The ICU Response
Infection with the Middle East respiratory syndrome coronavirus (MERS-CoV), a recently identified virus, has led to several hundred cases of severe acute respiratory illness requiring admission to the ICU (Saad et al. 2014; Arabi et al. 2014). As of 4 December 2015, the World Health Organization (WHO) reported 1,621 laboratory-confirmed cases, including at least 584 related deaths (WHO 2015a). The majority (~80%) of cases occurred in Saudi Arabia (WHO 2015a).The disease represents several challenges to ICU management. Although many MERS-CoV cases are community-acquired (Azhar et al. 2014), the disease has great potential for healthcare-associated transmission, and has been associated with several major hospital outbreaks. These include outbreaks in Alahsa (April-May 2013) (Assiri et al. 2013), Jeddah (April and May 2014) (Oboho et al. 2015) and Riyadh (AugustSeptember 2015) (World Health Organization 2015). Most outbreaks were triggered by a community case that led to healthcareassociated transmission. Healthcare-associated transmission of MERS-CoV is thought to occur via both droplet and contact routes; in addition to being airborne during aerosol-generating procedures (van Doremalen et al. 2013).
Second, the disease has an indistinguishable presentation from other severe acute respiratory illnesses. The presenting symptoms of fever (71%), cough (68%), dyspnoea (66%) and diarrhoea (32%) (Alsolamy 2015), occurring in older adults with chronic co-morbidities (Alsolamy 2015; Al-Tawfiq et al. 2014), are all common in other forms of pneumonia. The radiologic and general laboratory manifestations also overlap substantially with other causes of pneumonia. Co-infections with other pathogens such as influenza and pneumococcus are not uncommon. Therefore physicians should keep a low threshold for testing by real-time reverse transcription polymerase chain reaction (rRT-PCR) in the appropriate context.
Third, with the infrequent occurrence of the disease, and the unfamiliarity of many staff members with the case definition of MERS-CoV infection, the diagnosis can be delayed or even missed. Delayed diagnosis without taking the proper isolation and infection control precautions leads to exposing many other patients, visitors and healthcare workers to the infection. The latest outbreak in Korea is an example where the diagnosis was delayed in an infected traveller, leading eventually to 186 MERS cases with intra- and inter-hospital transmission (Ki 2015).
Fourth, from the ICU healthcare provider standpoint, caring for these patients represents a substantial exposure risk, in terms of the ‘dose’ of viral exposure, duration of exposure per day and the total exposure duration. ICU MERS-CoV patients probably have the highest viral load among all MERS-CoV patients and therefore the ‘dose’ of exposure is probably high. ICU MERSCoV patients are very ill and often require extended time of bedside care. Many patients develop ARDS and multiorgan failure requiring organ support such as mechanical ventilation, vasopressor therapy or continuous renal replacement. Patients with severe hypoxaemia may need prone positioning and extracorporeal membrane oxygenation (ECMO), which add to the duration of bedside care. Aerosol-generating procedures, such as noninvasive ventilation, suctioning and bronchoscopy further add to the risk for healthcare-associated transmission. ICU stays can last for weeks, with prolonged viral shedding in respiratory sections, urine and stool that may persist for more than 30 days (Memish et al. 2014).
Fifth, severe infection and even death have occurred in young healthcare workers (Memish et al. 2013). The impact of such occurrences on the ICU workforce can be devastating.
In this article, we discuss key issues related to ICU preparedness for managing a MERSCoV outbreak.
