ICU Management & Practice, Volume 20 - Issue 4, 2020
Introduction
In recent years, the post-ICU sequelae of survivors of critical illness have become a focus of attention in research and patient care. This is the result of progress made in critical care throughout the last decades, which led to vast increases in survival rates and, therefore, growth of the cohort of post-ICU patients (Iwashyna et al. 2012; Zimmerman et al. 2013). Early investigations outlined that post-ICU patients are burdened with multifaceted consequences of critical illness summarised under the term post-intensive care syndrome (PICS). Notably, patients often perceive such functional impairments that potentially result from treatment as extremely relevant (Fried et al. 2002; Needham et al. 2012). The aim of this narrative review is to provide an overview over the established and further extended PICS domains and outpatient management of post-ICU patients.
Cognition
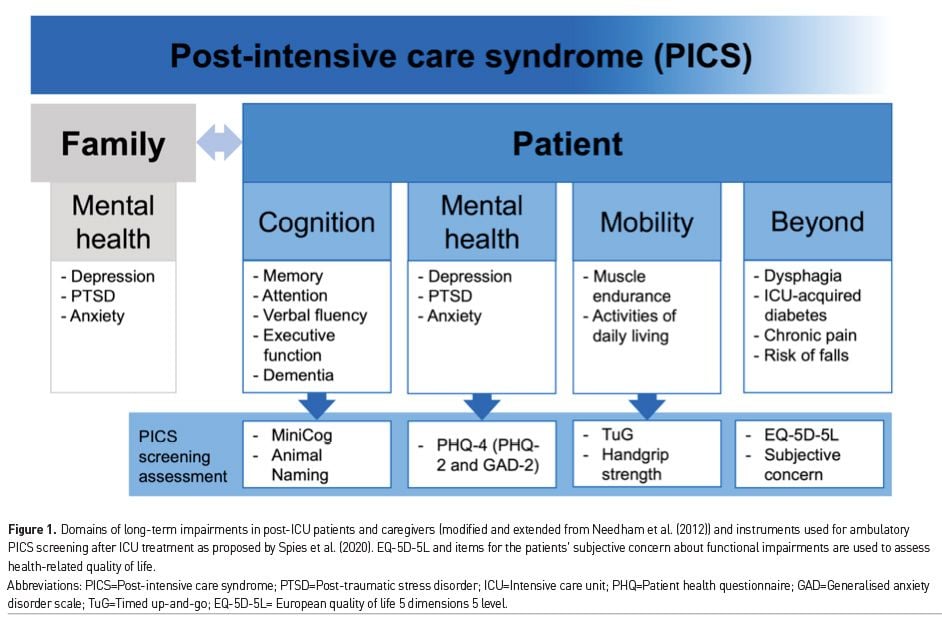
Studies in different patient populations and settings have established the association of critical illness and long-term cognitive impairments (Figure 1) (Adhikari et al. 2009; Hopkins et al. 2005; Iwashyna et al. 2010; Jackson et al. 2011; Jackson et al. 2003; Marra et al. 2018; Mitchell et al. 2018; Pandharipande et al. 2013; Wolters et al. 2013). Across studies, cognitive impairments were found in 4% to 62% of patients with follow-up periods from 2 to 156 months (Wolters et al. 2013). However, there has been no consensus on categorisation of cognitive impairments and tools of assessment, which partially explains the variations.
Upon ICU discharge, the frequency of cognitive impairments is high, and after an initial improvement (Hopkins et al. 2005), impairments persist for years. They pertain to almost all domains of cognition, including memory, verbal fluency, attention and executive function (Wolters et al. 2013). Additionally, ICU survivors face a 60% increase in relative risk to suffer from dementia three years after discharge (Guerra et al. 2015). Presence and duration of delirium is a risk factor for long-term cognitive impairment (Girard et al. 2010; Goldberg et al. 2020), but the underlying pathophysiology is widely unknown. Few studies have considered pre-ICU cognitive functions. Two population-based, prospective cohort studies found a decline in cognitive functions in ICU survivors when compared to their pre-ICU status (Ehlenbach et al. 2010; Iwashyna et al. 2010), and in a cross-sectional study, 37% of ICU patients showed pre-existing cognitive impairments (Pisani et al. 2003).
Considering the connection between delirium and cognitive impairment (Goldberg et al. 2020), preventing delirium seems rational. Regular screening for delirium (Luetz et al. 2014), implementation of bundles such as the ABCDEF bundle (Barnes-Daly et al. 2017; Marra et al. 2017), the preference for non-benzodiazepine sedatives if sedation is necessary (Pandharipande et al. 2007; Pandharipande et al. 2010), and modifications of the patient environment can reduce delirium (Litton et al. 2016; Luetz et al. 2019). Unlike a no-sedation strategy (Olsen et al. 2020; Strøm et al. 2010), no or light sedation has been shown to prevent delirium (Hager et al. 2013; Pandharipande et al. 2007). This is also the subject of current guidelines (Barr et al. 2013; Taskforce DAS et al. 2015).
As a brief screening for cognitive impairments, Spies et al. (2020) proposed to use the MiniCog (Borson et al. 2003) and Animal Naming test (Sager et al. 2006). If the patient is above threshold, the Trail Making test (Reitan 1958) and Repeatable Battery for the Assessment of Neuropsychological Status (RBANS) (Randolph 2012) provide in-depth assessment. Data on treatment of already manifest cognitive impairment is limited. Two pilot studies showed promising results of cognitive rehabilitation (Jackson et al. 2012; Wilson et al. 2018), while another study using a combined cognitive-physical rehabilitation did not detect an effect on executive functions (Brummel et al. 2012). In the future, larger trials need to investigate the potential of cognitive rehabilitation and have to consider pre-existing cognitive impairments. Studies also need to investigate if delirium prevention improves cognitive outcomes – an association still to be established.
Mental Health
Mental health impairments after critical illness pertain to depression, anxiety, and post-traumatic stress disorder (PTSD) (Marra et al. 2018). Symptoms of depression are present in about 30% of post-ICU patients, persisting even five years after discharge (Bienvenu et al. 2018; Davydow et al. 2009; Rabiee et al. 2016), but studies did not consistently use the same assessment tools, definitions and time frames (Rabiee et al. 2016). With regards to anxiety, 32% to 40% of patients show symptoms within the first year after discharge (Nikayin et al. 2016). Just like depression, anxiety symptoms remain relatively stable (Bienvenu et al. 2018; Hopkins et al. 2005). For PTSD, prevalence varied from 4% to 62% across studies, with a pooled prevalence of 17% to 44% in the year after ICU discharge (Parker et al. 2015). After eight years, PTSD prevalence was still 24% (Kapfhammer et al. 2004). Notably, a large number of patients show overlapping symptoms (Huang et al. 2016; Marra et al. 2018).
