventilator assistance (that is, the patient starts a breath but the ventilator does not provide any support), the asynchrony is termed major, whereas if the ventilator supports the patient in response to their request, but the assistance is not appropriate (delayed or insufficient), the asynchrony is termed minor. Mojoli et al. recently noted that minor asynchronies may have a greater impact than major ones on ventilated ICU patients.11
Etiology classification
Some asynchronies are typically associated with a patient’s low respiratory drive and/or too much ventilator assistance (ineffective efforts, delayed cycling, autotriggering, reverse triggering); others are associated with a high respiratory drive and low ventilator support, such as early cycling and double-triggering.12
Clinical relevance
The first aspect to consider is the prevalence of asynchronies; they are very common during ventilation, not only in assisted modes, but also in controlled modes. In 1997, Chao et al.13observed 200 patients during weaning from mechanical ventilation and found that 10% of them had ineffective efforts; this phenomenon was associated with prolonged and difficult weaning. This was the first large study focusing on patient-ventilator asynchronies. In the following years, there was increasing interest in the subject; other studies confirmed the high prevalence of asynchronies in ICU patients and also demonstrated their clinical impact. Asynchronies started to be considered not only as a cause of discomfort for patients14, but also as a cause of prolonged mechanical ventilation15, 6 muscle injury, higher sedation requirements,16 and eventually increased mortality.4
Clinicians applied different monitoring tools to detect asynchronies (esophageal pressure, diaphragm electrical activity), and manufacturers introduced new modes of ventilation aimed at better meeting patients’ requirements. Clinicians progressively learned how to detect asynchronies visually by looking at ventilator waveforms at the bedside and how to adapt ventilator settings accordingly breath by breath. In addition, they realized that the time required for such management was not compatible with everyday clinical practice in the ICU. In fact, patient-ventilator interaction is highly variable among different patients and may also vary in the same patient at different times.4 Moreover, it was recently suggested that brief clusters of asynchronies, that is, a greater than average frequency of asynchronies, may be associated with poor outcomes.17 However, it is not feasible to stay at the bedside 24/7 waiting for asynchronies to occur and then to change the ventilator’s settings according to the waveforms. In this context, researchers and manufacturers put their efforts into developing new technologies able to support the clinician by automatically analyzing ventilator waveforms and detecting the patients’ respiratory activity in the same way the clinician would.
Waveform analysis
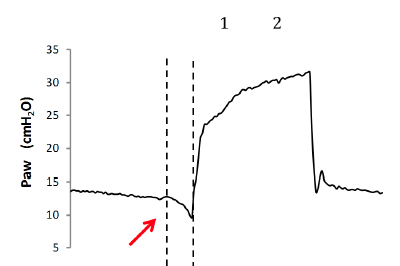
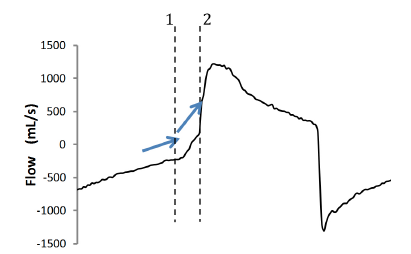
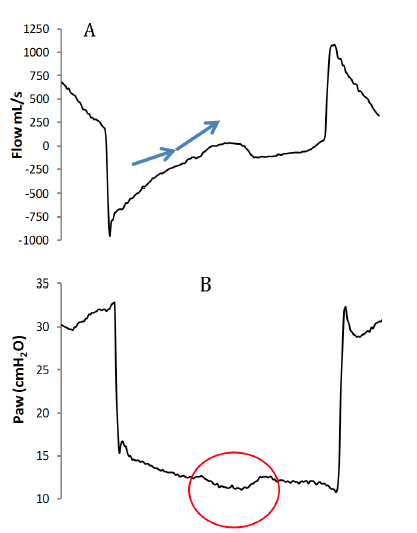
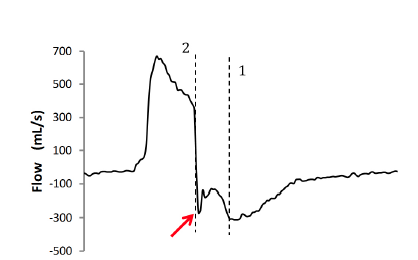
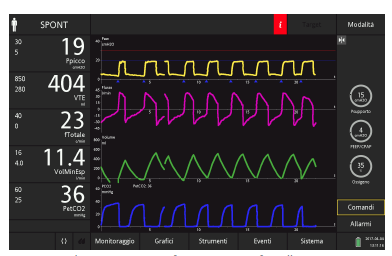
The patient’s inspiration can be detected by looking at the flow and airway-pressure waves: Typically, when a patient starts a breath, a negative deflection can be seen on the pressure curve (Fig. 1), whereas on the flow curve, a positive deflection can be detected, even if the flow is still negative (Fig. 2). Changes to flow and pressure correlate with esophageal pressure, thus they are sufficient to detect the patient’s respiratory activity in most cases13, 7, 6 With these simple rules, the patient’s inspiratory activity can be detected even when it is not detected or assisted by the ventilator. In other words, ventilator waveforms can reveal a patient’s attempt to trigger the ventilator that does not succeed, namely an ineffective effort (Fig. 3).
