ICU Management & Practice, Volume 21 - Issue 3, 2021
Introduction
Hypoxaemia is one of the most common complications during tracheal intubation of critically ill patients (Jaber et al. 2006; Russotto et al. 2021) with an incidence of severe hypoxaemia reaching up to 50% (De Jong et al. 2013; Jaber et al. 2006). Severe hypoxaemia can lead to cardiac arrest, neurologic damage, or multiple organ failure (De Jong et al. 2013; De Jong et al. 2018) and anticipating and avoiding such episodes is of critical importance to prevent the development of subsequent complications.
In order to reduce the occurrence of hypoxaemia, preoxygenation is mandatory before tracheal intubation, increasing the duration of apnoea before desaturation. Preoxygenation consists of increasing the pulmonary oxygen reserve, and thus the functional residual capacity (FRC), in order to prevent hypoxaemia that could occur during the intubation attempt. Obese patients, ICU patients and pregnant women are particularly at risk of reduced efficiency of preoxygenation due to certain pathophysiological changes: decreased FRC, increased risk of atelectasis, shunt.
However, the most common device used, a face mask, has to be taken off after preoxygenation in order to allow the passage of the orotracheal tube through the mouth. Furthermore, positioning the orotracheal tube in the trachea takes time, varying from a few seconds to several minutes in case of difficult intubation (De Jong et al. 2013).
High-flow nasal cannula oxygen therapy (HFNO) can be continued during the passage of the orotracheal tube through the mouth, and as a consequence may be used to continue blood oxygenation during the apnoea period of intubation, especially when the facial mask used for preoxygenation is removed (Papazian et al. 2016). All the same, the possible role of apnoeic oxygenation during intubation procedures in critically ill patients remains debated. When and how could it be used?
What is the Physiological Basis of Apnoeic Oxygenation?
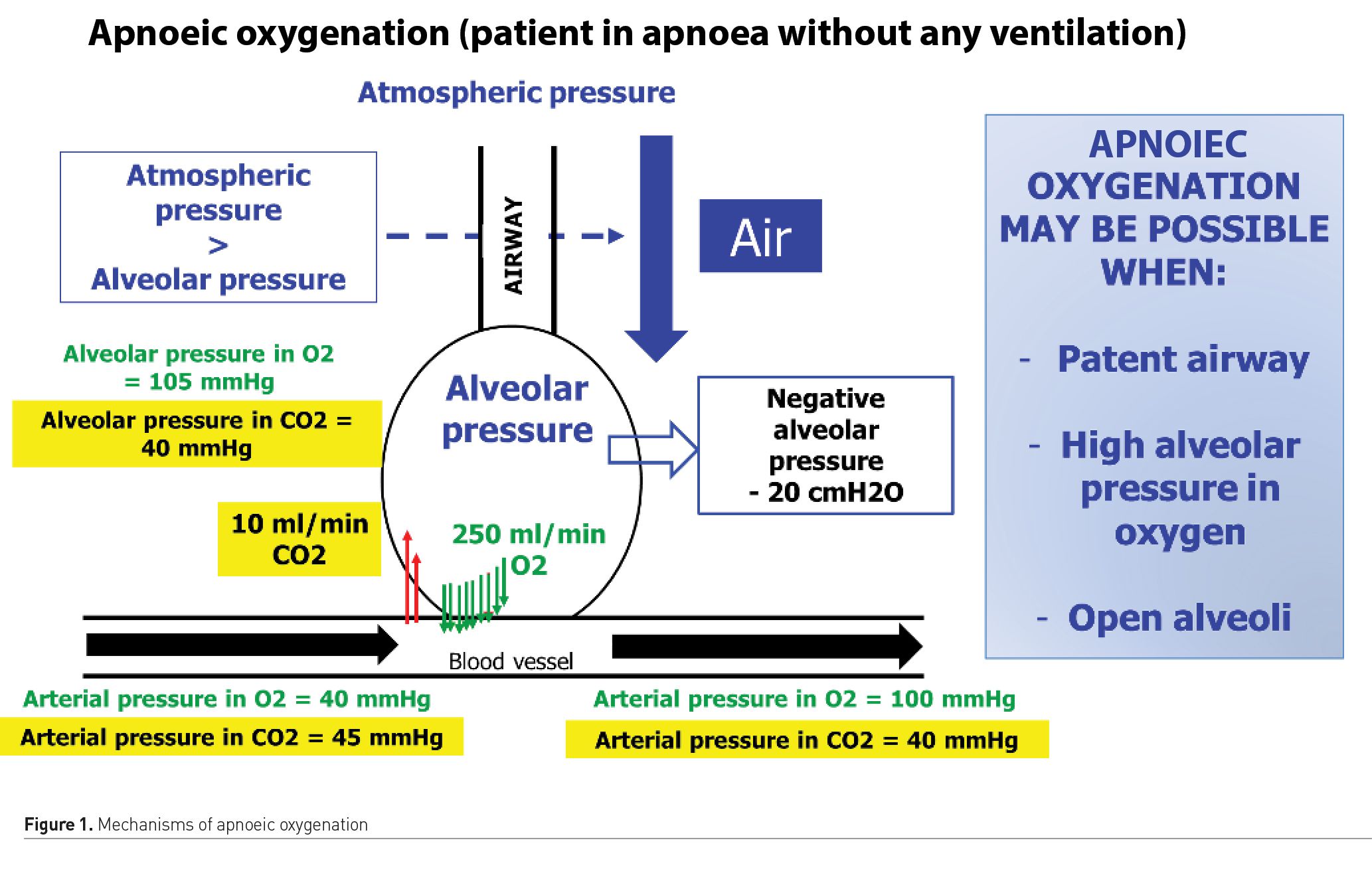
In 1959, a study reported eight patients scheduled for minor operations who were intubated and paralysed to prevent breathing (Frumin et al. 1959) but not ventilated. Pure oxygen was administered in the endotracheal tube. The patients drastically increased their carbon dioxide tension (up to 250 mm Hg) and developed respiratory acidosis (up to a pH of 6.72) while maintaining 100% oxygen saturation. Indeed, whereas carbon dioxide tension depends on minute ventilation, oxygenation depends on positive end-expiratory pressure (PEEP) and FIO2. Figure 1 summarises the course of oxygen from the atmosphere to the blood vessel during apnoea. Apnoeic oxygenation is a physiological phenomenon in which the difference between the alveolar rates of oxygen removal and carbon dioxide excretion generates a negative pressure gradient of up to 20 cmH2O. This negative pressure gradient can allow a flow of oxygen into the lungs, as long as airway permeability between the lungs and the atmosphere, open alveoli and high alveolar oxygen pressure are maintained (Figure 1).
