With so much digital information available about patients, could data presentation and security be improved? A session at the European Society of Intensive Care Medicine congress in Barcelona last week considered this important topic.
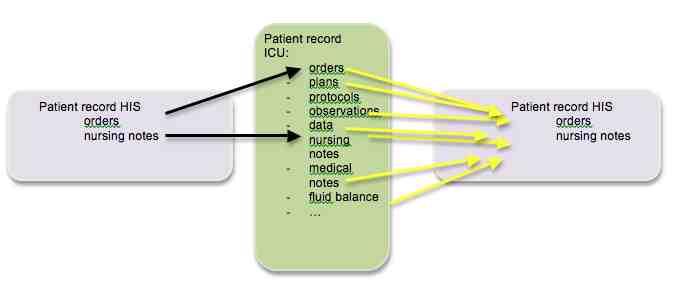 Michael Hiesmayr, from the Medical University of Vienna, noted that paperless ICUs have been around for 20 years. Information collected is both passive (coming from machines that can be integrated into a database), and active (including healthcare staff performing observations etc.). The electronic patient record makes information more global and the ICU is not an island. However, healthcare staff outside the ICU may not be used to all that information. The information needs to be condensed in order to create an understandable ‘story’ out of the patient experience during the ICU stay. Even during ICU rounds not all parts of the team have a story for or understand everything about the patient. Hiesmayr cited the VIE-VISU Metaphor Graphics to Visualize ICU Data over Time project, which was one attempt to create more quickly understandable data. Bade, Schlechtweg and Miksch in a 2004 paper experimented with representing temperatures with colours.
Michael Hiesmayr, from the Medical University of Vienna, noted that paperless ICUs have been around for 20 years. Information collected is both passive (coming from machines that can be integrated into a database), and active (including healthcare staff performing observations etc.). The electronic patient record makes information more global and the ICU is not an island. However, healthcare staff outside the ICU may not be used to all that information. The information needs to be condensed in order to create an understandable ‘story’ out of the patient experience during the ICU stay. Even during ICU rounds not all parts of the team have a story for or understand everything about the patient. Hiesmayr cited the VIE-VISU Metaphor Graphics to Visualize ICU Data over Time project, which was one attempt to create more quickly understandable data. Bade, Schlechtweg and Miksch in a 2004 paper experimented with representing temperatures with colours.
The monitor only shows the information available at one moment: - 3-5 trends on graph is already a lot. It is usually time-consuming to recombine the data and the information captured is poor for many. Text information from consultants, microbiology etc. have images, and if you want to combine the view you have to go to the Picture Archiving and Communication System (PACS). The issue is how to recognise the important information and get rid of the unimportant for the narrative.
Hiesmayr concluded that patients will never be digital - unless robots take over! However, a smart intuitive digital summary of patient course and actual status is urgently needed to create the potential for safe care.
A project to identify ICU patients using fingerprint technology was the theme for Max Jonas from Southampton, UK. The key issues for patient identity are: are you dealing with the correct patient, is data correct for that patient, is the information secure and private, and is data integrity assured vs cybersecurity medical fraud and medical identity theft. These issues are to the fore in e-health. Patients need to have trust that the organisation protects their personal data.
Jonas asserted that there was little evidence of coordinated thought or action on securing patient digital data in the healthcare system in UK. It was completely undeveloped in healthcare, despite the growth and widespread adoption of electronic health systems and available technological knowhow (for example, ability for identification is advanced in the security sector). The best healthcare can do is wristbands and passwords. Jonas observed that using wristbands for patient identification is an “accident waiting to happen”. A survey by the National Patient Safety Authority from 2003-2005 identified 236 “never” events related to wristbands.
The public is increasingly used to the idea of biometrics, e.g. using a fingerprint scanner to access bank accounts. Suitable biometric physiological identifiers include vein patterns, facial imaging, iris and retinal scanning, fingerprints and hand geometry, features formed during foetal development. The two stages in biometric identification are enrolment - biometric characteristic of the individual is initially scanned and digitised, compacted and stored in the form of the template. At the recognition stage the biometric is captured again and the template is compared against all the templates stored on the database to establish the identity of the individual.
