HealthManagement, Volume 3 - Issue 1, 2009
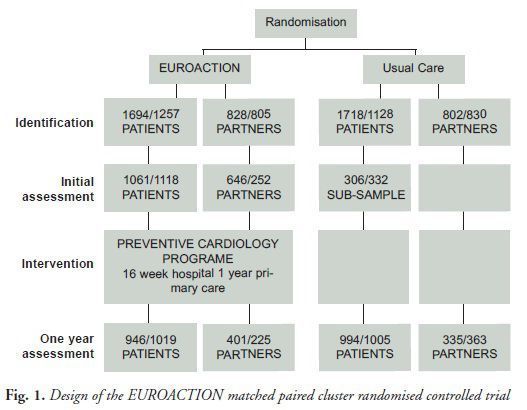
EUROACTION, a demonstration project in preventive cardiology, was launched in 2003 in eight European countries (Denmark, France, Italy, the Netherlands, Poland, Spain, Sweden and the UK). Using a matched paired cluster randomised controlled trial study design (see Fig. 1), it aimed to show that nurse-led care could facilitate the implementation of European and national guidelines for CVD prevention in everyday clinical practice. It was set up in 12 district general hospitals and 12 general practices, half of which were randomly assigned to receive the EUROACTION preventive cardiology programme and half which were monitored for the usual care they provided.
In hospitals, the study prospectively identified all consecutive patients presenting for the first time with acute coronary disease (acute myocardial infarction or unstable angina) or exertional angina as inpatients or outpatients in each centre.
In general practice, patients were opportunistically identified by their general practitioners at high total risk of developing cardiovascular disease (CVD) as calculated using the European heart score risk estimation tool (≥ 5% risk of dying from CVD over the next ten years), or currently under treatment with blood pressure and/or lipid lowering therapies and/or diagnosed with diabetes.
The primary one year endpoints were family-based lifestyle changes (not smoking, adoption of a cardio-protective diet, increased physical activity), reduced body weight and in particular central obesity, management of blood pressure, lipids, and blood glucose concentrations to target, and prescription of cardio-protective drugs. Analysis was by intention to treat.
Cardiovascular Specialist Nurses as Managers
Cardiovascular specialist nurses were employed to manage dedicated multidisciplinary teams. Nurses were responsible for the delivery of the smoking cessation intervention, dieticians for dietary and weight management intervention, and physiotherapists for physical activity intervention. Cardiologists were available to advice on symptom and risk factor management with medications. The nurse in general practice was trained to deliver a comprehensive lifestyle and risk factor programme with the support of physicians.
The hospital team worked together, sharing the same office space to manage patients and their family members attending the programme. The programme had certain key elements:
- Proactive identification of all eligible patients;
- Invitation to both patients and their partners (and first degree relatives where appropriate) to join the programme;
- A comprehensive multidisciplinary assessment of both the patient and their partner of all aspects of lifestyle risk factors, cardio-protective medications, health-related quality of life, health beliefs, illness and risk perception;
- Goal setting in negotiation with both patient and partner;
- A professional lifestyle management programme for smoking cessation, healthy eating, promoting physical activity and achieving a healthy weight and shape;
- Protocol management of blood pressure, lipids and glucose by the nurse working with physicians to achieve treatment targets;
- Prescription and up-titration of cardio protective medications by cardiologist general practitioner;
- Weekly attendance of the programme over 16 weeks;
- Regular multidisciplinary meetings of the core team with the cardiologist general practitioner to discuss progress and update the plan of care, recorded in the medical notes to be addressed at the next programme attendance;
- Hospital team/general practice nurse to follow up each family when they attend the programme to agree lifestyle plan and to give prescriptions;
- Weekly supervised exercise sessions, and
- Group health promotion workshops.
Why Nurses to Coordinate?
Each programme employed a full-time specialist nurse to coordinate the multidisciplinary team and to facilitate programme delivery. Nurses were chosen for this role for the following reasons:
- Nurse training and bachelor degree programmes incorporate the medical, biological, social and behavioural sciences as well as health psychology. In addition, they have the opportunity to learn counselling and teaching skills.
- Nurses are accustomed to working closely with the medical profession and to implementing medical decisions about care.
- They are trained to understand symptoms and monitor patients’ signs, e.g. blood pressure.
- They can cope with patients’ emotional problems (e.g. fear or denial).
- They are trained to safely administer medicines, are familiar with medications, doses, potential interactions, etc.
- They follow professional recommendations and protocols well.
- Training also includes management theory. In their professional role, nurses have to coordinate nursing teams on the hospital ward and other disciplines, e.g. physiotherapists, pharmacists, etc.
However, nurses must access adequate training for these extended
roles, know their capabilities and accept their limitations and understand when
it is appropriate to refer to other disciplines or seek the advice of doctors.
What did the Approach Achieve?