What are the Most Recent Data Published?
Interpretation of the many existing trials in the field remains difficult because preoxygenation and apnoeic oxygenation are often evaluated concomitantly.
Guitton et al. (2019) included non-severely hypoxaemic patients, and found no significant difference between the median lowest SpO2 during intubation in the HFNO group compared with the standard bag valve mask group. However, there was less severe desaturation (<90%) in the HFNO group compared with the standard bag valve mask group. These results confirm the encouraging results of an observational study (Miguel-Montanes et al. 2015) performed, also in mildly hypoxaemic patients.
However, in severely hypoxaemic patients intubated in the intensive care unit (ICU), HFNO has never proved its efficiency, compared to absence of apnoeic oxygenation. Vourc'h et al. (2015) found no difference on the minimal SpO2 values during intubation in hypoxaemic patients between 60L/min of HFNO and oxygen facial mask (92% vs 90%, p=0.44). Semler et al. (2016) found that the administration of 15L/min nasal cannula oxygen in the apnoeic oxygenation group was not associated with significantly increased minimal SpO2 values during intubation procedures (from 92% in the apnoeic oxygenation group to 90% in the usual care group [p=0.16]).
The discrepancies between the results of these studies (Semler et al. 2016; Miguel-Montanes et al. 2015; Vourc'h et al. 2015; Sakles et al. 2016) could mainly be explained by the oxygen flow used for the apnoeic oxygenation group (from 15 to 60 L/min) and the different studied populations in term of hypoxaemia (severe vs mild to moderate). Moreover, if the efficiency of using HFNO for preoxygenation and apnoeic oxygenation is still a matter of debate (Chanques and Jaber 2019; Ricard and Gregoretti 2019; Hanouz et al. 2019a), it is mostly because preoxygenation (before induction of apnoea, when the patient is still breathing) is not separated from apnoeic oxygenation (after induction of apnoea, when the patient is not breathing anymore).
Preoxygenation using a tightly applied facial mask remains the method of choice. In a physiologic study (Hanouz et al. 2019b) comparing the ETO2 following preoxygenation, 96% and 46% (P < 0.001) of volunteers had an ETO2 of at least 90% in the face-mask and HFNO groups, respectively. In the face mask group, the hazard ratio to achieve an ETO2 of 90% was 5.3 (95% CI: 3.2 to 8.9; P < 0.001).