For instance, Wolters et al. (2016) found that 63% percent with any mental health symptoms showed symptoms of anxiety, depression and PTSD. Analogous to cognitive impairments, very few studies assessed pre-existing psychiatric symptoms, but results indicate that prevalence is high (Davydow et al. 2009; Rabiee et al. 2016). For instance, 6.2% of mechanically ventilated ICU patients had a psychiatric diagnosis and about 50% received a prescription for psychoactive medication in the five years preceding their ICU stay, significantly more than in the general population. ICU treatment increased the risk for a psychiatric diagnosis and psychoactive medication prescription, with hypnotics and antidepressants being most commonly prescribed (Wunsch et al. 2014).
Risk factors associated with mental health impairments are nightmares and extreme fear in the ICU (Parker et al. 2015; Rattray et al. 2005; Samuelson et al. 2007), lack of recollection of ICU experience (Rattray et al. 2005), and delusional memories from the ICU (Jones et al. 2001; Nikayin et al. 2016). Further, pre-ICU psychiatric morbidity (Wade et al. 2012; Weinert and Meller 2006), stress during ICU treatment (Wade et al. 2012), and psychiatric symptoms at hospital discharge were associated with post-ICU depression, anxiety and PTSD (Davydow et al. 2009; Nikayin et al. 2016; Rabiee et al. 2016; Rattray et al. 2005). Interestingly, neither age, severity of illness, or sex were identified as risk factors. Likewise, delirium, was not associated with PTSD or depression in the ICU context (Girard et al. 2007; Jackson et al. 2014; Wolters et al. 2016), even though post-operative delirium was found to be a risk factor for PTSD (Drews et al. 2015). It has been shown that mental health problems significantly diminished health-related quality of life (Davydow et al. 2009; Parker et al. 2015).
As a screening tool for mental health impairments, the Patient Health Questionnaire-4 was proposed, followed by the more detailed Patient Health Questionnaire-8 for depression, Generalised Anxiety Disorder Scale-7 for anxiety (Kroenke et al. 2010), and Impact of Event Scale-revised for PTSD (Spies et al. 2020; Weiss 2007). For treatment, ICU diaries reduced PTSD symptoms in one large randomised controlled trial and one prospective, non-randomised study (Garrouste-Orgeas et al. 2012; Jones et al. 2010), and anxiety and depression symptoms in another small randomised controlled trial (Knowles and Tarrier 2009), whereas a recent, large randomised controlled trial published in JAMA did not detect an effect of ICU diaries on PTSD, anxiety or depression (Garrouste-Orgeas et al. 2019). Provision of a self-help manual reduced PTSD symptoms but not depression or anxiety symptoms (Jones et al. 2003), and the benefit of post-ICU follow-ups remains inconclusive (Cuthbertson et al. 2009; Schandl et al. 2012). Interestingly, physical rehabilitation has been shown to reduce anxiety and depression (Jones et al. 2015; McWilliams et al. 2009), whereas a recent review concluded that early physical therapy does not reduce anxiety or depression (Fuke et al. 2018). Clearly, there is a demand for randomised controlled trials that rigorously compare different approaches such as self-help manuals and post-ICU follow-ups to provide evidence on strategies to reduce mental health impairments after critical illness.
Mobility and Physical Impairments
Physical impairments manifest early during the ICU stay as intensive care unit-acquired weakness (ICUAW), which is a muscular weakness defined by a Medical Research Council (MRC) score < 48 that occurs during critical illness in absence of any other plausible aetiology (Fan et al. 2014a). It has consistently been shown that muscle weakness during the ICU has a direct impact on the treatment success, like liberation from mechanical ventilation and discharge from the ICU as well as hospital (Hermans et al. 2014). Furthermore, muscle weakness at discharge from the ICU is a predictor for long-term mortality, physical function and health-related quality of life up until five years after discharge (Hermans et al. 2014; Van Aerde et al. 2020). Interestingly, Van Aerde et al. (2020) observed a dose-response relationship between muscle strength at ICU discharge and 5-year mortality. Furthermore, the optimal cut-off for predicting 5-year mortality and morbidity is a MRC score ≤ 55, which is above the diagnostic cut-off of 48 for ICUAW.
For screening of physical impairments, Spies et al. (2020) recommended to use handgrip strength (Roberts et al. 2011) and the Timed Up-and-Go (Podsiadlo and Richardson 1991), followed by the more elaborate Short Physical Performance Battery (Pavasini et al. 2016) and 2-Minute Walk Test (Brooks et al. 2006). Long-term follow up studies have shown that muscle strength measured with the MRC score fully recovers one year after ICU discharge, while muscle endurance measured via 6-minute walk test remains at 75% of predicted values (Fan et al. 2014b; Herridge et al. 2011; Wollersheim et al. 2019). This suggests that the physical impairments extend beyond muscle strength and that muscle endurance or regenerability might be a more relevant parameter during long-term evaluation. The term introduced by Van Aerde et al. (2020) “ICU-acquired neuromuscular complications” might therefore be more appropriate than the commonly used ICUAW, as weakness appears to be only one aspect of the spectrum of physical impairments. Just like cognitive and mental impairments, there is little evidence on pre-existing physical impairments, even though worse functional physical status right before hospital admission was associated with increased ICU mortality (Zampieri et al. 2017).
Current recommended management encompasses the early, goal-directed therapy of the critical illness itself in conjunction with early (within 72 hours after ICU admission) protocol-based mobilisation to improve physical function, reduce duration of a possible delirium, counteract muscle atrophy and shorten time on mechanical ventilation and in the ICU (Bein et al. 2015; Ding et al. 2019; Schaller et al. 2016; Schweickert et al. 2009; Wollersheim et al. 2019).