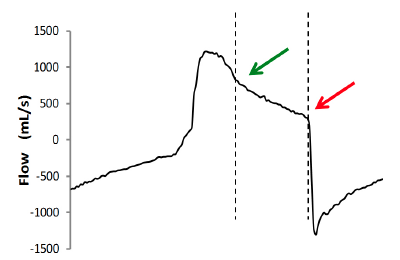
The start of the patient’s expiration can be detected on the flow and pressure waves as well. Physiologically, it corresponds to a point in time between the lowest point of the muscular pressure curve and its return to the baseline; this time point varies from patient to patient depending on the respiratory mechanics and breathing pattern, but can be conveniently approximated at half relaxation. If the muscular pressure curve is not available, indirect signs of relaxation can be detected on the flow wave and their appearance will vary depending on the assistance given by the ventilator. There are three possible cases: late cycling, early cycling and optimal cycling. In the first case, the machine supplies air for longer than required and the patient’s inspiratory muscles will relax during the ventilator’s inspiratory phase, causing a sudden change from a fast to a slow decrease in inspiratory flow as shown in Fig. 4. This often leads to hyperinflation, causing other asynchronies such as ineffective efforts and delayed triggering in the following breaths.18 This phenomenon called late cycling is typical of COPD patients and is promoted by a high level of pressure support. Sometimes, patients react to late cycling with active exhalation attempts while the ventilator’s inflation phase is continuing, causing a positive deflection of the pressure wave.
In the second case, the ventilator stops supplying air when the patient’s muscles are still contracting, so the expiratory flow is slowed by the patient’s inspiratory activity continuing after the opening of the expiratory valve. This typically affects the expiratory peak, which appears cut, delayed or “doubled” (Fig. 5). Another possible consequence of early cycling to expiration is double-triggering: Continuing patient activity after the expiratory valve has opened can activate the trigger again, causing the ventilator to deliver another breath immediately after the previous one, without a physiological exhalation in-between.
In the third case, the ventilator ends its support exactly when the patient’s muscle relaxes; the decrease in inspiratory flow becomes faster and faster, changing directly into expiratory flow with an immediate peak and then a slow exponential decrease.
Figure 1: Negative deflection of the pressure wave due to the patient’s inspiratory effort (red arrow). The two dotted lines indicate the beginning of the patient’s inspiratory effort (1) and the delayed ventilator support (inspiratory delay) (2).
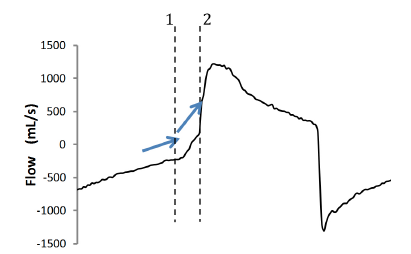
Figure 2: Blue arrows show the change in slope of the flow curve due to the patient’s inspiratory effort. The initial part of the expiration phase is characterized by a certain slope, representing the passive deflation of the lungs. When any inspiratory muscle activity starts, it produces a change in flow shape with a steeper slope towards zero flow. Note that the ventilator is able to detect the patient’s activity only if it reaches the set inspiratory trigger level (always at positive values of flow). Thus, delayed triggering will always be present if the patient’s inspiration starts at negative values of flow (for example, in the case of hyperinflation). The two dotted lines indicate the beginning of the patient’s inspiratory effort (1) and the delayed ventilator support (inspiratory delay) (2).
