ICU Management & Practice, Volume 20 - Issue 4, 2020
Is the gender gap a concern for intensive care medicine (ICM)? ICM is not gender friendly by design and this could have a major impact on the discipline given the increase in the number of female doctors. What are the main barriers to career progression for women in ICM? Members of the iWIN Foundation present their views.
Several authors and organisations have reflected on the future of Intensive and Critical Care Medicine following a significant increase, year on year, in the number of women recruited into medical schools around the world. In general, there is a concern for this phenomenon, which is leading to gender segregation with some specialties such as psychiatry becoming female dominated. Meanwhile, there is a reduction in the number of female applicants to specialties that have been traditionally male dominated such as intensive care medicine (ICM) (Lambert et al. 2003; Goldacre et al. 2005; Dacre 2008).
Data from several countries have shown that women are under-represented in the field of ICM. In Canada for example, ICM is a specialty with some of the lowest representation of women (27.7%) (Canadian Medical Association 2018). In Australia, while women are the majority of medical graduates, this has yet to translate into a significantly increased gender-balance in ICM (Modra and Yong 2019). Auspiciously, the number of women practising ICM in the United States of America (USA) has increased from 6% in 1980 to 27% in 2017 (Goldacre et al. 2005; Dacre 2008). The proportion of doctors, including ICM specialists that are women in the United Kingdom (UK) has grown every year since 2009 according to the National Healthcare System (NHS) workforce statistics by NHS Digital. The representation of women in Japanese academic medicine is not evident (Fujii et al. 2018). The trend of having an increasing number of female doctors is similar in most countries.
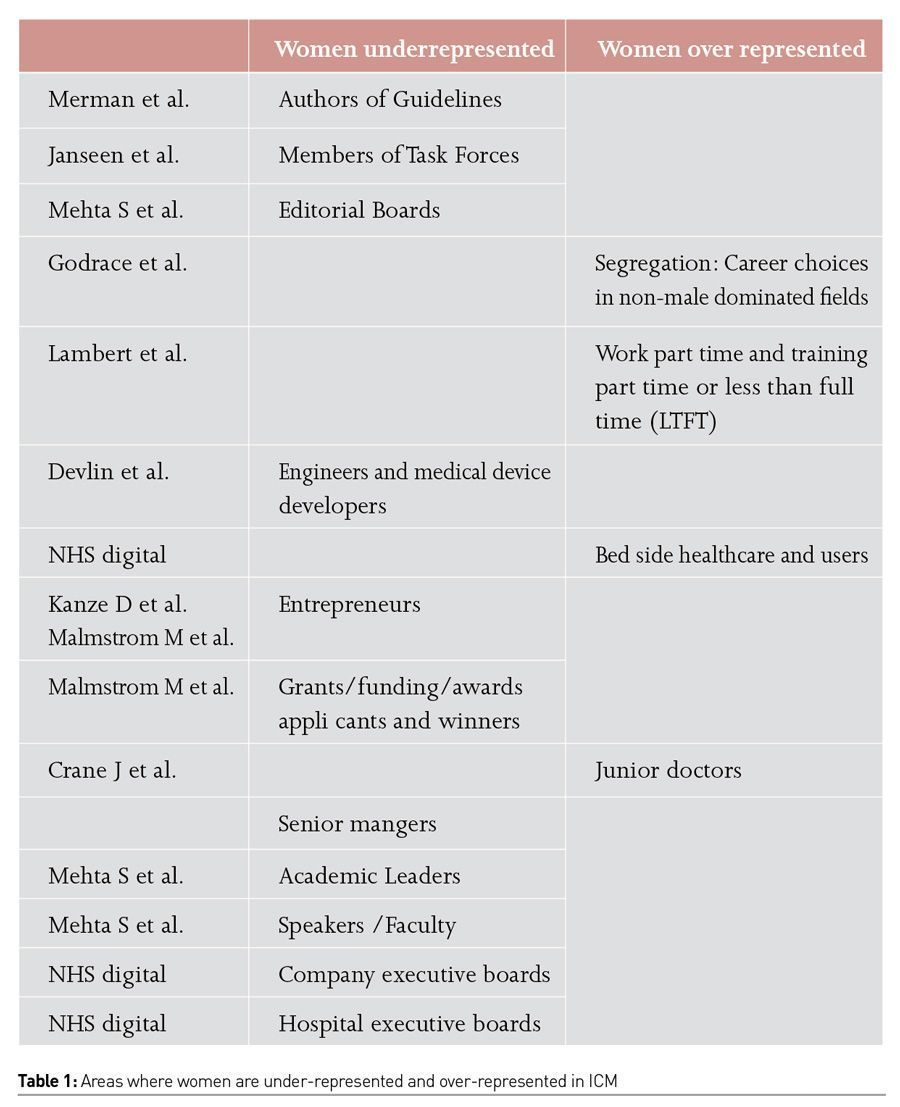
Despite this, women continue to be underrepresented in roles such as:
• Full professors in academic critical care medicine (Mehta et al. 2018; Mehta et al. 2017; Parsons et al. 2019; Metaxa 2013).