Noninvasive ventilation (NIV) preoxygenation of patients with severe hypoxaemic acute respiratory failure is associated with less hypoxaemia than preoxygenation with oxygen facial mask during intubation procedures (Baillard et al. 2006). Indeed, associating pressure support (PS) with positive end expiratory pressure (PEEP) limits alveolar collapse and atelectasis formation (Pepin et al. 2016; Hemmes et al. 2014), responsible for hypoventilation and low perfusion ventilation ratio (De Jong et al. 2014). Incidence of severe hypoxaemia defined by a pulse oximetry (SpO2) of less than 80% can be decreased by applying NIV preoxygenation, a method which is now used by many teams for preoxygenation of patients with severe hypoxaemic acute respiratory failure.
In a randomised controlled trial including 313 patients, NIV was recently compared to HFNO for preoxygenation of critically ill patients with acute hypoxaemic respiratory failure (Frat et al. 2019). Severe hypoxaemia (pulse oximetry < 80%) occurred in 33 (23%) of 142 patients after preoxygenation with NIV and 47 (27%) of 171 with HFNO (absolute difference –4.2%, 95% CI –13.7 to 5.5; p=0.39). In the subgroup of patients with PaO2/FiO2 lower than 200 mmHg, severe hypoxaemia occurred less frequently after preoxygenation with NIV than with HFNO (28 (24%) of 117 patients vs 44 (35%) of 125; adjusted odds ratio 0.56, 0.32 to 0.99, p=0.0459). Preoxygenation using NIV remains the most efficient way to decrease oxygen desaturation in critically ill patients, and furthermore in the obese patient (Schetz et al. 2019).
Using HFNC combined with NIV may have potential advantages over conventional NIV alone for preoxygenation before intubation procedures in hypoxaemic ICU patients.The OPTINIV method (Figure 2) (Jaber et al. 2016), associating preoxygenation with pressure support and PEEP (NIV) and HFNO for both preoxygenation and apnoeic oxygenation, allowed a significantly higher oxygen saturation during the intubation procedure, when compared to preoxygenation with NIV alone.
What To Do in Practice?
Several preoxygenation methods are available in practice: bag valve mask, HFNO, pressure support associated with PEP (NIV), OPTINIV method (NIV combined to HFNO).
Three methods provide sufficient reserves in oxygen: bag valve mask oxygenation, NIV, OPTINIV method, the latter permitting higher oxygen saturation during intubation procedures in severely hypoxaemic patients. HFNO can be added for apnoeic oxygenation in case of high risk of desaturation, ensuring good mandible subluxation, after an attempt to open alveoli using NIV (Figure 1).
One very efficient way to oxygenate during the apnoea period remains to ventilate the patient. The efficiency of ventilation during apnoea after rapid sequence induction was recently assessed (Casey et al. 2019). Among critically ill adults undergoing tracheal intubation, patients receiving bag valve mask ventilation had higher oxygen saturations and a lower incidence of severe hypoxaemia than those receiving no ventilation. In very hypoxaemic critically ill patients, without high risk of aspiration, considering bag valve mask ventilation may help to limit the rapid drop in oxygen saturation.
Conclusion
To date, the evidence for apnoeic oxygenation being beneficial during ICU intubation is conflicting, most likely because its success depends on upper airway patency during laryngoscopy and intubation, as well as the FiO2, oxygen flow rate, patient position and the extent and cause of any pre-existing hypoxaemia. There is little or no evidence of harm. However, the clinician must avoid confusion between preoxygenation and apnoeic oxygenation. Whereas NIV is the method of preference for preoxygenation of critically ill hypoxaemic patients, HFNO can be used for apnoeic oxygenation, and might limit the occurrence of desaturation especially in mild to moderately hypoxaemic patients. The OPTNIV method, combining NIV and HFNO, is the method of choice to increase the lowest oxygen saturation reached during the intubation procedure. In patients at high risk of desaturation and without high risk of aspiration, preventive ventilation during apnoea should be considered.
Conflict of interest
Dr De Jong reports receiving consulting fees from Medtronic. Pr. Jaber reports receiving consulting fees from Drager, Medtronic, Baxter, Fresenius-Xenios, and Fisher & Paykel. Dr Monet has no conflict of interest.
References:
Baillard C, Fosse J, Sebbane M et al. (2006) Noninvasive Ventilation Improves Preoxygenation Before Intubation of Hypoxic Patients. Am J Respir Crit Care Med, 174:171-7.
Casey JD, Janz DR, Russell DW et al. (2019) Bag-Mask Ventilation During Tracheal Intubation of Critically Ill Adults. N Engl J Med, 380, 811-821.
Chanques G, Jaber S (2019) Nasal High-Flow Preoxygenation for Endotracheal Intubation in the Critically Ill Patient? Maybe. Intensive Care Med, 45:532-534.
De Jong A, Futier E, Millot A et al. (2014) How to Preoxygenate in Operative Room: Healthy Subjects and Situations "At Risk". Annales Françaises D'anesthèsie Et De Rèanimation, 33:457-61.