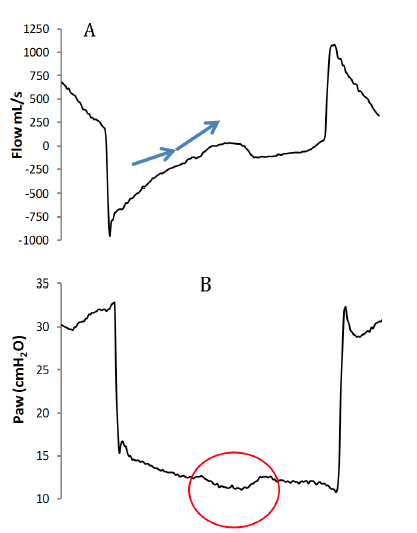
Figure 3: Patient inspiratory activity without ventilator assistance. A: A change in flow shape similar to the one previously observed in the case of delayed triggering; here no ventilator assistance follows, thus it is an ineffective effort. B: The wasted effort causes a typical depression on the pressure curve in the expiratory phase (red circle).
Figure 4: Examination of the flow wave can reveal the end of the patient’s inspiratory activity (green arrow). The rest of the inspiratory phase is passive, because the patient’s inspiratory muscles are already relaxed. The ventilator, however, continues to inflate the lungs until the expiratory valve opens (red arrow). The dotted lines indicate the expiratory delay.
Figure 5: When the ventilator ends inspiration before the patient (that is, the expiratory valve opens while the patient’s inspiratory muscles are still contracting), the first effect on the flow shape is visible on the expiratory peak. It is not as deep as expected (red arrow) and can appear to be doubled. The two dotted lines indicate the expiratory mismatch between the start of expiration by the patient (1) and ventilator (2), namely early cycling.
Optimization of ventilator settings
Once the clinician has identified the patient’s activity and asynchronies by looking at ventilator waveforms, there are a few interventions that can effectively solve the issue. Firstly, any source of external disturbance has to be eliminated (for example, circuit leaks, secretions, circuit occlusions, and disconnections), because they can lead to changes in the waveforms and thus to misinterpretation. Secondly, clinicians have to consider the effects of ventilator settings on the development of asynchrony and adjust them accordingly to promote synchronization. Examples of setting changes and their effect on patient-ventilator interaction are shown below, obtained from a simulated patient (ASL 5000 Breathing Simulator, IngMar Medical) ventilated in pressure-support modality with a
HAMILTON-G5 ventilator (Hamilton Medical AG).
Inspiratory trigger
An appropriate inspiratory trigger setting facilitates initiation of the breath and decreases the patient’s work of breathing. Flow trigger is considered better than pressure trigger because it is more sensitive to the patient’s effort and does not require negative pressure to be produced in the circuit to trigger the ventilator; a small amount of flow entering the inspiratory valve is enough. This leads to more comfortable triggering. However, pressure triggers on modern ventilators have been improved and the difference between flow and pressure triggers today is often very small.1 As a general rule, trigger sensitivity should be set at the highest value (lowest flow threshold) possible to avoid autotriggering and thus optimize the patient’s comfort.