Other Functional Impairments
PICS was initially defined around physical function, cognition and mental health. Yet, additional post-ICU sequelae have been discovered outside the classical PICS domains. Dysphagia, for instance, is commonly observed after endotracheal intubation and has an incidence of up to 62% depending on the study cohort and length of intubation (Skoretz et al. 2010). It is an independent risk factor for 28- and 90-day mortality (Schefold et al. 2017), but Brodsky et al. (2017) were able to show that 100% of ARDS survivors discharged with dysphagia had recovered until five years after discharge.
Critical illness-associated hyperglycaemia is common and affects mortality (Plummer et al. 2014). The hyperglycaemia during acute treatment has been thoroughly investigated, while progression to a permanent dysregulation of the glucose homeostasis was neglected (NICE-SUGAR Study Investigators et al. 2009; Van den Berghe et al. 2006; Van den Berghe et al. 2001). A recent meta-analysis has shown that critical illness-associated hyperglycaemia increases the risk of developing diabetes with an odds ratio of 3.5 (Ali Abdelhamid et al. 2016). Systematic screening for ICU-acquired diabetes after discharge for early diagnosis and prevention of long-term consequences might therefore be warranted (Preiser and de Longueville 2017).
ICU patients regularly receive analgesic therapy as pain frequently occurs in critically ill patients. Interestingly, pain is also among the top three symptoms reported four months after ICU discharge, which has led to systematic investigations showing that chronic, ICU-related pain has a major impact on patients’ daily life (Baumbach et al. 2016; Choi et al. 2014).
Another organ system that has received increased attention is the skeletal system, which is affected immensely by immobilisation during and after the ICU stay (Leblanc et al. 1990). ICU survivors experience an increased bone resorption, leading to decreased bone mineral density (Orford et al. 2016). The combination with frequently observed falls in post-ICU patients cumulates to an increased risk for fractures and imposes a major detriment on recovery (Parry et al. 2020).
Family and Caregivers
The family’s role for the ICU patient is twofold, whereby family is used as a surrogate for all people the patient wishes to be included in his or her care (Brown et al. 2015). Firstly, the family is a treatment resource in a concept termed “patient-family-engagement” (PFE), which was defined by Braun et al. (2015) as “[...] an active partnership between health professionals and patients and families working at every level of the healthcare system to improve health and the quality, safety, and delivery of healthcare." Secondly, the family bears a huge burden during the ICU treatment, which can manifest in anxiety as well as depression and can lead to subsequent symptoms of PTSD (Azoulay et al. 2005; Pochard et al. 2001). Additionally, in the post-ICU care, family members regularly work as unpaid caregivers, which can cause depressive symptoms (Cameron et al. 2016). Notably, symptoms in family members are positively correlated to the degree of impairments in the post-ICU patient himself (Choi et al. 2014).
Family support interventions can reduce the ICU length of stay, most likely by facilitating the shared-decision-making process of futile interventions since no impact on mortality could be detected (Lee et al. 2019; White et al. 2018). Even though families were more satisfied with the communication with the ICU team, no benefit for their mental health was detected (Carson et al. 2016; Shelton et al. 2010; White et al. 2018). Nevertheless, the implementation of structured family support is weakly recommended in current guidelines (Davidson et al. 2017). An additional measure to include the family in the ICU treatment is a flexible or extended visitation policy, since evidence indicates towards reduced anxiety and depression in family members as well as reduced anxiety and delirium in patients (Nassar Junior et al. 2018; Rosa et al. 2019; Rosa et al. 2017). On the contrary, extended visiting hours might increase the risk of ICU staff burnout (Nassar Junior et al. 2018).
Post-ICU Care Trajectories and PICS Management
With a growing cohort of ICU survivors (Kaukonen et al. 2014; Pronovost et al. 2004), more patients require transition management from inpatient to outpatient care. Post-ICU rehabilitation should be organised to mitigate functional disabilities, enable social participation and foster return to work. These demands are hardly met, as shown in a study of 103 mechanically ventilated ICU patients followed for one year post discharge and characterisation of their care pathways and quality of life (Unroe et al. 2010). Patients experienced multiple transitions of care locations, and 67% were re-hospitalised at least once. Simultaneously, each patient accrued more than $300,000 of health care costs (Unroe et al. 2010), with re-hospitalisations being an expensive element of post-ICU care (Kress and Herridge 2012). Only 9% were independently functioning and 27% were considered having a good quality of life (Unroe et al. 2010). Several studies showed approximately 50% of previously employed survivors of critical illness were unemployed one year after discharge (Hopkins et al. 2005; Myhren et al. 2010; Norman et al. 2016), leading to a 60% loss of income (Kamdar et al. 2017). The economic consequences for the society have not been thoroughly quantified yet but are likely to be substantial. Devoid of structured post-ICU follow-up, ICU discharge has been described as “ejection” instead of smooth “transition” (Sevin and Jackson 2019).
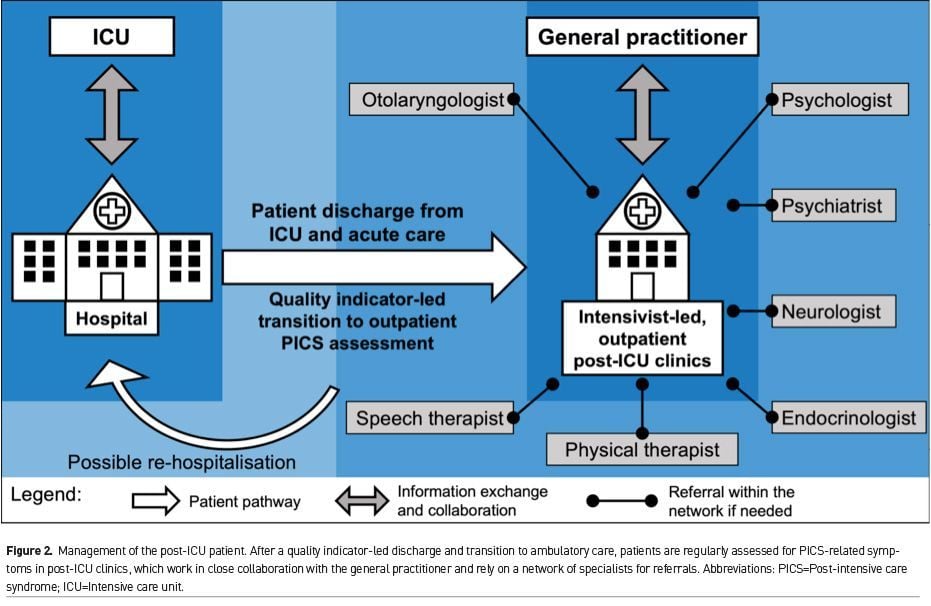
In light of complex impairments and fragmented patient trajectories, attention should be given to coordinated and evidence-based transitions from inpatient to outpatient care. Description of ideal patient pathways and implementation of intersectoral quality indicators, as defined for mechanically-ventilated patients in Germany (Kastrup et al. 2017), can help streamline the process. In more detail, these quality indicators comprise the handover to the outpatient care physician, individualised needs assessments, and transfer conferences with stakeholders from inpatient and outpatient care (i.e. transfer manager, physician, and respiratory therapist).