• Authors of scientific literature (Mehta et al. 2018; Metaxa 2013).
• Speakers at international conferences (Mehta et al. 2018).
• Editors in journals (Mehta et al. 2017; Parsons et al. 2019).
• Members of scientific boards (Mehta et al. 2017; Metaxa 2013).
• Entrepreneurs and CEO of start-up (Kanze et al. 2017; Malmstrom et al. 2017).
• Engineers and designers for medical devices (Kanze et al. 2017; Malmstrom et al. 2017).
• Authors of guidelines (Metaxa 2013; Merman et al. 2018).
• Members task force panels (Mehta et al. 2018; Mehta et al. 2017; Parsons et al. 2019; Janssen et al. 2019).
ICM is not “gender friendly” by design. This will have a major impact on the discipline given the increase in the number of female doctors.
Table 1 summarises the areas where women are under-represented and over-represented in ICM. Merman et al. (2018) showed that there is a significant difference in the authorship of clinical practice guidelines by gender, causing an impact on how problems are approached and solved at the bedside (Merman et al. 2018). Similarly, women are under-represented in task forces determining standards of care and this is relevant in ICM assuming that more women will be involved in the implementation of optimal clinical practice at the bed side (Janssen et al. 2019).
Women are less likely to apply for grants or awards. NHS digital has published the number of women applicants receiving new excellence awards in England and Wales between 2013 and 2016 compared to men. Female applicants were 19% in 2013 and 22% in 2016. However, every year the success rate was the same for males and females applicants.
The difference in the amount of money given to fund research and innovation led by women is not known in the field of ICM. The percentage of female principal investigators for the National Institute of Health (NIH) was 24.6% in 2003, with female investigators achieving, on average, smaller grants (Metaxa 2013). The drivers for such differences are also unknown and unmeasured (Parson et al. 2019). However, looking at women in other professions, there is an enormous gender gap recorded in Venture Capital (VC) funding and female entrepreneurs, who are receiving only about 2% of all venture funding in the USA (Kanze et al. 2017). The prevailing desire among academics, policy makers and practitioners alike has been that this gap will narrow as more women become venture capitalists. However, the number of female venture capitalists has increased from 3% in 2014 to an estimated 7% in 2017, but the funding gap has only widened (Kanze et al. 2017; Malmstrom et al. 2017). This scenario mimics reality in ICM (Parson et al. 2019). Prof Parson Leigh has tried to identify the drivers of gender inequity in ICM, but qualitative studies are currently lacking.
Researchers at Harvard have tried to look at human factors and qualitative analysis to understand the nature of this gap (Kanze et al. 2017; Malmstrom et al. 2017). They have observed, for example, the interactions between 140 prominent venture capitalists (40% of them female) and 189 entrepreneurs (12% female) that took place at TechCrunch Disrupt New York, an annual start-up funding competition (Kanze et al. 2017). Authors showed that “67% of the questions posed to male entrepreneurs were promotion-oriented, while 66% of those posed to female entrepreneurs were prevention-oriented." Malmstrom et al. (2017) recorded Venture Capitalists’ conversations and analysed how differently they talked about female entrepreneurs. VCs had stereotypical images of women instead of having qualities such as those considered important to being an entrepreneur and questioned their credibility. Conversely, when assessing male entrepreneurs, financiers leaned on stereotypical beliefs about men that reinforced their entrepreneurial potential. Male entrepreneurs were commonly described as being innovative, competent, knowledgeable and having established networks (Malmstrom et al. 2017). Shadowing the example of VCs, the overall proportion of women in ICM is steadily increasing. This has no impact on female representation among leading roles in academia and/or management (Guancial et al. 2006). Only 12% of department chairs, 17% of full professors and 11% of medical school deans in the US are female (Mehta et al. 2017). Inequality between the two genders is evident in other fields of academic medicine such as rank attainment, leadership roles and salaries (Mehta et al. 2017; Parson et al. 2019; Sidhu et al. 2009; John et al. 2012). The assumption is that stereotypes like those that have been measured in the financial world, are present in ICM (Kanze et al. 2017; Malmstrom et al. 2017; Burgess et al. 2012).