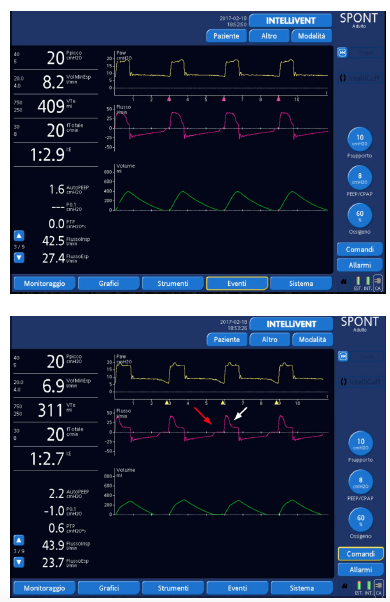
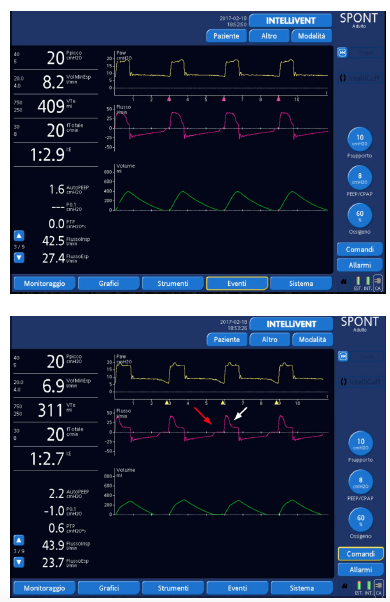
Figure 6: The same patient ventilated with inspiratory trigger: 2 l/ min, expiratory trigger sensitivity: 25%, ramp: 75ms (top) and after switching to pressure trigger: -2 cmH2O, but keeping the other settings as they were (bottom). Note the increased inspiratory delay (red arrow) and, as a consequence, late cycling to expiration (white arrow).
Pressure support level
Over-assistance may cause asynchronies as well as muscle atrophy; therefore, excessive levels of pressure support must be avoided. Too much pressure support can worsen hyperinflation, leading to difficult triggering (trigger delay and ineffective efforts) and late cycling to expiration.19 When such asynchronies are detected on ventilator waveforms, physicians should consider a decrease in the level of pressure support.
Figure 7: The same patient ventilated with inspiratory trigger: 2 l/ min, expiratory trigger sensitivity: 25%, ramp: 75 ms (top), and after an increase in pressure support from 12 to 14 cmH2O (bottom). Note the progressively increasing expiratory delay (arrows).
Ramp
The ramp represents the flow speed to reach the peak inspiratory flow. As a general rule for the same expiratory trigger sensitivity, a faster ramp results in earlier cycling, whereas a slower ramp results in later cycling. Therefore, a fast ramp can facilitate expiratory synchronization, especially in COPD patients, while a slow ramp increases the time needed to reach a lower peak inspiratory flow, thus favoring late cycling to expiration.
Figure 8: The same patient ventilated with inspiratory trigger sensitivity: 2 l/min, expiratory trigger sensitivity: 25%, ramp: 75 ms (top), and after slowing the ramp to 175 ms (bottom). Note the increased time to reach the inspiratory peak and the progressively greater expiratory delay with an ineffective effort (arrow).
Expiratory trigger sensitivity
The expiratory trigger sensitivity (ETS) is the percentage of peak inspiratory flow that controls the expiratory valve opening and the cycling to expiration. It can be manually set from minimum values of 5% to a maximum of 60%–70% of the peak flow; the default setting is usually at 25% of the peak flow.
Setting the ETS appropriately is essential for synchronization.9, 20, 21 There is not a “one fits all” configuration: Each patient needs a customized setting, based on the respiratory mechanics and the current respiratory pattern. If the ETS is too low, the ventilator will continue to inflate the patient’s lungs even after the respiratory muscles have relaxed; in other words, a certain amount of the inspiratory phase will be passive, without the patient’s muscles participating. On the contrary, if the ETS is too high, the ventilator will stop delivering air even the if respiratory muscles are still contracted; this “pliometric” or “eccentric” contraction can directly damage the diaphragm5, 22, 23 and can lead to double-triggering, breath-stacking and lung injury. An optimized ETS setting can positively affect the triggering phase as well, allowing passive, physiological exhalation, minimizing hyper-inflation and ultimately facilitating the trigger for the following breath.
Due to the fact that COPD patients are prone to late cycling, whereas a restrictive patient can experience early cycling, a reasonable approach for the initial ETS setting is 25% for patients with normal mechanics (RCexp 0.4–0.8 s), 10% for restrictive patients (RCexp < 0.4 s) and 50% for COPD patients (RCexp > 0.8 s). Thereafter, bedside interpretation of ventilator waveforms can be used to fine tune the ETS.
