ICU Management & Practice, Volume 16 - Issue 4, 2016
As a neurointensivist with a strong interest in nutritional support, I was delighted to trial a new integrated nutritional module. We know that nutrition really matters to our ICU patients in the context of first indicators. For example, our research group recently published a paper about two patients with viral meningoencephalitis. Invasive neuromonitoring of brain metabolism showed episodes of severe neuroglycopenia (brain glucose <0.7 mM/l) in both patients that were not attributable to decreased cerebral perfusion or hypoglycaemia. CMD-glucose levels changed depending on variations in insulin therapy, nutrition, and systemic glucose administration. The metabolic profile showed a pattern of non-ischaemic metabolic distress suggestive for mitochondrial dysfunction (Kofler et al. 2016).
Our ICU has 10 beds equipped with mechanical ventilation. At the time of the presentation, we had tested this system for 6 weeks.
IT Solution
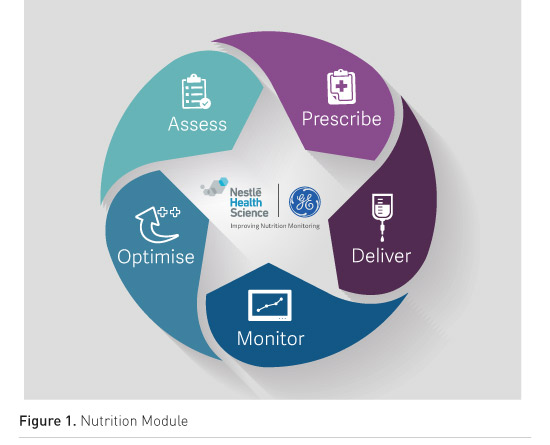
The Nutrition Module tested at Innsbruck was created by GE and Nestlé to integrate the hardware (pumps, monitor, ventilator) with the patient data management system software (Centricity). tirolkliniken University Hospital Innsbruck IT supported the installation and implementation. The module is installed on a PC and connected to the nutrition pump and to the monitor (Figure 1).
Nutritional Needs in a Single View
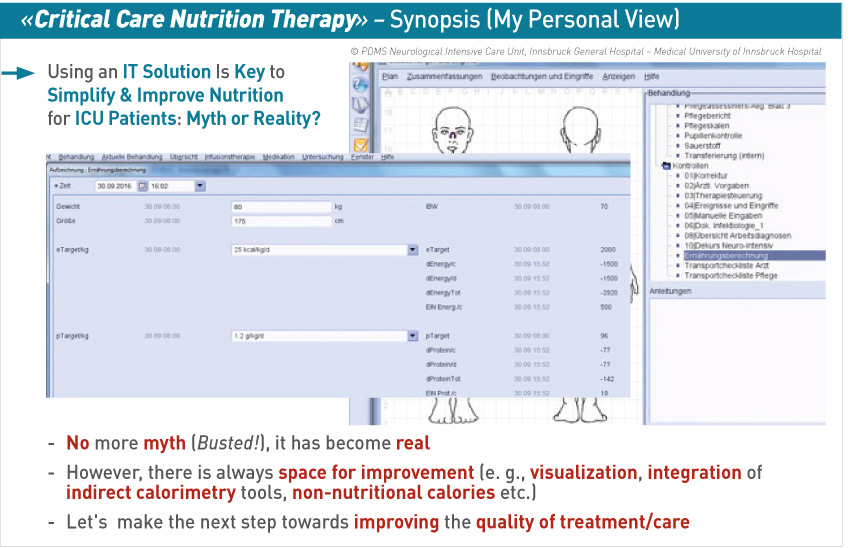
After using indirect calorimetry to assess the energy requirements of the patient, the doctor prescribes the nutrition. Using the new Nutrition Module we can also easily input body weight and check the calorie amount the patient needs. The nutrition is delivered through a pump, provided by Nestlé, and at a glance the doctor can see how much has been administered, compared to the patient’s energy needs. The system makes the calculation and shows how many calories and how much protein has been administered. This information can be displayed as a data spreadsheet and we plan to provide this also visually, to show trends. So, in one page view the doctor can see what has been delivered and what the metabolic, caloric and protein needs of the patient are, and can immediately understand and optimize the prescription to achieve those needs and see if this leads to improved patient outcomes.
With the new Nutrition Module our intention was to keep it simple. While the prescription of energy and protein relies on calculations, we are doing it now in a structured way. The module integrates six numbers and we can see the middle or late phase of the treatment period of the patient. The initial system does not have indirect calorimetry attached yet. This will improve it even more. We are also working with our pharmacists to attach other infusion pumps. There are many nutrition products available and we will liaise with our hospital pharmacy so that we can implement the key components of the nutrition formulas so these will be included in the caloric and protein calculations for macro- and micronutrients.
We use blind formulations for ongoing clinical trials on nutrition, and at the moment we cannot account for these in the system. Some medications need to be accommodated in future, for example propofol and those that use glucose as a carrier solution for other medications and contribute non-nutritional calories (Bousie et al. 2016).
Conclusion
Using the Nutrition Module will enable us to overcome variability in nutritional support, and use the data provided to plan for the future by analyzing process and outcome indicators. Using this system is much simpler than our previous method, which involved complex and time-consuming calculations, and switching between screens.
There is room for improvement in this system, including some issues with visualisation, integration of indirect calorimetry tools, non-nutritional calories etc. We have used the system for a few months only and we are working together to improve this tool to provide even better quality of patient care. However, by using an IT solution, we can combine all the different measurements, and optimize and improve the quality of treatment of the patient.
Take Home
Points
• A new tool integrates hardware and software to provide doctors with the full picture of the patient’s nutritional requirements and intake.
• A single view replaces switching between screens.
• Data is provided in a spreadsheet and will in future be provided visually, to show trends.
• Future development will integrate indirect calorimetry and infusion pumps to account for non-nutritional calories.
• We should use these tools to improve further the quality of
patient treatment and care.
References:
Bousie E, van Blokland D, Lammers HJ et al. (2016) Relevance of non-nutritional calories in mechanically ventilated critically ill patients. Eur J Clin Nutr, Sep 14. doi: 10.1038/ejcn.2016.167. [Epub ahead of print]
Kofler M, Schiefecker A, Beer R et al. (2016) Neuroglucopenia and metabolic distress in two patients with viral meningoencephalitis: a microdialysis study. Neurocrit Care, 25(2):273-81.




