ICU Preparedness for MERS-CoV
Early identification and diagnosis
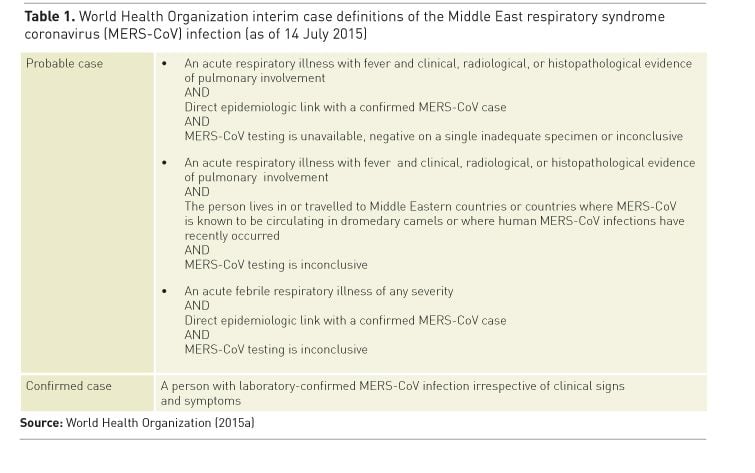
Early identification and diagnosis is critical in interrupting the chain of transmission in the healthcare setting. In order to facilitate early identification and prompt isolation, healthcare providers need to become aware of the MERS-CoV case definition and be promptly informed of any updates (see Table 1). Efficient triage systems, within the emergency department and ambulatory care areas, are needed for early identification of respiratory illness among patients. Once identified with pertinent risk factors healthcare staff need to be provided with proper protective equipment to prevent transmission. Once such patients are classified as suspected, probable or confirmed MERS CoV, proper patient placement according to hospital policy is needed.
When to Suspect MERS CoV
The disease should be suspected in patients with an acute febrile respiratory illness with clinical or radiologic evidence of pneumonia, who have a direct epidemiologic link with a confirmed MERS-CoV case, or live in or have travelled to a Middle Eastern country or countries where MERS-CoV is known to be circulating in dromedary camels or where human MERS-CoV infections have recently occurred. It is important to note that fever may not be present in up to 30% of cases on presentation (Alsolamy 2015).
The diagnosis is confirmed by rRT-PCR. Commonly tested samples are nasopharyngeal and throat swabs, sputum, tracheal aspirates and bronchoalveolar lavage. Lower respiratory tract specimens have a higher sensitivity than upper respiratory tract specimens for detecting MERS-CoV and are preferred (Lee et al. 2015). However, nasopharyngeal swabs have low yield compared to lower respiratory tract samples, and a negative rRT-PCR, even from lower respiratory samples, should not exclude the diagnosis in the presence of clinical suspension. Standardising the workup of patients presenting with lower respiratory tract infections is recommended.
Proper Use of Personal Protective Equipment while caring for MERS CoV
The Centers for Disease Control and Prevention (CDC) recommend that droplet precautions should be added to the standard precautions when providing care to all patients with symptoms of acute respiratory infection (National Center for Immunization and Respiratory Diseases (NCIRD), Division of Viral Diseases 2015), and that airborne precautions are applied for all suspected and confirmed MERSCoV cases or during aerosol-generating procedures. These precautions have been shown in the severe acute respiratory syndrome (SARS) epidemic to prevent transmission of infection to healthcare workers (Seto et al. 2003). On the other hand, the WHO recommends droplet and contact precautions (World Health Organization (WHO) 2015b). Airborne precautions should be additionally instituted when performing an aerosol-generating procedure (i.e., aspiration or open suctioning of the respiratory tract, intubation, bronchoscopy and cardiopulmonary resuscitation) (WHO 2015b).
It is recommended that healthcare providers, and in particular those exposed to patients with respiratory illness, including the ICU staff, should be fit tested for the proper respirator, preferably as part of an institutionally-based respiratory protection programme. Powered air-purifying respirators (PAPR) should be made available for staff who fail fit testing, and proper training for use and cleaning should be provided. An accurate record of individuals accessing rooms of suspected and confirmed MERS CoV cases needs to be established to assist proper contact tracing processes.
Additionally, staff should be trained on proper hand hygiene technique and PPE application, including how to don and doff personal protective equipment without self-contaminating. Their competency should be tested and documented. Policies to ensure 100% compliance with proper donning and doffing of personal protective equipment (PPE) should be in place. A buddy system, similar to what is recommended for monitoring healthcare workers’ (HCWs) compliance with PPEs while managing Ebola may be used. Housekeepers should also be trained in proper cleaning techniques and the use of PPE.
The implementation of such infection control measures requires having adequate stocks of PPE, such as respirators, goggles, face shields, gowns and scrub suits. During an outbreak, the consumption of PPE supply increases substantially and logistic plans should be in place to ensure constant supply.