After transitioning to an outpatient setting, post-ICU clinics can serve as a hub to guide patients and ensure that their health concerns are addressed (Figure 2). These clinics should be staffed with intensivists, regularly assess patients for long-term impairments (Spies et al. 2020), and work in close communication with the patients’ general practitioners to exchange information. Drawing on a network of specialists such as psychotherapists and physical therapists, post-ICU clinics can develop care plans tailored to the patients’ individual needs to pave the tedious road to recovery. With continuity in post-ICU care, costly hospital re-admissions might be avoidable, PICS symptoms alleviated and return to work more likely. A similar concept was implemented at Vanderbilt ICU Recovery Center, but evaluation of effectiveness is still pending (Sevin et al. 2018). Another post-ICU programme in the UK, which included functional assessments and referrals, did not show an effect on quality of life or mental health outcomes after twelve months (Cuthbertson et al. 2009). Yet, post-ICU care was led by nurses, even though, as noted by Sevin and Jackson (2019), intensivists might be more sensitive to ICU-specific problems such as ICUAW. A Cochrane review on post-ICU follow-up services concluded that there are large variations in the design of interventions and insufficient evidence to draw conclusions at this point (Schofield-Robinson et al. 2018). Taken together, large-scale randomised-controlled trials need to rigorously assess the potential of intensivist-led, outpatient post-ICU clinics to guide patient care after critical illness.
Conclusions
Over the last two decades, functional outcomes of critical illness have gained a centre stage of intensive care research, due to the growing cohort of ICU survivors and, thus, more patients with impairments. Clinical research does not merely focus on survival, but also how the patient manages to recover in the subsequent months and years. Despite a broad consensus that a fragmented care process imposes risks on patients, evidence on effective interventions to counter impairments is scarce, and post-ICU care trajectories are an area of future improvement. In collaboration with patients’ general practitioners, post-ICU clinics might function as integrative hubs, which are embedded in a broad referral network of specialists. These institutions can harmonise inpatient-to-outpatient transitions and streamline post-ICU care processes to ensure optimal patient recovery.
Conflict of Interest
All authors declare no conflicts of interest for the submitted work. For grants, personal fees, non-financial support and patents outside the submitted work, International Committee of Medical Journal Editors (ICMJE) disclosure forms are available upon request. 
Abbreviations
ICU - Intensive care unit
PICS - Post-intensive care syndrome
RBANS - Repeatable Battery for the Assessment of Neuropsychological Status
PTSD - Post-traumatic stress disorder
ICUAW - Intensive care unit-acquired weakness
MRC - Medical Research Council
PFE - Patient-family-engagement
References:
Adhikari NKJ, McAndrews MP, Tansey CM, Matté A, Pinto R, Cheung AM et al. (2009) Self-reported symptoms of depression and memory dysfunction in survivors of ARDS, Chest, 135 (3): 678-87.
Ali Abdelhamid Y, Kar P, Finnis ME, Phillips LK, Plummer MP, Shaw JE et al. (2016) Stress hyperglycaemia in critically ill patients and the subsequent risk of diabetes: A systematic review and meta-analysis, Crit Care, 20 (1): 301.
Azoulay E, Pochard F, Kentish-Barnes N, Chevret S, Aboab J, Adrie C et al. (2005) Risk of post-traumatic stress symptoms in family members of intensive care unit patients, Am J Respir Crit Care Med, 171 (9): 987-94.
Barnes-Daly MA, Phillips G & Ely EW (2017) Improving hospital survival and reducing brain dysfunction at seven California community hospitals: Implementing PAD guidelines via the ABCDEF bundle in 6,064 patients, Crit Care Med, 45 (2): 171-8.
Barr J, Fraser GL, Puntillo K, Ely EW, Gélinas C, Dasta JF et al. (2013) Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit, Crit Care Med, 41 (1): 263-306.
Baumbach P, Gotz T, Gunther A, Weiss T, Meissner W (2016) Prevalence and characteristics of chronic intensive care-related pain: The role of severe sepsis and septic shock, Crit Care Med, 44 (6): 1129-37.
Bein T, Bischoff M, Bruckner U, Gebhardt K, Henzler D, Hermes C et al. (2015) S2e guideline: positioning and early mobilisation in prophylaxis or therapy of pulmonary disorders: Revision 2015: S2e guideline of the German Society of Anaesthesiology and Intensive Care Medicine (DGAI), Anaesthesist, 64: S1-S26.
Bienvenu OJ, Friedman LA, Colantuoni E, Dinglas VD, Sepulveda KA, Mendez-Tellez P et al. (2018) Psychiatric symptoms after acute respiratory distress syndrome: A 5-year longitudinal study, Intensive Care Med, 44 (1): 38-47.
Borson S, Scanlan JM, Chen P & Ganguli M (2003) The Mini-Cog as a screen for dementia: validation in a population-based sample, J Am Geriatr Soc, 51 (10): 1451-4.
Brodsky MB, Huang M, Shanholtz C, Mendez-Tellez PA, Palmer JB, Colantuoni E, et al. (2017) Recovery from dysphagia symptoms after oral endotracheal intubation in acute respiratory distress syndrome survivors. A 5-year longitudinal study, Ann Am Thorac Soc, 14 (3): 376-83.
Brooks D, Davis AM & Naglie G (2006) Validity of 3 physical performance measures in inpatient geriatric rehabilitation, Arch Phys Med Rehabil, 87 (1): 105-10.
Brown SM, Rozenblum R, Aboumatar H, Fagan MB, Milic M, Lee BS et al. (2015) Defining patient and family engagement in the intensive care unit, Am J Respir Crit Care Med, 191 (3): 358-60.