Figure 9: The same patient ventilated with inspiratory trigger sensitivity: 2 l/min, expiratory trigger sensitivity: 25%, ramp: 75 ms (top), immediately after changing the ETS to 10% (middle; red line), and after a few breaths with ETS at 10% (bottom). Note the prolonged inspiration with evident late cycling in the first breath after the settings have been changed (red arrow), and the effect on the triggering phase soon leading to ineffective efforts (white arrows).
Figure 10: The same patient ventilated with inspiratory trigger sensitivity: 2 l/min, expiratory trigger sensitivity: 25%, ramp: 75 ms (top), and after changing the ETS to 45% (bottom; red line). Note the correction of delayed cycling to expiration (red arrow) and the shorter inspiratory delay (white arrow), thus confirming the asynchronies’ interdependence.
Sedation
Most of the patients ventilated in assisted modes need some sedation, at least for tube tolerance,24 but excessive sedation is associated with difficult ventilator triggering and with ineffective efforts, mainly for respiratory drive and muscular pressure reduction.15 Optimizing sedation is mandatory for correct patient-ventilator interaction management: A lighter sedation plan promotes the patient’s muscle activity and reduces asynchronies, also allowing a reduction in pressure-support levels.
Continuous real-time waveform analysis
During the last ten years, considerable efforts have been made to develop software programs able to detect the patient’s respiratory activity, and to compute this data with the ventilator output to identify asynchronies. Most of this monitoring software was able to work online for brief periods only, usually from a few minutes to a few hours, and in reality the programs operated primarily as offline asynchrony analyzers, focusing mainly on major asynchronies.25, 26, 27 The only effective way to monitor patient-ventilator interaction online at the bedside remains waveform analysis performed by the expert clinician, which allows detection of asynchronies and the simultaneous optimization of ventilator settings. However, waveform analysis inevitably has certain requirements and costs. First of all, specific training is needed, as it has been shown that general clinical expertise and experience do not correlate with the ability of clinicians to detect asynchronies by waveform analysis.28, 29, 30 Moreover, performing waveform analysis at the bedside is time-consuming and requires reoptimization every time patients change their breathing pattern or their respiratory system resistance and/or compliance for any reason (for example, bronchoconstriction, hyperinflation, increased or decreased pleural effusion).
In this setting, there is a real clinical need for new technologies able to automatically analyze ventilator waveforms continuously in real time (breath by breath). The ideal software should be able to identify any respiratory activity of the patient, differentiating between the beginning and the end of each inspiratory act, and it should be able to work online as a trigger to control opening and closing of the inspiratory valve according to the patient’s effort. Recently, manufacturers have introduced several promising systems to the market, implementing them into modern ICU ventilators; this paper concentrates on one of these technologies, IntelliSync+ from Hamilton Medical.
IntelliSync+
One of the most interesting features of IntelliSync+ is how it was initially conceived: The original idea was to create a mathematical model for the clinician’s way of thinking when watching ventilator waveforms. All the possible variations in the shape and slope of ventilatory curves were implemented in a complex equation and turned into an electronic signal, which was then set up to communicate with the ventilator. Since the first prototype, many improvements have been made and IntelliSync+ is currently able to work effectively as a trigger for inspiration, expiration or both.
In 2016, we tested IntelliSync+ on a small cohort of ICU patients ventilated with PSV,31 comparing its effectiveness in optimizing the cycling-off with the ventilator’s default settings (ETS 25%) and with settings adjusted by an expert clinician at the bedside. Two different levels of pressure support were tested: the clinically set one (basal) and a 50% increase (+50).
This small study demonstrated not only the effectiveness of bedside waveform analysis and ventilator setting optimization performed by experts in improving patient-ventilator interaction, but also the need for further reoptimization once the pressure-support level has been increased. In other words, the beneficial effects of bedside optimization are not maintained throughout ventilation; rather, readjustment is required every time other settings or the clinical scenario change. However, the activation of the automatic trigger performed well in terms of synchronization and remained effective even after pressure support was increased. This means that when IntelliSync+ is active, clinicians can manage ventilation without needing to analyze waveforms again each time a setting is changed, because the software adapts to external modifications relying on the interpretation of waveforms, rather than a preset threshold.