De Jong A, Molinari N, Terzi N et al. (2013) Early Identification of Patients at Risk for Difficult Intubation in the Intensive Care Unit: Development and Validation of the Macocha Score in a multicenter cohort study. Am J Respir Crit Care Med, 187:832-9.
De Jong A, Rolle A, Molinari N et al. (2018) Cardiac Arrest and Mortality Related to Intubation Procedure in Critically Ill Adult Patients: A Multicenter Cohort Study. Crit Care Med, 46:532-539.
Frat JP, Ricard JD, Quenot JP et al. (2019) Non-Invasive Ventilation versus High-Flow Nasal Cannula Oxygen Therapy with Apnoeic Oxygenation for Preoxygenation Before Intubation of Patients with Acute Hypoxaemic Respiratory Failure: A Randomised, Multicentre, Open-Label Trial. Lancet Respir Med, 7:303-312.
Frumin MJ, Epstein RM, Cohen G (1959) Apneic Oxygenation in Man. Anesthesiology, 20: 789-98.
Guitton C, Ehrmann S, Volteau C et al. (2019) Nasal High-Flow Preoxygenation for Endotracheal Intubation in the Critically Ill Patient: A Randomized Clinical Trial. Intensive Care Med, 45:447-458.
Hanouz JL, Gerard JL, Fischer MO (2019a) Nasal High-Flow Preoxygenation for Endotracheal Intubation in the Critically Ill Patient? Con. Intensive Care Med, 45:526-528.
Hanouz JL, L hermitte D, Gerard JL et al. (2019b) Comparison of Pre-Oxygenation Using Spontaneous Breathing Through Face Mask and High-Flow Nasal Oxygen: A Randomised Controlled Crossover Study in Healthy Volunteers. Eur J Anaesthesiol, 36:335-341.
Hemmes SN, Gama De Abreu M, Pelosi P et al. (2014) High Versus Low Positive End-Expiratory Pressure During General Anaesthesia for Open Abdominal Surgery (Provhilo Trial): A Multicentre Randomised Controlled Trial. Lancet, 384:495-503.
Jaber S, Amraoui J, Lefrant JY et al. (2006) Clinical Practice and Risk Factors for Immediate Complications of Endotracheal Intubation in the Intensive Care Unit: A Prospective, Multiple-Center Study. Critical Care Medicine, 34:2355-2361.
Jaber S, Monnin M, Girard M et al. (2016) Apnoeic Oxygenation via High-Flow Nasal Cannula Oxygen Combined with Non-Invasive Ventilation Preoxygenation for Intubation in Hypoxaemic Patients in the Intensive Care Unit: The Single-Centre, Blinded, Randomised Controlled Optiniv Trial. Intensive Care Med, 42:1877-1887.
Miguel-Montanes R, Hajage D, Messika J et al. (2015) Use Of High-Flow Nasal Cannula Oxygen Therapy to Prevent Desaturation During Tracheal Intubation of Intensive Care Patients with Mild-To-Moderate Hypoxemia. Crit Care Med, 43:574-83.
Papazian L, Corley A, Hess D et al. (2016) Use Of High-Flow Nasal Cannula Oxygenation in ICU Adults: A Narrative Review. Intensive Care Medicine.
Pepin JL, Timsit JF, Tamisier R et al. (2016) Prevention and Care of Respiratory Failure in Obese Patients. Lancet Respir Med, 4, 407-18.
Ricard JD, Gregoretti C (2019) Nasal High-Flow Preoxygenation for Endotracheal Intubation in the Critically Ill Patient? Pro. Intensive Care Med, 45:529-531.
Russotto V, Myatra SN, Laffey JG et al. (2021) Intubation Practices and Adverse Peri-Intubation Events in Critically Ill Patients from 29 Countries. JAMA, 325:1164-1172.
Sakles JC, Mosier JM, Patanwala AE et al. (2016) Apneic Oxygenation is Associated with a Reduction in the Incidence O=off Hypoxemia During the RSI of Patients With Intracranial Hemorrhage in the Emergency Department. Intern Emerg Med.
Schetz M, De Jong A, Deane AM et al. (2019) Obesity in the Critically Ill: A Narrative Review. Intensive Care Med, 45:757-769.
Semler MW, Janz DR, Lentz RJ et al. (2016) Randomized Trial of Apneic Oxygenation During Endotracheal Intubation of the Critically Ill. Am J Respir Crit Care Med, 193: 273-80.
Vourc'h M, Asfar P, Volteau C et al. (2015) High-Flow Nasal Cannula Oxygen During Endotracheal Intubation in Hypoxemic Patients: A Randomized Controlled Clinical Trial. Intensive Care Medicine, 41:1538-48.






















