HealthManagement, Volume 17 - Issue 1, 2017
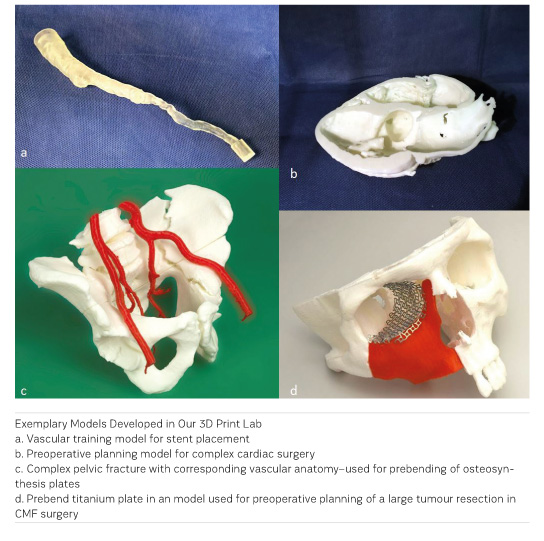
3D printing will most likely transform the medical field as it presents a multitude of new opportunities from visualisation of complex anatomy, building training models or templates for challenging procedures to patient-specific implants. A variety of disciplines work with 3D printing and various regular use cases have been identified. Since the late 1980s, craniomaxillofacial (CMF) surgeons have been using 3D printed anatomical models to visualise and facilitate the treatment of complex facial pathologies. With the advent of consumer-grade 3D printers that can be bought for less than €2000, many hospitals are starting to investigate this emerging field.
At our 3D print lab, this is most often a CT study, in fewer cases an MR sequence or cone beam volume CT. Some authors also report success in printing 3D ultrasound data. Further on, the technical requirements for 3D printing include, besides the aforementioned printer, segmentation software which turns the image dataset into a three-dimensional model that the printer software can read. This can often be done with common radiological visualisation suites or commercially available medical segmentation and planning tools. There is also open source and freeware software available online. This process of image transformation from two-dimensional images to virtual 3D objects—called segmentation—identifies the structures of interest comprising the final model. Segmentation can be done automatically, semi-automatically (for example by region growing algorithms) or manually. Depending on the structure of interest, this process can be quite easy when there is high contrast between objects (eg, bone surrounded by muscle in a CT scan) or it can be quite difficult (eg, differentiation of white and grey matter on a brain CT scan). Therefore, it is advisable to select the imaging modalities best suited to depict the structure of interest, eg, contrast media application for the segmentation of vessels. When the desired structure is segmented, it is exported as a STL file (stereolithography), which is subsequently converted by the printer control software into the specific movements of the printing head. Alternatively, the model can be sent to an external 3D printing service provider.
But where would you place the 3D lab within the complex infrastructure of today’s hospitals? When we started inquiring about 3D printing within our hospital, we found a highly variable degree of involvement. Some disciplines had heard about it, some already worked with it, while others did not see any need for 3D printing. Consequently, we decided to form a partnership between two disciplines that had already gathered substantial 3D printing knowledge.
This—to our knowledge—unique approach in forming the 3D lab as a joint operation by radiologists and CMF surgeons allows us to tap into the knowledge of these core disciplines for 3D printing: the advanced 3D printing knowledge of CMF surgery in the surgical context as well as the radiologists’ knowledge about the acquisition of imaging datasets and experience in imaging and image postprocessing.
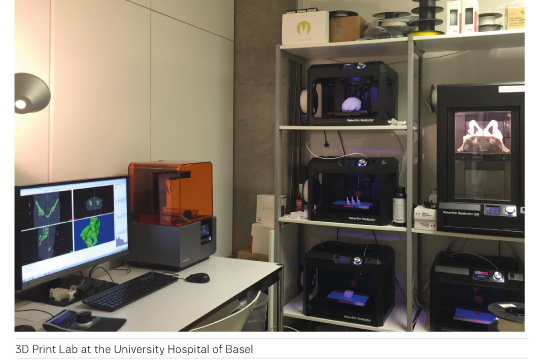
At our hospital, the 3D print lab is located in the department of radiology. Radiology is at the intersection of many disciplines: it is usually the place where most colleagues turn to for “all things regarding visualisation” and was among the first fully digitised disciplines. We then established a simple online order entry workflow for new 3D print jobs out of the clinical information system, which gets transferred to a common email inbox. Depending on the kind of print job, the referring department and the schedule, the printing job is then managed by either the radiologist, the CMF surgeon or, in complex cases, in a joint effort. Additionally, we formed a partnership with the University of Applied Sciences North-western Switzerland that can provide the biomedical engineering know-how when needed. A cloud-based solution addressing all 10 fused filament moulding (FFM) printers allows uploading and submission of the final 3D model from within the hospital or remotely from outside while simultaneously assisting in monitoring the print jobs. For ultra high-resolution prints and printing of bio-compatible materials, such as surgical guides, our 3D printing lab offers a stereolithography (SLA) printer.
The benefit of this collaboration has been immediately evident since the inauguration of our 3D print lab in June 2016. We have seen a steady increase in 3D planning cases and prints—more than 250 3D models in 6 months—with many referring physicians providing positive feedback about the impact of the 3D prints on their practice. To date, we have been working with more than ten different medical disciplines and the number of requests keeps rising. As another benefit, the installation of the 3D lab brings the radiologist closer to the clinician, which improves the understanding of our colleagues’ expectations and needs. The 3D printing lab is an enriching set-up for both the clinicians and the radiologists.
Key Points
- 3D printing will transform the medical field as it
provides many new opportunities for visualisation, training and creating templates
- The threshold for 3D printing is low: post processing
freeware and an entry-level printer are all that’s needed to get started
- In our hospital, the 3D printing cooperation between
craniomaxillofacial (CMF) surgeons and radiologists turned out to be especially
fruitful since their expertise was complementary for creating a 3D printing lab
in-house, offering fast preparation of models, improved collaboration and increasing
interest from clinicians
Philipp Brantner, MD, is an attending at the Clinic of Radiology and Nuclear Medicine at the University Hospital of Basel. In addition to completing a cardio-thoracic fellowship he is the department specialist for 3D printing and is the co-leader of the university hospital’s 3D print lab.
References:
Mitsouras D, Liacouras P, Imanzadeh A et al. (2015) Medical 3D printing for the radiologist. Radiographics, 35(7): 1965–88.
Matsumoto JS et al. (2015) Three-dimensional physical modeling: applications and experience at Mayo Clinic. Radiographics, 35(7): 1989–2006.


