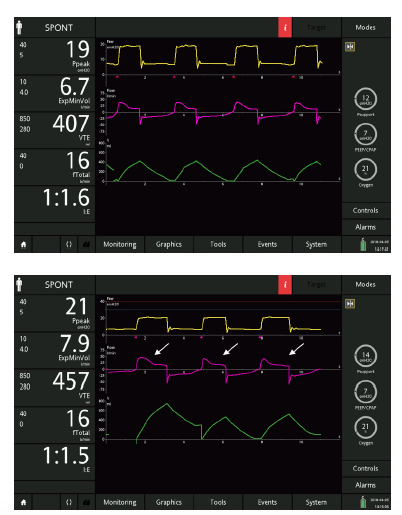
The figures below clearly demonstrate how IntelliSync+ functions, moving step by step through the study design on a simulated patient who is severely obstructed (resistance (Res) 20 cmH2O/l/s; compliance (Cpl) 90 ml/cmH2O; ASL 5000 Breathing Simulator, IngMar Medical).
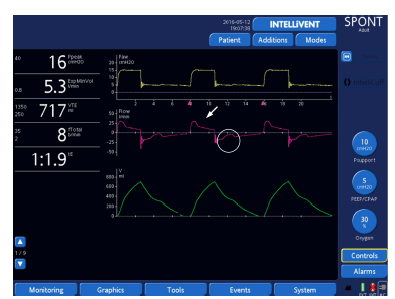
Figure 11: Default ETS setting (25% of peak inspiratory flow). Note the late cycling to expiration (arrow) and the ineffective efforts (circle).
Figure 12: Optimization (red line) of ETS performed by the clinician (ETS 50%); note the correction of late cycling and consequently the elimination of ineffective efforts.
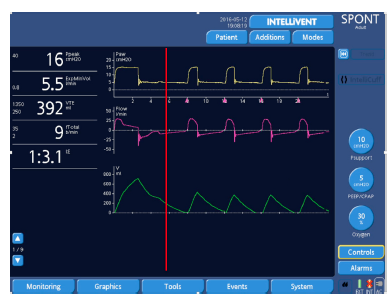
Figure 13: Next step representing an increase in the level of pressure support (from 10 cmH2O to 15 cmH2O; red line). Late cycling appears again despite the high ETS, followed by an ineffective effort (circle). At this point, reoptimization of settings would be necessary.
Figure 14: The same simulated patient with the activation of IntelliSync+ (red line) starting from the basal PS level and default ETS setting. It immediately adapts to the patient’s activity, resolving the problem of late cycling almost completely.
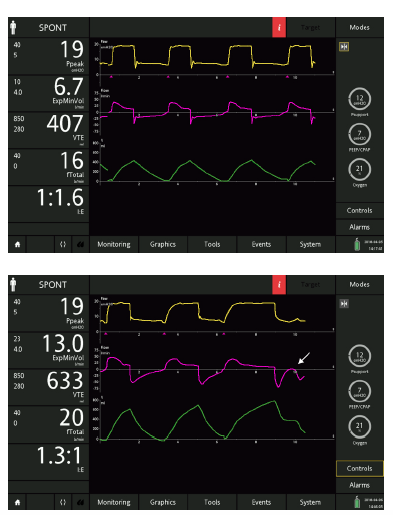
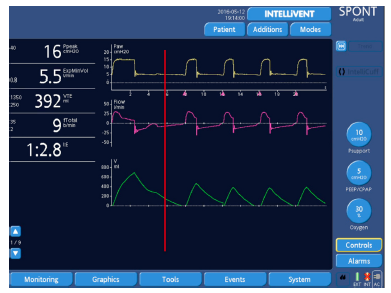
Figure 15: Even with an increase in pressure support from 10 cmH2O to 15 cmH2O, the ability to adapt to the patient’s activity remains unchanged, without the need for reoptimization of the ETS.
Another remarkable property of IntelliSync+ is demonstrated by the following example: Being able to analyze the patient’s respiratory activity continuously, it also follows the small changes in the respiratory pattern that occur breath by breath. In other words, with IntelliSync+ each breath can be different, depending on the features of each patient’s effort. This is a very interesting capability, which appears to put the technology a step ahead of human resources.