Brummel NE, Jackson JC, Girard TD, Pandharipande PP, Schiro E, Work B et al. (2012) A combined early cognitive and physical rehabilitation program for people who are critically ill: The activity and cognitive therapy in the intensive care unit (ACT-ICU) trial, Phys Ther, 92 (12): 1580-92.
Carson SS, Cox CE, Wallenstein S, Hanson LC, Danis M, Tulsky JA, et al. (2016) Effect of palliative
care-led meetings for families of patients with chronic critical illness: A randomized clinical trial, JAMA,
316 (1): 51-62.
Choi J, Hoffman LA, Schulz R, Tate JA, Donahoe MP, Ren D, et al. (2014) Self-reported physical symptoms in intensive care unit (ICU) survivors: Pilot exploration over four months post-ICU discharge, J Pain Symptom Manage, 47 (2): 257-70.
Cuthbertson BH, Rattray J, Campbell MK, Gager M, Roughton S, Smith A, et al. (2009) The PRaCTICaL study of nurse led, intensive care follow-up programmes for improving long term outcomes from critical illness: A pragmatic randomised controlled trial, BMJ, 339: b3723.
Davidson JE, Aslakson RA, Long AC, Puntillo KA, Kross EK, Hart J, et al. (2017) Guidelines for family-
centered care in the neonatal, pediatric, and adult ICU, Crit Care Med, 45 (1): 103-28.
Davydow DS, Gifford JM, Desai SV, Bienvenu OJ & Needham DM (2009) Depression in general intensive care unit survivors: A systematic review, Intensive Care Med, 35 (5): 796-809.
Ding N, Zhang Z, Zhang C, Yao L, Yang L, Jiang B, et al. (2019) What is the optimum time for initiation of early mobilization in mechanically ventilated patients? A network meta-analysis, PLoS One, 14 (10): e0223151.
Drews T, Franck M, Radtke FM, Weiss B, Krampe H, Brockhaus WR, et al. (2015) Postoperative delirium is an independent risk factor for posttraumatic stress disorder in the elderly patient: A prospective observational study, Eur J Anaesthesiol, 32 (3): 147-51.
Ehlenbach WJ, Hough CL, Crane PK, Haneuse SJ, Carson SS, Curtis JR, et al. (2010) Association between acute care and critical illness hospitalization and cognitive function in older adults, JAMA, 303 (8): 763-70.
Fan E, Cheek F, Chlan L, Gosselink R, Hart N, Herridge MS, et al. (2014a) An official American Thoracic
Society Clinical Practice guideline: The diagnosis of intensive care unit-acquired weakness in adults,
Am J Respir Crit Care Med, 190 (12): 1437-46.
Fan E, Dowdy DW, Colantuoni E, Mendez-Tellez PA, Sevransky JE, Shanholtz C, et al. (2014b) Physical complications in acute lung injury survivors: A two-year longitudinal prospective study, Crit Care Med, 42 (4): 849-59.
Fried TR, Bradley EH, Towle VR & Allore H (2002) Understanding the treatment preferences of
seriously ill patients, N Engl J Med, 346 (14): 1061-6.
Fuke R, Hifumi T, Kondo Y, Hatakeyama J, Takei T, Yamakawa K, et al. (2018) Early rehabilitation to prevent postintensive care syndrome in patients with critical illness: A systematic review and meta-analysis, BMJ Open, 8 (5): e019998.
Garrouste-Orgeas M, Coquet I, Périer A, Timsit JF, Pochard F, Lancrin F, et al. (2012) Impact of an intensive care unit diary on psychological distress in patients and relatives*, Crit Care Med, 40 (7): 2033-40.
Garrouste-Orgeas M, Flahault C, Vinatier I, Rigaud JP, Thieulot-Rolin N, Mercier E, et al. (2019) Effect
of an ICU diary on posttraumatic stress disorder symptoms among patients receiving mechanical
ventilation: A randomized clinical trial, JAMA, 322 (3): 229-39.
Girard TD, Jackson JC, Pandharipande PP, Pun BT, Thompson JL, Shintani AK, et al. (2010) Delirium
as a predictor of long-term cognitive impairment in survivors of critical illness, Crit Care Med, 38 (7): 1513-20.
Girard TD, Shintani AK, Jackson JC, Gordon SM, Pun BT, Henderson MS, et al. (2007) Risk factors for
post-traumatic stress disorder symptoms following critical illness requiring mechanical ventilation: A
prospective cohort study, Crit Care, 11 (1): R28.
Goldberg TE, Chen C, Wang Y, Jung E, Swanson A, Ing C, et al. (2020) Association of delirium with long-term cognitive decline: A meta-analysis, JAMA Neurol.
Guerra C, Hua M & Wunsch H (2015) Risk of a diagnosis of dementia for elderly medicare beneficiaries
after intensive care, Anesthesiology, 123 (5): 1105-12.
Hager DN, Dinglas VD, Subhas S, Rowden AM, Neufeld KJ, Bienvenu OJ, et al. (2013) Reducing deep sedation and delirium in acute lung injury patients: A quality improvement project, Crit Care Med, 41(6): 1435-42.
Hermans G, Van Mechelen H, Clerckx B, Vanhullebusch T, Mesotten D, Wilmer A, et al. (2014) Acute outcomes and 1-year mortality of intensive care unit-acquired weakness. A cohort study and propensity-matched analysis, Am J Respir Crit Care Med, 190 (4): 410-20.
Herridge MS, Tansey CM, Matte A, Tomlinson G, Diaz-Granados N, Cooper A, et al. (2011) Functional
disability 5 years after acute respiratory distress syndrome, N Engl J Med, 364 (14): 1293-304.
Hopkins RO, Weaver LK, Collingridge D, Parkinson RB, Chan KJ & Orme JF, Jr. (2005) Two-year cognitive, emotional, and quality-of-life outcomes in acute respiratory distress syndrome, Am J Respir Crit Care Med, 171 (4): 340-7.
Huang M, Parker AM, Bienvenu OJ, Dinglas VD, Colantuoni E, Hopkins RO, et al. (2016) Psychiatric symptoms in acute respiratory distress syndrome survivors: A 1-year national multicenter study, Crit Care Med, 44 (5): 954-65.
Iwashyna TJ, Cooke CR, Wunsch H & Kahn JM (2012) Population burden of long-term survivorship after severe sepsis in older Americans, J Am Geriatr Soc, 60 (6): 1070-7.