Jonas and his colleagues trialled the use of fingerprint identity. The project included 100 patients on admission to the Surgical Day Unit and Intensive Care Unit at University Hospital Southampton. They tested the proof of concept for finger vein identification as a tool to prevent the catastrophic sequence leading to a “never” event involving the wrong patient, wrong diagnosis and wrong treatment, which relies only on loosely clipped plastic wristbands.
They used finger vein pattern imaging, which offers high security and accuracy, low to medium price, fast speed and a device which is small to medium size. The finger is placed into an infrared chamber and the venous pattern is scanned. This technology is already used for access control, banks etc., but has never been used for patient identification outside research trials. It is simple, easy to use and has a similar false positive rate to iris scanners used in airports. The project looked at the false match rate and the false non-match rates.
Interestingly, 9% of patients had no wristband at enrolment. Jonas conjectured that the 2% of patients not correctly recognised could have been due to misplacement in the reader.
In conclusion, the project did prove the concept. High performance was shown by the recognition rate, false rejection rate and the fact that there were no cases of false acceptance. Low circumvention was shown by the zero false acceptance rate, and good collectability was shown by the 100% enrolment rte and the 0% failure to acquire rate. The advantages are fast access, ability to identify unconscious patients, uniform identification, ease and convenience and potential reduction in medical errors. Disadvantages are the initial costs of the technology and data protection issues. The ability to identfy any patient and match them to the correct data, care pathway and healthcare professional should represent an absolute human right, said Jonas. However, the potential for misidentification is an ever-present risk, especially in the incapacitated or unconscious patient.
The project was presented as an e-poster at ESICM 2013.
Claire Pillar
Managing Editor, ICU Management
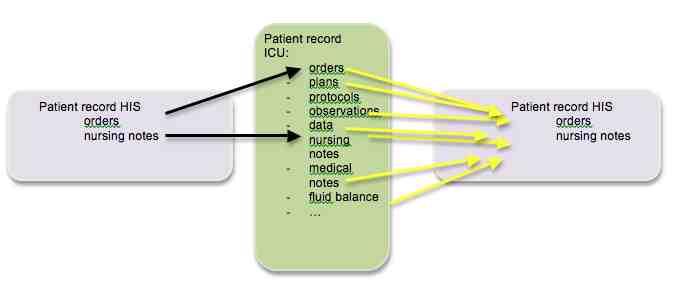 Michael Hiesmayr, from the Medical University of Vienna, noted that paperless ICUs have been around for 20 years. Information collected is both passive (coming from machines that can be integrated into a database), and active (including healthcare staff performing observations etc.). The electronic patient record makes information more global and the ICU is not an island. However, healthcare staff outside the ICU may not be used to all that information. The information needs to be condensed in order to create an understandable ‘story’ out of the patient experience during the ICU stay. Even during ICU rounds not all parts of the team have a story for or understand everything about the patient. Hiesmayr cited the VIE-VISU Metaphor Graphics to Visualize ICU Data over Time project, which was one attempt to create more quickly understandable data. Bade, Schlechtweg and Miksch in a 2004 paper experimented with representing temperatures with colours.
Michael Hiesmayr, from the Medical University of Vienna, noted that paperless ICUs have been around for 20 years. Information collected is both passive (coming from machines that can be integrated into a database), and active (including healthcare staff performing observations etc.). The electronic patient record makes information more global and the ICU is not an island. However, healthcare staff outside the ICU may not be used to all that information. The information needs to be condensed in order to create an understandable ‘story’ out of the patient experience during the ICU stay. Even during ICU rounds not all parts of the team have a story for or understand everything about the patient. Hiesmayr cited the VIE-VISU Metaphor Graphics to Visualize ICU Data over Time project, which was one attempt to create more quickly understandable data. Bade, Schlechtweg and Miksch in a 2004 paper experimented with representing temperatures with colours.The monitor only shows the information available at one moment: - 3-5 trends on graph is already a lot. It is usually time-consuming to recombine the data and the information captured is poor for many. Text information from consultants, microbiology etc. have images, and if you want to combine the view you have to go to the Picture Archiving and Communication System (PACS). The issue is how to recognise the important information and get rid of the unimportant for the narrative.