Placement of Patients with Suspected and Confirmed MERS CoV Infection
The CDC recommends that a suspected or confirmed MERS CoV case should be isolated in an airborne infection isolation room that is constructed and maintained according to the current guidelines (National Center for Immunization and Respiratory Diseases, Division of Viral Diseases 2015). For example, the negative pressure room should have a minimum of six air changes per hour, with the air from these rooms exhausted directly to the outside or filtered through a high-efficiency particulate air (HEPA) filter before recirculation (National Center for Immunization and Respiratory Diseases, Division of Viral Diseases 2015). Until such placement, a facemask should be placed on the patient, who should be isolated in a room with the door kept closed (National Center for Immunization and Respiratory Diseases, Division of Viral Diseases 2015). If the housing ICU does not have an adequate number of such rooms, clinical engineering should have a plan to convert standard rooms to negative pressure rooms. Additionally, the proper negative pressure function of these rooms should be monitored and documented.
Cohorting of MERS patients in one ICU is recommended to facilitate care and monitoring. Other units should be identified prior to any increase in the number of cases beyond the capacity of the first unit. Transferring patients without MERS to other units or hospitals may be needed to increase bed capacity.
Medical Management of Patients with MERS-CoV Infection
To date, there are no clinical trials in humans for virus-specific therapies for MERS-CoV infection. Therefore, the medical management of patients is largely supportive. The WHO has issued interim guidance for the management of suspected and confirmed MERS-CoV infection (WHO 2015b). For patients with worsening hypoxaemia, early endotracheal intubation and mechanical ventilation using a lung-protective ventilation strategy are indicated (WHO 2015b). Early prone positioning and neuromuscular blockade may be considered in patients with moderate-to-severe acute respiratory distress syndrome (WHO 2015b). Systematic corticosteroids should probably be avoided unless there is another indication. Certain aerosol-generating procedures, such as high-flow oxygen and noninvasive ventilation, should be avoided or used with caution (WHO 2015b). A systematic review found the following procedures to be associated with an increased risk of respiratory pathogen transmission: endotracheal intubation, noninvasive ventilation, tracheotomy and manual ventilation (Tran et al. 2012).
Staffing
Care for these patients can be demanding. It is not unusual for the nurse-to-patient staffing ratio for MERS patients to increase to 2:1 nursing for some patients, similar to what has been described in the SARS epidemic (Hawryluck et al. 2005). ICU healthcare providers are frequently given additional tasks such as monitoring and correcting infection prevention practices of other healthcare workers. Infectious outbreaks in hospitals can lead to staff shortage due to the fear of working in a contagious setting, quarantine and illness (Hawryluck et al. 2005). Staff who develop fever, respiratory or gastrointestinal illness should be asked not to present to work, and to report to the emergency department or the employee health service depending on the severity of illness. Each institution should define the algorithm for managing staff exposure such as the required testing and isolation.
On the other hand, unnecessary exposure of healthcare workers to infected patients should be avoided, and limiting the number of medical and nursing staff caring for these patients is recommended.
Communication with Families
Family visits to patients with MERS-CoV infection should be restricted to a minimum. Family members with symptoms of acute respiratory illness should not be allowed to visit and should be tested for MERS-CoV. However, the treating intensivist should have a mechanism to communicate with the next of kin regularly, for example by phone.
Infectious Disease Emergency Preparedness Plan (IDEPP)
The ICU should be part of a hospital-wide infectious disease emergency preparedness plan (IDEPP). The
University of Texas at Brownsville has published an example of such a plan (2012), which provides the basic structure and guidance on how and by whom the different activities of the plan will be managed and coordinated. In addition the plan requires monitoring and assessment, to ensure all elements are in place. The IDEPP establishes a command centre that oversees all responses to the outbreak and is typically phased depending on the level of threat. For the ICU, plans for surge capacity should be described.
Conclusion
Prevention of healthcare-associated transmission should be a major focus of ICU preparedness to MERS-CoV. Early diagnosis and isolation of suspected cases, proper use of personal protective equipment, staff management, surge capacity for negative pressure rooms and integrating ICU plans with the hospital IPEPP are key elements of this response
See Also:
First-Ever Possible Treatments for MERS
Alsolamy S (2015) Middle East respiratory syndrome:
knowledge to date. Crit Care Med, 43(6): 1283-90.