The NHS Future Forum has acknowledged the under-representation of women in senior leadership positions and the need for appropriate development opportunities (Dacre 2008). Despite women making up over three quarters of all NHS staff, in 2018, 37% of all senior roles were held by women compared with 31% in 2009, and 36% of consultants were women compared with 30% in 2009. This is less than 10% improvement in nearly a decade (Dacre 2008). Perceptions of gender composition in critical care medicine, including perceived drivers i.e. influencing factors of gender inequity, observed implications i.e. associated consequences and related strategies to encourage and retain women in the specialty, have not yet been comprehensively explained (Parson et al. 2019). Harvard researchers used sensors on employers to study how women interact at work and “no perceptible differences were observed in the behavior of men and women, yet women weren’t advancing and men were” (Gavet 2017).
ICM is a discipline where technology is increasingly represented and progressively developed. Unfortunately, there is a significant mismatch between the number of engineers developing medical devices (Kanze et al. 2017; Malmstrom et al. 2017; Devlin and Hern 2017) and the bedside users, which are mostly women (nurses and doctors) (Canadian Medical Association 2018). We cannot quantify such gap in healthcare and in particular in ICM; however, in general, women are a minority in tech companies and engineering. The Guardian recently reported the case of an engineer working at Google, who lost his job because he suggested that “male domination of Silicon Valley is down to biological differences between the sexes” (Devlin and Hern 2017). There are currently 20% of Google engineers that are women, a statistic that is matched roughly across big tech companies.
There are countless scientific studies that claim to identify differences between male and female cognitive aptitudes and in the UK, far fewer girls choose to study computer science in secondary schools (20% of the total number of students), at degree level (16%) and beyond. However, while 16% of computer science undergraduates in the UK and in the USA are female, the balance is different in India, Malaysia and Nigeria where 50% are women (Devlin and Hern 2017). Prof Dame Wendy Hall, a director of the Web Science Institute at the University of Southampton suggested that the gender gap and the “male stereotype” is dated back to the advent of the home computer in the early 80s. As a matter of fact, home computers were marketed as gaming systems for men (Devlin and Hern 2017). Jane Margolls is a psychologist at the University of California, Los Angeles, who interviewed computer science students in the 90s at Carnegie Mellon University, which had one of the top programmes in the country at the time. “Many of the women at Carnegie Mellon talked about computers being in their brother’s bedroom and there were a lot of father-son internships around the computer that were not happening with the daughters.”
The setting and structure of ICM is “gender unfriendly” by design. Authors could assume that women working at the bedside in ICM have an environment designed by male engineers. Furthermore, they have to use guidelines created by male task force members or authors. Interestingly women have no representation in leadership or academic scale to express their difficulties. This is a system that is designed to fail as soon as the number of women in medicine increases.