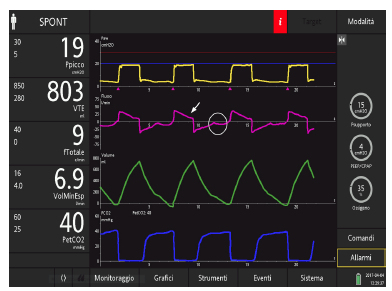
Figure 16: An ICU patient ventilated with the default ETS setting (25%) and ITS of 2 l/min with a HAMILTON-C6 ventilator (Hamilton Medical AG). Note the late cycling (arrow) and the ineffective efforts (circle).
Figure 17: The same patient after activation of IntelliSync+. Note not only the resolution of late cycling and the elimination of ineffective efforts, but also the curves’ appearance, which changes slightly from one breath to another, as happens physiologically.
Conclusion
It is beneficial for ventilated patients to be monitored and their interaction with the ventilator to be optimized, and waveform analysis has become essential to administer high-quality ventilation. Recognizing asynchronies requires good knowledge of the subject and specific training. It also takes time to perform a bedside analysis of waveforms, especially in those cases where patient-ventilator interaction is difficult. A possible solution is automation, and several interesting technologies capable of optimization have now been introduced to the market. Of these, IntelliSync+ has unique features because it is designed to reproduce the human way of thinking when approaching a ventilator waveform. It has demonstrated good performance in different ventilatory settings, maintaining its effectiveness for the duration of mechanical ventilation.
References
- Kondili E, Prinianakis G, Georgopoulos D. Patient– ventilator interaction. BJA: British Journal of Anaesthesia. 2003;91(1):106-119.
- Epstein S. How Often Does Patient-Ventilator Asynchrony Occur and What Are the Consequences?. Respiratory Care. 2011;56(1):25-38.
- Sassoon C. Triggering of the Ventilator in Patient Ventilator Interactions. Respiratory Care. 2011;56(1):39-51.
- Blanch L, Villagra A, Sales B, Montanya J, Lucangelo U, Luján M et al. Asynchronies during mechanical ventilation are associated with mortality. Intensive Care Medicine. 2015;41(4):633-641.
- Nilsestuen JO, Hargett KD. Using Ventilator Graphics to Identify Patient-Ventilator Asynchrony. Respiratory Care. 2005;50(2):202-234.
- Thille A, Rodriguez P, Cabello B, Lellouche F, Brochard L. Patient-ventilator asynchrony during assisted mechanical ventilation. Intensive Care Medicine. 2006;32(10):1515-1522.
- Georgopoulos D, Prinianakis G, Kondili E. Bedside waveforms interpretation as a tool to identify patient-ventilator asynchronies. Intensive Care Medicine. 2005;32(1):34-47.
- Mojoli F, Iotti G, Arnal J, Braschi A. Is the ventilator switching from inspiration to expiration at the right time? Look at waveforms!. Intensive Care Medicine. 2015;42(5):914-915.
- Tassaux D, Gainnier M, Battisti A, Jolliet P. Impact of Expiratory Trigger Setting on Delayed Cycling and Inspiratory Muscle Workload. American Journal of Respiratory and Critical Care Medicine. 2005;172(10):1283-1289.
- Dres M, Rittayamai N, Brochard L. Monitoring patient–ventilator asynchrony. Current Opinion in Critical Care. 2016;22(3):246-253.
- Mojoli et al. Continuous monitoring of patient-ventilator interaction in ICU patients undergoing prolonged mechanical ventilation. 27th Annual Congress of the European Society of Intensive Care Medicine, Volume: 40
- Murias G, Lucangelo U, Blanch L. Patient-ventilator asynchrony. Current Opinion in Critical Care. 2016;22(1):53-59.
- Chao D, Scheinhorn D, Stearn-Hassenpflug M. Patient-Ventilator Trigger Asynchrony in Prolonged Mechanical Ventilation. Chest. 1997;112(6):1592-1599.
- Kacmarek R, Pirrone M, Berra L. Assisted mechanical ventilation: the future is now!. BMC Anesthesiology. 2015;15(1).