Iwashyna TJ, Ely EW, Smith DM & Langa KM (2010) Long-term cognitive impairment and functional disability among survivors of severe sepsis, JAMA, 304 (16): 1787-94.
Jackson JC, Archer KR, Bauer R, Abraham CM, Song Y, Greevey R, et al. (2011) A prospective investigation of long-term cognitive impairment and psychological distress in moderately versus severely injured trauma intensive care unit survivors without intracranial hemorrhage, J Trauma, 71 (4):
860-6.
Jackson JC, Ely EW, Morey MC, Anderson VM, Denne LB, Clune J, et al. (2012) Cognitive and physical
rehabilitation of intensive care unit survivors: Results of the RETURN randomized controlled pilot
investigation, Crit Care Med, 40 (4): 1088-97.
Jackson JC, Hart RP, Gordon SM, Shintani A, Truman B, May L, et al. (2003) Six-month neuropsychological outcome of medical intensive care unit patients, Crit Care Med, 31 (4): 1226-34.
Jackson JC, Pandharipande PP, Girard TD, Brummel NE, Thompson JL, Hughes CG, et al. (2014) Depression, post-traumatic stress disorder, and functional disability in survivors of critical illness in the BRAIN-ICU study: A longitudinal cohort study, Lancet Resp Med, 2 (5): 369-79.
Jones C, Bäckman C, Capuzzo M, Egerod I, Flaatten H, Granja C, et al. (2010) Intensive care diaries reduce new onset post traumatic stress disorder following critical illness: A randomised, controlled trial, Crit Care, 14 (5): R168.
Jones C, Eddleston J, McCairn A, Dowling S, McWilliams D, Coughlan E, et al. (2015) Improving rehabilitation after critical illness through outpatient physiotherapy classes and essential amino acid supplement: A randomized controlled trial, J Crit Care, 30 (5): 901-7.
Jones C, Griffiths RD, Humphris G & Skirrow PM (2001) Memory, delusions, and the development of
acute posttraumatic stress disorder-related symptoms after intensive care, Crit Care Med, 29 (3): 573-80.
Jones C, Skirrow PM, Griffiths RD, Humphris GH, Ingleby S, Eddleston J, et al. (2003) Rehabilitation after critical illness: A randomized, controlled trial, Crit Care Med, 31 (10): 2456-61.
Kamdar BB, Huang M, Dinglas VD, Colantuoni E, von Wachter TM, Hopkins RO, et al. (2017) Joblessness and lost earnings after acute respiratory distress syndrome in a 1-year national multicenter study, Am J Respir Crit Care Med, 196 (8): 1012-20.
Kapfhammer HP, Rothenhäusler HB, Krauseneck T, Stoll C & Schelling G (2004) Posttraumatic stress disorder and health-related quality of life in long-term survivors of acute respiratory distress syndrome, Am J Psychiatry, 161 (1): 45-52.
Kastrup M, Tittmann B, Sawatzki T, Gersch M, Vogt C, Rosenthal M, et al. (2017) Transition from in-hospital ventilation to home ventilation: Process description and quality indicators, Ger Med Sci, 15: Doc18.
Kaukonen K-M, Bailey M, Suzuki S, Pilcher D & Bellomo R (2014) Mortality related to severe sepsis and septic shock among critically ill patients in Australia and New Zealand, 2000-2012, JAMA, 311 (13): 1308-16.
Knowles RE & Tarrier N (2009) Evaluation of the effect of prospective patient diaries on emotional well-
being in intensive care unit survivors: A randomized controlled trial, Crit Care Med, 37 (1): 184-91.
Kress JP & Herridge MS (2012) Medical and economic implications of physical disability of survivorship,
Semin Respir Crit Care Med, 33 (4): 339-47.
Kroenke K, Spitzer RL, Williams JB & Loewe B (2010) The Patient Health Questionnaire somatic, anxiety, and depressive symptom scales: a systematic review, Gen Hosp Psychiatry, 32: 345-59.
Leblanc AD, Schneider VS, Evans HJ, Engelbretson DA & Krebs JM (1990) Bone mineral loss and recovery after 17 weeks of bed rest, J Bone Miner Res, 5 (8): 843-50.
Lee HW, Park Y, Jang EJ & Lee YJ (2019) Intensive care unit length of stay is reduced by protocolized family support intervention: A systematic review and meta-analysis, Intensive Care Med, 45 (8): 1072-81.
Litton E, Carnegie V, Elliott R & Webb SA (2016) The efficacy of earplugs as a sleep hygiene strategy for reducing delirium in the ICU: A systematic review and meta-analysis, Crit Care Med, 44 (5): 992-9.
Luetz A, Balzer F, Radtke FM, Jones C, Citerio G, Walder B, et al. (2014) Delirium, sedation and analgesia in the intensive care unit: a multinational, two-part survey among intensivists, PLoS One, 9 (11): e110935.
Luetz A, Grunow JJ, Mörgeli R, Rosenthal M, Weber-Carstens S, Weiss B, et al. (2019) Innovative ICU solutions to prevent and reduce delirium and Post-Intensive Care Unit Syndrome, Semin Respir Crit Care Med, 40 (5): 673-86.
Marra A, Ely EW, Pandharipande PP & Patel MB (2017) The ABCDEF bundle in critical care, Crit Care Clin, 33 (2): 225-43.
Marra A, Pandharipande PP, Girard TD, Patel MB, Hughes CG, Jackson JC, et al. (2018) Co-occurrence of post-intensive care syndrome problems among 406 survivors of critical illness, Crit Care Med, 46 (9): 1393-401.
McWilliams DJ, Atkinson D, Carter A, Foëx BA, Benington S & Conway DH (2009) Feasibility and impact of a structured, exercise-based rehabilitation programme for intensive care survivors, Physiother Theory Pract, 25 (8): 566-71.
Mitchell ML, Shum DHK, Mihala G, Murfield JE & Aitken LM (2018) Long-term cognitive impairment and delirium in intensive care: A prospective cohort study, Aust Crit Care, 31 (4): 204-11.
Myhren H, Ekeberg Ø & Stokland O (2010) Health-related quality of life and return to work after critical illness in general intensive care unit patients: A 1-year follow-up study, Crit Care Med, 38 (7): 1554-61.