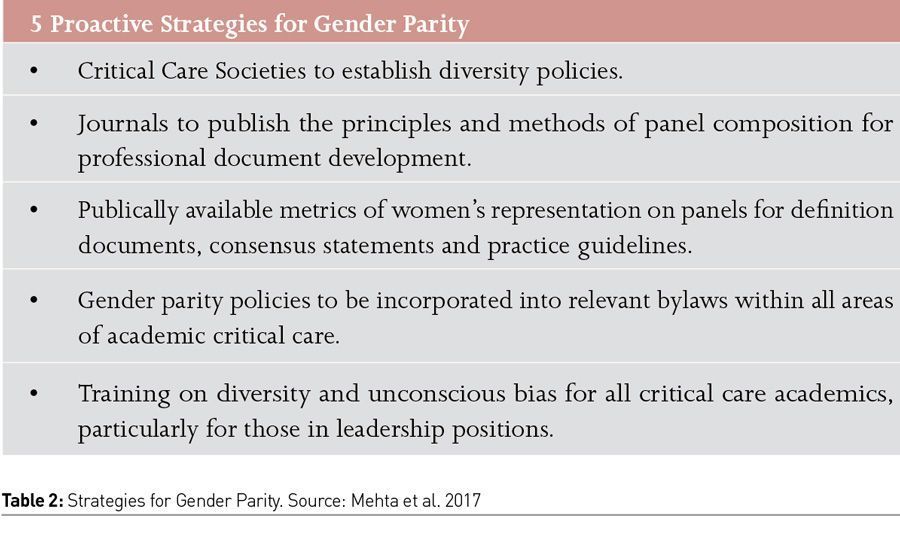
To change this culture, our critical care community must acknowledge that gender inequity exists and is problematic. Mehta et al. (2017) advocate for diversity and propose 5 proactive strategies to ensure gender parity, which we have listed in Table 2.
Barriers to Career Progression for Women in ICM
The question is: how could it be possible to address system barriers for women’s progression in the field of ICM? Table 3 contains some suggestions:
Change the myth that less than full time work/training equals being lazy or not ambitious
Frequently, trainees or specialists working outside the full-time scheme are seen as an exception to the ‘norm’ and sadly affiliate to lack of ambition and enthusiasm. The concept of part time or less than full time (LTFT) employments is crucial and relates very closely to parental responsibilities. It is evident that caring responsibilities continue to have a more substantial impact on women’s careers, despite the findings that there is little difference in male and female doctors’ personal values and their orientation towards family, children and work. Central to this issue is the need to address the bias that working or training part time or less than full time (LTFT) is a deviation from the ‘normal’ pathway.
In 2019, The College of ICM of Australia and New Zealand published that it “is committed to providing an inclusive environment that welcomes contributions from the broad diversity of the intensive care community” (cicm.org.au). This is the first formal document suggesting “The College will support accredited ICUs to offer high quality part-time training positions and part-time specialist positions“ (cicm.org.au). Nevertheless, public perception of LTFT work is unchanged, identifying individuals in this category as less productive or valued. Younger members of the British Medical Association (BMA) in the UK report that “there are often significant administrative and practical hurdles to gaining LTFT status and concerning reports of bullying and undermining behaviour from managers and colleagues” (Mehta et al. 2017). The Australian and New Zealand documents one of few examples of training institution, college or hospital, which formally addresses this issue. All Royal Colleges and specialist societies should be required to publish the proportion working LTFT in their specialty and at each grade. This would help highlight where it is currently more restricted and encourage action on identifying and removing barriers in those specialities in the future.
Moreover, according to BMA junior doctors’ surveys, “traditional career pathway of full-time, uninterrupted training to consultant or attending is not as appealing to younger generations of doctors and medical students, whether male or female. Widening access to LTFT training and working will help retain more staff, improve wellbeing and reduce burnout in women and men. Employers or trainees who take extended periods of leave, including maternity/parental leave are not guaranteed a return to the rotations that they had previously been allocated. This can have a significant impact on career progression and increase the existing gap.” Return to work or training is mostly unsupported. This has a major impact on self-confidence. People returning to work or training in a stressful environment do not feel supported in advancing their career or asking for more responsibility for several months or years. Making senior jobs more accessible and attractive to women include and moving away from the full-time default for senior posts.
Enhance transparency
Recruiting managers and academics is challenging and the interview panel is hardly trained in how to carry out these processes to minimise bias influencing decisions. Job advertisements and role descriptions should be reviewed for gendered language. There is no global regulation and frequently there is no transparency in the way those jobs are offered. There are no specific global requirements for academics to become Professors; as a matter of fact, leading roles in academia could be given without a PhD if “someone” is the right candidate. This is highlighted also in the UK gender gap enquiry by the fact that high level degrees have more value when owned by men compared to women. Transparency must be offered for:
-advertising
-recruiting
-contracting (mangers and academics)
Transparency in advertising and recruiting is likely to increase gender parity by shining a light on areas and processes that need to be improved and making individuals more aware of their rights. The UK government is currently consulting on requiring large employers to be transparent about their work-life policies and flexible work opportunities on job advertisements, which we would support.