Hiesmayr concluded that patients will never be digital - unless robots take over! However, a smart intuitive digital summary of patient course and actual status is urgently needed to create the potential for safe care.
Patient Identification
A project to identify ICU patients using fingerprint technology was the theme for Max Jonas from Southampton, UK. The key issues for patient identity are: are you dealing with the correct patient, is data correct for that patient, is the information secure and private, and is data integrity assured vs cybersecurity medical fraud and medical identity theft. These issues are to the fore in e-health. Patients need to have trust that the organisation protects their personal data.
Jonas asserted that there was little evidence of coordinated thought or action on securing patient digital data in the healthcare system in UK. It was completely undeveloped in healthcare, despite the growth and widespread adoption of electronic health systems and available technological knowhow (for example, ability for identification is advanced in the security sector). The best healthcare can do is wristbands and passwords. Jonas observed that using wristbands for patient identification is an “accident waiting to happen”. A survey by the National Patient Safety Authority from 2003-2005 identified 236 “never” events related to wristbands.
The public is increasingly used to the idea of biometrics, e.g. using a fingerprint scanner to access bank accounts. Suitable biometric physiological identifiers include vein patterns, facial imaging, iris and retinal scanning, fingerprints and hand geometry, features formed during foetal development. The two stages in biometric identification are enrolment - biometric characteristic of the individual is initially scanned and digitised, compacted and stored in the form of the template. At the recognition stage the biometric is captured again and the template is compared against all the templates stored on the database to establish the identity of the individual.
Jonas and his colleagues trialled the use of fingerprint identity. The project included 100 patients on admission to the Surgical Day Unit and Intensive Care Unit at University Hospital Southampton. They tested the proof of concept for finger vein identification as a tool to prevent the catastrophic sequence leading to a “never” event involving the wrong patient, wrong diagnosis and wrong treatment, which relies only on loosely clipped plastic wristbands.
They used finger vein pattern imaging, which offers high security and accuracy, low to medium price, fast speed and a device which is small to medium size. The finger is placed into an infrared chamber and the venous pattern is scanned. This technology is already used for access control, banks etc., but has never been used for patient identification outside research trials. It is simple, easy to use and has a similar false positive rate to iris scanners used in airports. The project looked at the false match rate and the false non-match rates.
Results
- Correct recognition rate - 98%
- False acceptance rate - 0%
- False rejection rate - 2%
- Failure to acquire rate - 0%
- Enrolment rate - 100%
Interestingly, 9% of patients had no wristband at enrolment. Jonas conjectured that the 2% of patients not correctly recognised could have been due to misplacement in the reader.
In conclusion, the project did prove the concept. High performance was shown by the recognition rate, false rejection rate and the fact that there were no cases of false acceptance. Low circumvention was shown by the zero false acceptance rate, and good collectability was shown by the 100% enrolment rte and the 0% failure to acquire rate. The advantages are fast access, ability to identify unconscious patients, uniform identification, ease and convenience and potential reduction in medical errors. Disadvantages are the initial costs of the technology and data protection issues. The ability to identfy any patient and match them to the correct data, care pathway and healthcare professional should represent an absolute human right, said Jonas. However, the potential for misidentification is an ever-present risk, especially in the incapacitated or unconscious patient.
The project was presented as an e-poster at ESICM 2013.
Claire Pillar
Managing Editor, ICU Management
Latest Articles
With so much digital information available about patients, could data presentation and security be improved? A session at the European Society of Intensive...