Nassar Junior AP, Besen B, Robinson CC, Falavigna M, Teixeira C & Rosa RG (2018) Flexible versus restrictive visiting policies in ICUs: A systematic review and meta-analysis, Crit Care Med, 46 (7): 1175-80.
Needham DM, Davidson J, Cohen H, Hopkins RO, Weinert C, Wunsch H, et al. (2012) Improving long-term outcomes after discharge from intensive care unit: Report from a stakeholders' conference, Crit Care Med, 40 (2): 502-9.
NICE-SUGAR Study Investigators, Finfer S, Chittock DR, Su SY, Blair D, Foster D, et al. (2009) Intensive versus conventional glucose control in critically ill patients, N Engl J Med, 360 (13): 1283-97.
Nikayin S, Rabiee A, Hashem MD, Huang M, Bienvenu OJ, Turnbull AE, et al. (2016) Anxiety symptoms in survivors of critical illness: A systematic review and meta-analysis, Gen Hosp Psychiatry, 43: 23-9.
Norman BC, Jackson JC, Graves JA, Girard TD,
Pandharipande PP, Brummel NE, et al. (2016)
Employment outcomes after critical illness: An analysis of the Bringing to Light the Risk Factors and
Incidence of Neuropsychological Dysfunction in ICU Survivors cohort, Crit Care Med, 44 (11): 2003-9.
Olsen HT, Nedergaard HK, Strøm T, Oxlund J, Wian KA, Ytrebø LM, et al. (2020) Nonsedation or light sedation in critically ill, mechanically ventilated patients, N Engl J Med, 382 (12): 1103-11.
Orford NR, Lane SE, Bailey M, Pasco JA, Cattigan C, Elderkin T, et al. (2016) Changes in bone mineral density in the year after critical illness, Am J Respir Crit Care Med, 193 (7): 736-44.
Pandharipande PP, Girard TD, Jackson JC, Morandi A, Thompson JL, Pun BT, et al. (2013) Long-term
cognitive impairment after critical illness, N Engl J Med, 369 (14): 1306-16.
Pandharipande PP, Pun BT, Herr DL, Maze M, Girard TD, Miller RR, et al. (2007) Effect of sedation with dexmedetomidine vs lorazepam on acute brain dysfunction in mechanically ventilated patients: The MENDS randomized controlled trial, JAMA, 298 (22): 2644-53.
Pandharipande PP, Sanders RD, Girard TD, McGrane S, Thompson JL, Shintani AK, et al. (2010) Effect
of dexmedetomidine versus lorazepam on outcome in patients with sepsis: An a priori-designed
analysis of the MENDS randomized controlled trial, Crit Care, 14 (2): R38.
Parker AM, Sricharoenchai T, Raparla S, Schneck KW, Bienvenu OJ & Needham DM (2015) Posttraumatic stress disorder in critical illness survivors: A metaanalysis, Crit Care Med, 43 (5): 1121-9.
Parry S, Denehy L, Granger C, McGinley J, Files DC, Berry M, et al. (2020) The fear and risk of community falls in patients following an intensive care admission: An exploratory cohort study, Aust Crit Care, 33 (2): 144-50.
Pavasini R, Guralnik J, Brown JC, di Bari M, Cesari M, Landi F, et al. (2016) Short Physical Performance Battery and all-cause mortality: systematic review and meta-analysis, BMC Med, 14 (1): 215.
Pisani MA, Redlich C, McNicoll L, Ely EW & Inouye SK (2003) Underrecognition of preexisting cognitive impairment by physicians in older ICU patients, Chest, 124 (6): 2267-74.
Plummer MP, Bellomo R, Cousins CE, Annink CE, Sundararajan K, Reddi BA, et al. (2014) Dysglycaemia in the critically ill and the interaction of chronic and acute glycaemia with mortality, Intensive Care Med, 40 (7): 973-80.
Pochard F, Azoulay E, Chevret S, Lemaire F, Hubert P, Canoui P, et al. (2001) Symptoms of anxiety and depression in family members of intensive care unit patients: Ethical hypothesis regarding decision-making capacity, Crit Care Med, 29 (10): 1893-7.
Podsiadlo D & Richardson S (1991) The timed "Up & Go": a test of basic functional mobility for frail elderly persons, J Am Geriatr Soc, 39 (2): 142-8.
Preiser JC & de Longueville C (2017) Could type 2 diabetes be a component of the post-intensive care syndrome?, Crit Care, 21 (1): 26.
Pronovost PJ, Rinke ML, Emery K, Dennison C, Blackledge C & Berenholtz SM (2004) Interventions to reduce mortality among patients treated in intensive care units, J Crit Care, 19 (3): 158-64.
Rabiee A, Nikayin S, Hashem MD, Huang M, Dinglas VD, Bienvenu OJ, et al. (2016) Depressive symptoms after critical illness: A systematic review and meta-analysis, Crit Care Med, 44 (9): 1744-53.
Randolph C (2012) Repeatable Battery for the Assessment of Neuropsychological Status Update (RBANS Update), San Antonio, TX, US: The Psychological Corporation.
Rattray JE, Johnston M & Wildsmith JA (2005) Predictors of emotional outcomes of intensive care, Anaesthesia, 60 (11): 1085-92.
Reitan RM (1958) Validity of the Trail Making Test as an indicator of organic brain damage, Percept Mot Skills, 8: 271-6.
Roberts HC, Denison HJ, Martin HJ, Patel HP, Syddall H, Cooper C, et al. (2011) A review of the measurement of grip strength in clinical and epidemiological studies: towards a standardised approach, Age Ageing, 40 (4): 423-9.
Rosa RG, Falavigna M, da Silva DB, Sganzerla D, Santos MMS, Kochhann R, et al. (2019) Effect of flexible family visitation on delirium among patients in the intensive care unit: The ICU Visits randomized clinical trial, JAMA, 322 (3): 216-28.
Rosa RG, Tonietto TF, da Silva DB, Gutierres FA, Ascoli AM, Madeira LC, et al. (2017) Effectiveness and safety of an extended ICU visitation model for delirium prevention: A before and after study, Crit Care Med, 45 (10): 1660-7.
Sager MA, Hermann BP, La Rue A & Woodard JL (2006) Screening for dementia in community-based
memory clinics, Wis Med J, 105 (7): 25-9.
Samuelson KA, Lundberg D & Fridlund B (2007) Stressful memories and psychological distress in adult
mechanically ventilated intensive care patients - A 2-month follow-up study, Acta Anaesthesiol Scand, 51 (6): 671-8.