Challenge negative behaviours
ICM organisations and societies should produce a set of recommendations on what is needed to effectively challenge behaviour and create a more positive workplace culture. Culture provides the context within which employees judge the appropriateness of their behaviour. Health and safety used to be all about policies, procedures and policing, and the focus on people was not on the agenda. Currently a safe workplace is about changing behaviour and influencing engagement. Safety is more about people, human factor and not policies. ICM specialists need to move away from the command and control mindset, and focus on daily habits, changing attitudes and recalibrating the way people think about safety. Proactive, preventative behaviour needs to be enhanced and in this context challenging negative behaviour should be part of the hospital culture. Women will benefit from this change and might find support in male colleagues. Harvard researchers showed that gender parity efforts are most effective when men believe they have a role to play, that their partnership is valued and that transformation of the workplace is something they can share in (Johnson and Smith 2018).
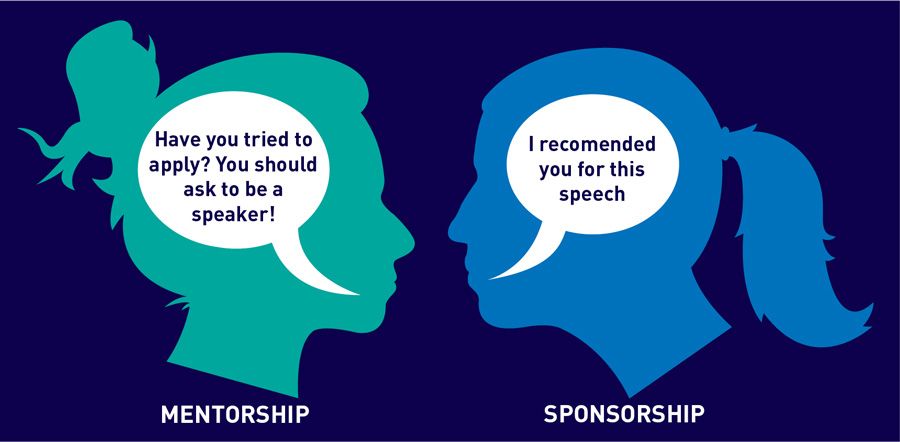
Promote sponsorship vs mentoring
Providing access to senior level sponsors and advocates could make a significant impact on successfully developing, retaining and progressing women. The General Medical Council in the UK states in its “Duties of a Doctor” guidance that doctors should be willing to take on a mentoring role for more junior doctors and healthcare professionals (gmc-uk.org/ethical-guidance/ethical-guidance-for-doctors/good-medical-practice/duties-of-a-doctor).Those specialties which currently have the widest gender pay gaps, are male dominated, and should be prioritised and additional government funding also provided to support an enhanced mentoring and sponsorship programmes.
Increase the number of grants, awards and clinical excellence awards applications done by women.
The process and application to grants and awards should be open and transparent. Women are not empowered when applying to research grants as well as excellence awards. To address the gender imbalance in submissions all possible steps should be taken to train and encourage women to apply. Success rate following application is not different for excellence awards and might increase for research grants in future.
Reduce gender pay gaps within grades and specialties. Changes to mandatory gender pay gap reporting. Reduce gender pension gap.
Laine et al. (2004) reported evidence from the US Census Bureau that “female physicians’ wages averaged 63% for each dollar earned by their male colleagues.” The College of Medicine in the US female academics earned 89% of the average male salary (Connolly and Holdcroft 2007). In April 2018, Department of Health & Social Care (DHSC) commissioned a review, chaired by Professor Dame Jane Dacre, to identify the causes of the gender pay gap in the medical sector. Data are not published, but still a significant pay gap is being recorder in the UK. Additionally, some analysis has been done on the intersection between gender and other protected characteristics such as disability, ethnicity and sexual orientation using the Oaxaca-Blinder decomposition (Elder et al. 2010).
The Gender pension gaps also needs consideration given its impact on gender long term pay inequalities. As women earn less than men on average they accrue less pension, and they are also more likely to take pension holidays to cover family costs such as childcare. Older women may also work less to provide care for others (e.g. care of adults with illnesses and disabilities) meaning they are more likely to give up work or reduce their working hours. Women working LTFT are additionally disadvantaged because pension contributions are frequently calculated on the basis of full-time equivalent earnings rather than actual earnings.