1,589 and 1,499 patients with CHD in the hospital study and 1,189
and 1,128 at high risk of developing CVD were recruited to intervention and
usual care centres respectively. The analyses were based on intention to treat
using random effects modelling so as to take account of a cluster randomised
controlled design. Tables 1 and 2 show
the principal results reported at one year.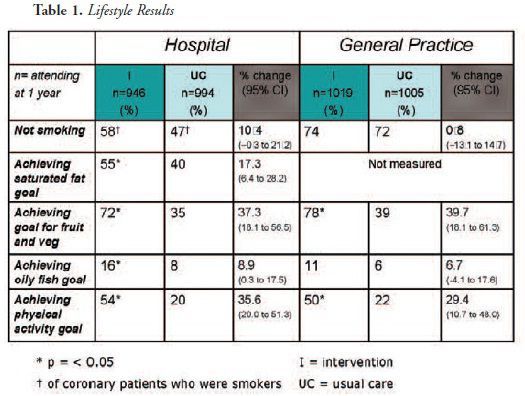
In the physical activity results, half or more of both coronary and high-risk patients in the intervention groups reported achieving the physical activity goal of at least 30 minutes of moderate intensity activity on at least five days of the week compared to less than a quarter in usual care. Also encouraging were the dietary results with significantly more coronary patients in the intervention group compared to usual care achieving the low saturated fat target, the high consumption of fruit and vegetable target and the oily fish target.
In the EUROACTION study, most coronary patients who smoked at the time of their event had stopped by the time of the initial assessment. Therefore the challenge for nurses was to prevent relapse in this group in the programme. 58% in the intervention group compared to 47% in the usual care group were not smoking (validated by breath carbon monoxide) at one year. Although of borderline statistical significance (p=0.06), this absolute difference of 10% less smoking relapse is clinically important. Amongst high-risk individuals in general practice, despite more quit attempts being made in the intervention group, the proportions not smoking at one year were no different from usual care. This was probably due to a very low use of pharma therapies to aid smoking cessation.
The successful changes reported in the dietary and physical
activity results were reflected in the results for risk factor management, i.e.
for overweight and obesity, blood pressure, lipids and glucose (see table 2).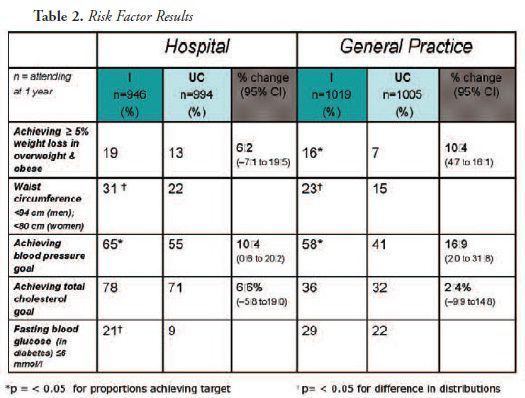
Body weight was measured in terms of body mass index, overall
weight reduction and weight distribution (central obesity). The initial goal
for weight loss in the overweight and obese was 5 - 10% of total body weight.
The EUROACTION nurses helped significantly more patients to achieve this goal
than in usual care.
Blood Pressure & Cholesterol Goals
The nurse-led programme was more successful than usual care in helping patients attain the blood pressure goal of less than 140/90 mm Hg. This was achieved in coronary patients despite no difference in the prescription of blood pressure lowering therapies between intervention and usual care. It is probably attributable to the delivery of a professional lifestyle intervention and better compliance with prescribed medication.
Achievement of the total cholesterol target of less than 5 mmol/L was high in both intervention and usual care hospital patients despite significantly more prescribing of statins in the intervention centres: 86% compared to 80%. In those at high risk in general practice, a larger proportion of patients in the usual care centres started off at goal for lipids compared to intervention. However, the difference in change from baseline to one year in achieving target was 12.7% in favour of the intervention group.
The EUROACTION nurses were required to screen for diabetes and
impaired glucose regulation and manage blood glucose and blood pressure to the
lower target of 130/85mmHg. With regard to blood glucose control in patients
with diabetes at one year, the distributions of blood glucose between the
intervention and usual care groups in coronary patients were significantly
different and in favour of intervention. Blood pressure management was
significantly better in diabetic patients in general practice with 39% of
patients in the intervention group achieving the goal of 130/85mmHg compared to
only 19% in usual care: an 18.8% difference.
Challenges of Leading a Multidisciplinary Team
Professional Standing of Nurses
Demonstrating effectiveness of a leadership role for nurses was not without difficulties. Nurses have differing professional standing across European countries. Nurse coordinated care may, therefore, not be applicable to all health cultures and may be dependent upon training provision for expanding roles and physician/nurse ratios in a particular country.
Successful Multidisciplinary Teamwork
Another challenge was to ensure good team cohesion. The success of the preventive cardiology programme in hospital, where a dedicated multidisciplinary team was put in place, depended to a large extent on the dynamics of the working relationships within the team. Coordinating a team of expert professionals to run a programme is a challenge that demands respect for knowledge and skills. However, it requires leadership qualities that can direct and keep the team together despite individual differences. The nurses coordinating each one of these EUROACTION programmes were expected to have these qualities.
Challenging Traditional Models and Roles
Communication to health professionals of the success of EUROACTION
has been seen as a threat to some. This presented a steep learning curve for
all concerned, not least the EUROACTION central team, to understand
sensitivities, and also to understand that for some health economies, a nurse
coordinated model of care, rather than a doctor led model of care has not yet
reached its time.
Conclusion
EUROACTION has shown that standards of preventive care in general hospitals and general practices across Europe can be improved. This nurse coordinated, multidisciplinary, family-based, ambulatory programme achieved healthier lifestyle changes and improvements in other risk factors for patients with coronary heart disease and those at high risk of cardiovascular disease and their partners than those in usual care. For more information about EUROACTION please visit www.escardio.org/euroaction



