Al-Tawfiq JA, Hinedi K, Ghandour J et al. (2014) Middle East
respiratory syndrome coronavirus: a case-control study of hospitalized
patients. Clin Infect Dis, 59(2): 160-5.
Assiri A, McGeer A, Perl TM et al. (2013) Hospital outbreak
of Middle East respiratory syndrome coronavirus. N Engl J Med, 369(5): 407-16.
Arabi YM, Arifi AA, Balkhy HH et al. (2014) Clinical course
and outcomes of critically ill patients with Middle East respiratory syndrome
coronavirus infection. Ann Intern Med, 160(6): 389-97.
Azhar EI, El-Kafrawy SA, Farraj SA et al. (2014) Evidence
for camel-to-human transmission of MERS coronavirus. N Engl J Med, 370(26):
2499-505.
Hawryluck L, Lapinsky SE, Stewart TE (2005) Clinical review:
SARS - lessons in disaster management. Crit Care, 9(4): 384-9.
Ki M (2015) 2015 MERS outbreak in Korea:
hospital-to-hospital transmission. Epidemiol Health, 37: e2015033.
Lee JH, Lee CS, Lee HB (2015) An Appropriate Lower
Respiratory Tract Specimen Is Essential for Diagnosis of Middle East
Respiratory Syndrome (MERS). J Korean Med Sci, 30(8): 1207-8.
Memish ZA, Assiri AM, Al-Tawfiq JA (2014) Middle East
respiratory syndrome coronavirus (MERS-CoV) viral shedding in the respiratory
tract: an observational analysis with infection control implications. Int J
Infect Dis, 29: 307-8.
Memish ZA, Zumla AI, Assiri A (2013) Middle East respiratory
syndrome coronavirus infections in health care workers. N Engl J Med, 369(9):
884-6.
National Center for Immunization and Respiratory Diseases
(NCIRD), Division of Viral Diseases (2015) Interim Infection Prevention and
Control Recommendations for Hospitalized Patients with Middle East Respiratory
Syndrome Coronavirus (MERS-CoV). [Accessed: 3 October 2015] Available from
cdc.gov/coronavirus/mers/infectionprevention-control.html
Oboho IK, Tomczyk SM, Al-Asmari AM et al. (2015) 2014
MERS-CoV outbreak in Jeddah-a link to health care facilities. N Engl J Med,
372(9): 846-54.
Saad M, Omrani AS, Baig K et al. (2014) Clinical aspects and
outcomes of 70 patients with Middle East respiratory syndrome coronavirus
infection: a single-center experience in Saudi Arabia. Int J Infect Dis, 29: 301-6.
Seto WH, Tsang D, Yung RW et al. (2003) Effectiveness of
precautions against droplets and contact in prevention of nosocomial
transmission of severe acute respiratory syndrome (SARS). Lancet, 361(9368):
1519-20.
Tran K, Cimon K, Severn M et al. (2012) Aerosol generating
procedures and risk of transmission of acute respiratory infections to
healthcare workers: a systematic review. PLoS One, 7(4): e35797.
The University of Texas at Brownsville (UTB) (2012)
Infectious Disease Emergency Preparedness Plan (IDEPP). [Accessed 3 October
2015] Available from www.utb.edu/ba/safety/Documents/IDEPP.pdf
van Doremalen N, Bushmaker T, Munster VJ (2013) Stability of
Middle East respiratory syndrome coronavirus (MERS-CoV) under different
environmental conditions. Euro Surveill, 18(38).
World Health Organization (WHO) (2015a) Middle East
respiratory syndrome coronavirus (MERSCoV). [Accessed: 3 October 2015]
Available from who.int/emergencies/mers-cov/en/
World Health Organization (WHO) (2015b) Clinical management
of severe acute respiratory infection when Middle East respiratory syndrome
coronavirus (MERS-CoV) infection is suspected—Interim guidance. [Accessed: 3
October 2015] Available from
who.int/csr/disease/coronavirus_infections/case-management-ipc/en/