References:
Burgess DJ, Joseph A, van Ryn M, Carnes M (2012) Does stereotype threat affect women in academic medicine? Acad Med, 87:506-512.
Canadian Medical Association: Number of Physicians by Province/Territory and Specialty, Canada (2018) Available from cma.ca/sites/default/files/2019-03/2018-01-spec-prov.pdf
College of Intensive Care Medicine of Australia and New Zealand. ABN: 16 134 292 103
Connolly S, Holdcroft A (2007) The Pay Gap for Women in Medicine and Academic Medicine. An analysis of the Women in Academic Medicine (WAM) database 2007. Available from medicalwomensfederation.org.uk/images/Daonload_Pay_Gap_Report.
Dacre J (2008) Are there too many female medical graduates? No. BMJ, 336;749.
Devlin H, Hern A (2017) Why are there so few women in tech? The truth behind the google memo. The Guardian, August 8.
Elder TE, Goddeeris JH, Haider SJ (2010) Unexplained gaps and Oaxaca-Blinder decomposition. Lab economics, 1:284-290.
Fujii T, Matsuyama T, Takeuchi J et al. (2018) Women among first authors in Japanese cardiovascular journal and observational study. Int Heart Journal, 59:372-377.
Gavet G (2017) What research tells us about how women are treated at work. Harvard Business Review.
Goldacre MJ, Turner G, Fazel S, Lambert T (2005) Career choices for psychiatry: national surveys of graduates of 1974-2000 from UK medical schools. Br J Psychiatry, 186:158-64.
Guancial JR, Worobeyy CC, Henault LE et al. (2006) The gender gap in Authorship of Academic Medical Literature” A 35 years perspective. N Engl J Med, 35:281-287.
Janssen KT, Urbach HM, Ham KR, et al. (2019) The gender gap in critical care task force participation. Lancet Resp Med.
John A (2012) Is there equal pay in healthcare? Not if you are a doctor. BMJ, 345:e6191.
Johnson WB, Smith DG (2018) How Men Can Become Better Allies to Women. Harvard Business Review, October 12.
Kanze D, Huang L, Conley MA, Higgins ET (2017) Male and Female Entrepreneurs get asked different questions by Venture Capitals — and it affects how much funding they get. Harvard Business Review, 27th June.
Laine C, Turner B (2004) Unequal Pay for Equal Work: The Gender Gap in Academic Medicine. Ann Int Med, 141(3):238-240.
Lambert TW, Goldacre MJ, Turner G (2003) Career choices of United Kingdom medical graduates 1999 and 2000: questionnaire surveys. BMJ, 326:194-5.
Malmstrom M, Johansson J, Wincent J (2017) We recorded Venture Capitalists’ conversations and analyzed how differently they talk about female entrepreneurs. The Harvard Business Review, 17th May.
Mehta S, Rose L, Cook D, et al. (2018) The Speaker Gender Gap at Critical Care Conferences. CCM.
Mehta S, Burns KEA, Machado FR, et al. (2017) Gender parity in Critical Care Medicine. AJRCCM, 196(4): 425-427.
Merman E, Pincus D, Bell C, et al. (2018) Differences in clinical practice guideline authorship by gender. Lancet, 392:1626-1628.
Metaxa V (2013) Is this (still) a man’s world? Crit Care, 17:112.
Modra L, Yong S (2019) Towards gender balance in the Australian intensive care medicine workforce. Medical Journal of Australia, 211(7):300-302.
Parson LJ, Grood C, Ahmed SB, et al. (2019) Towards Gender Equity in Critical Care Medicine: A Qualitative Study of Perceived Drivers, Implications, and Strategies. CCM.
Sidhu R, Rajashekhar P, Lavin VL, Parry J, Attwood J, Holdcroft A, Sanders DS (2009) The gender imbalance in academic medicine: a study of female authorship in the United Kingdom. J R Soc Med , 102:337-342.
The duties of a doctor registered with the General Medical Council. gmc-uk.org/ethical-guidance/ethical-guidance-for-doctors/good-medical-practice/duties-of-a-doctor






