- de Wit M, Pedram S, Best A, Epstein S. Observational study of patient-ventilator asynchrony and relationship to sedation level. Journal of Critical Care. 2009;24(1):74-80.
- Chanques G, Kress J, Pohlman A, Patel S, Poston J, Jaber S et al. Impact of Ventilator Adjustment and Sedation–Analgesia Practices on Severe Asynchrony in Patients Ventilated in Assist-Control Mode*. Critical Care Medicine. 2013;41(9):2177-2187.
- Vaporidi K, Babalis D, Chytas A, Lilitsis E, Kondili E, Amargianitakis V et al. Clusters of ineffective efforts during mechanical ventilation: impact on outcome. Intensive Care Medicine. 2016;43(2):184-191.
- Kacmarek RM, Villar J, Blanch L. Cycle asynchrony: always a concern during pressure ventilation! Minerva Anestesiol 2016 July;82(7):728-30.
- Thille A, Cabello B, Galia F, Lyazidi A, Brochard L. Reduction of patient-ventilator asynchrony by reducing tidal volume during pressure-support ventilation. Intensive Care Medicine. 2008;34(8):1477-1486.
- Chiumello D, Polli F, Tallarini F, Chierichetti M, Motta G, Azzari S et al. Effect of different cycling-off criteria and positive end-expiratory pressure during pressure support ventilation in patients with chronic obstructive pulmonary disease*. Critical Care Medicine. 2007;35(11):2547-2552.
- Hoff F, Tucci M, Amato M, Santos L, Victorino J. Cycling-off modes during pressure support ventilation: Effects on breathing pattern, patient effort, and comfort. Journal of Critical Care. 2014;29(3):380-385.
- Gea J, Gáldiz J, Comtois N, Zhu E, Salazkin I, Fiz J et al. Modifications of Diaphragmatic Activity Induced by Midline Laparotomy and Changes in Abdominal Wall Compliance. Archivos de Bronconeumología ((English Edition)). 2009;45(1):30-35.
- Devor S, Faulkner J. Regeneration of new fibers in muscles of old rats reduces contraction-induced injury. Journal of Applied Physiology. 1999;87(2):750-756.
- Vaschetto R, Cammarota G, Colombo D, Longhini F, Grossi F, Giovanniello A et al. Effects of Propofol on Patient-Ventilator Synchrony and Interaction During Pressure Support Ventilation and Neurally Adjusted Ventilatory Assist*. Critical Care Medicine. 2014;42(1):74-82.
- Younes M, Brochard L, Grasso S, Kun J, Mancebo J, Ranieri M et al. A method for monitoring and improving patient: ventilator interaction. Intensive Care Medicine. 2007;33(8):1337-1346.
- Blanch L, Sales B, Montanya J, Lucangelo U, Garcia Esquirol O, Villagra A et al. Validation of the Better Care® system to detect ineffective efforts during expiration in mechanically ventilated patients: a pilot study. Intensive Care Medicine. 2012;38(5):772-780.
- Sinderby C, Liu S, Colombo D, Camarotta G, Slutsky A, Navalesi P et al. An automated and standardized neural index to quantify patient-ventilator interaction. Critical Care. 2013;17(5):R239.
- Colombo D, Cammarota G, Alemani M, Carenzo L, Barra F, Vaschetto R et al. Efficacy of ventilator waveforms observation in detecting patient–ventilator asynchrony*. Critical Care Medicine. 2011;39(11):2452-2457.
- Ramirez I, Arellano D, Adasme R, Landeros J, Salinas F, Vargas A et al. Ability of ICU Health-Care Professionals to Identify Patient-Ventilator Asynchrony Using Waveform Analysis. Respiratory Care. 2016;62(2):144-149.
- Prinianakis G, Kondili E, Georgopoulos D. Effects of the flow waveform method of triggering and cycling on patient-ventilator interaction during pressure support. Intensive Care Medicine. 2003;29(11):1950-1959.
- Mojoli F et al. Cycling-off guided by real time waveform analysis (IntelliSync+): pilot study on next generation PSV. Intensive Care Medicine. 2016;4(Suppl1):A1164.