Schaller SJ, Anstey M, Blobner M, Edrich T, Grabitz SD, Gradwohl-Matis I, et al. (2016) Early, goal-directed mobilisation in the surgical intensive care unit: A randomised controlled trial, Lancet, 388 (10052): 1377-88.
Schandl A, Bottai M, Hellgren E, Sundin Ö & Sackey P (2012) Gender differences in psychological morbidity and treatment in intensive care survivors--a cohort study, Crit Care, 16 (3): R80.
Schefold JC, Berger D, Zurcher P, Lensch M, Perren A, Jakob SM, et al. (2017) Dysphagia in mechanically ventilated ICU patients (DYnAMICS): A prospective observational trial, Crit Care Med, 45 (12): 2061-9.
Schofield-Robinson OJ, Lewis SR, Smith AF, McPeake J & Alderson P (2018) Follow-up services for improving long-term outcomes in intensive care unit (ICU) survivors, Cochrane Database Syst Rev, 11 (11): Cd012701.
Schweickert WD, Pohlman MC, Pohlman AS, Nigos C, Pawlik AJ, Esbrook CL, et al. (2009) Early physical and occupational therapy in mechanically ventilated, critically ill patients: A randomised controlled trial, Lancet, 373 (9678): 1874-82.
Sevin CM, Bloom SL, Jackson JC, Wang L, Ely EW & Stollings JL (2018) Comprehensive care of ICU survivors: Development and implementation of an ICU recovery center, J Crit Care, 46: 141-8.
Sevin CM & Jackson JC (2019) Post-ICU clinics should be staffed by ICU clinicians, Crit Care Med, 47 (2): 268-72.
Shelton W, Moore CD, Socaris S, Gao J & Dowling J (2010) The effect of a family support intervention on family satisfaction, length-of-stay, and cost of care in the intensive care unit, Crit Care Med, 38 (5): 1315-20.
Skoretz SA, Flowers HL & Martino R (2010) The incidence of dysphagia following endotracheal intubation: A systematic review, Chest, 137 (3): 665-73.
Spies CD, Krampe H, Paul N, Denke C, Kiselev J, Piper SK, et al. (2020) Instruments to measure outcomes of post-intensive care syndrome in outpatient care settings – Results of an expert consensus and feasibility field test, J Intensive Care Soc.
Strøm T, Martinussen T & Toft P (2010) A protocol of no sedation for critically ill patients receiving mechanical ventilation: A randomised trial, Lancet, 375 (9713): 475-80.
Taskforce DAS, Baron R, Binder A, Biniek R, Braune S, Buerkle H, et al. (2015) S3-Leitlinie Analgesie,
Sedierung und Delirmanagement in der Intensivmedizin (DAS-Leitlinie 2015), The German Society of
Anaesthesiology and Intensive Care Medicine.
Unroe M, Kahn JM, Carson SS, Govert JA, Martinu T, Sathy SJ, et al. (2010) One-year trajectories of care and resource utilization for recipients of prolonged mechanical ventilation: A cohort study, Ann Intern Med, 153 (3): 167-75.
Van Aerde N, Meersseman P, Debaveye Y, Wilmer A, Gunst J, Casaer MP, et al. (2020) Five-year impact of ICU-acquired neuromuscular complications: A prospective, observational study, Intensive Care Med, 46 (6): 1184–93.
Van den Berghe G, Wilmer A, Hermans G, Meersseman W, Wouters PJ, Milants I, et al. (2006) Intensive insulin therapy in the medical ICU, N Engl J Med, 354 (5): 449-61.
Van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, et al. (2001) Intensive
insulin therapy in critically ill patients, N Engl J Med, 345 (19): 1359-67.
Wade DM, Howell DC, Weinman JA, Hardy RJ, Mythen MG, Brewin CR, et al. (2012) Investigating risk factors for psychological morbidity three months after intensive care: A prospective cohort study, Crit Care, 16 (5): R192.
Weinert C & Meller W (2006) Epidemiology of depression and antidepressant therapy after acute respiratory failure, Psychosomatics, 47 (5): 399-407.
Weiss DS (2007). The Impact of Event Scale: Revised. In: Wilson J & So-Kum Tang CC (eds.) International and cultural psychology. Cross-cultural assessment of psychological trauma and PTSD. New York, NY, US: Springer Science + Business Media.
White DB, Angus DC, Shields AM, Buddadhumaruk P, Pidro C, Paner C, et al. (2018) A randomized trial of a family-support intervention in intensive care units, N Engl J Med, 378 (25): 2365-75.
Wilson JE, Collar EM, Kiehl AL, Lee H, Merzenich M, Ely EW, et al. (2018) Computerized cognitive rehabilitation in intensive care unit survivors: Returning to everyday tasks using rehabilitation networks–Computerized cognitive rehabilitation pilot investigation, Ann Am Thorac Soc, 15 (7): 887-91.
Wollersheim T, Grunow JJ, Carbon NM, Haas K, Malleike J, Ramme SF, et al. (2019) Muscle wasting and function after muscle activation and early protocol-based physiotherapy: An explorative trial, J Cachexia Sarcopenia Muscle, 10 (4): 734-47.
Wolters AE, Peelen LM, Welling MC, Kok L, de Lange DW, Cremer OL, et al. (2016) Long-term mental health problems after delirium in the ICU, Crit Care Med, 44 (10): 1808-13.
Wolters AE, Slooter AJ, van der Kooi AW & van Dijk D (2013) Cognitive impairment after intensive care unit admission: A systematic review, Intensive Care Med, 39 (3): 376-86.
Wunsch H, Christiansen CF, Johansen MB, Olsen M, Ali N, Angus DC, et al. (2014) Psychiatric diagnoses and psychoactive medication use among nonsurgical critically ill patients receiving mechanical ventilation, JAMA, 311 (11): 1133-42.
Zampieri FG, Bozza FA, Moralez GM, Mazza DD, Scotti AV, Santino MS, et al. (2017) The effects of performance status one week before hospital admission on the outcomes of critically ill patients, Intensive Care Med, 43 (1): 39-47.
Zimmerman JE, Kramer AA & Knaus WA (2013) Changes in hospital mortality for United States
intensive care unit admissions from 1988 to 2012, Crit Care, 17 (2): R81.

























